Abstract
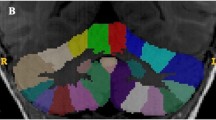
Cerebellar volume, in particular vermal lobule areas VI–VII, have been extensively researched in individuals with autism spectrum disorder (ASD), although findings are often unclear. The aim of the present study is to consolidate all existing cerebellar and age data of individuals with ASD, and compare this data to typically developing (TD) controls. Raw data, or the means and standard deviations of cerebellar volume and age, were obtained from 17 studies (NCerebellum: 421 ASD and 370 TD participants; NVI–VII: 506 ASD and 290 TD participants). Total cerebellar volume, or VI–VII area, was plotted against age and lines of fit of ASD and TD data were compared. Mean differences in cerebellar volume and VI–VII area between participants with ASD and TD participants were then compared via ANCOVA analyses. Findings revealed multiple differences in VI–VII area between participants with ASD and TD participants below 18 years of age. Additionally, cerebellar volume was greater in males with ASD than TD males between 2 and 4 years. In the present study, cerebellar volume and VI–VII area show different rates of change across age for those with autism compared with those without. These morphological differences provide a neurobiological justification to investigate related behavioural correlates.


Similar content being viewed by others
References
Bourgeron T. A synaptic trek to autism. Curr Opin Neurobiol. 2009;19(2):231–4.
Amaral DG, Li D, Libero L, Solomon M, Van de Water J, Mastergeorge A, et al. In pursuit of neurophenotypes: the consequences of having autism and a big brain. Autism Res. 2017;10(5):711–22.
Verhoeff B. Fundamental challenges for autism research: the science–practice gap, demarcating autism and the unsuccessful search for the neurobiological basis of autism. Med Health Care Philos. 2015;18(3):443–7.
Traut N, Beggiato A, Bourgeron T, Delorme R, Rondi-Reig L, Paradis A-L, et al. Cerebellar volume in autism: literature meta-analysis and analysis of the autism brain imaging data exchange cohort. Biol Psychiatry. 2018;83(7):579–88.
Sacco R, Gabriele S, Persico AM. Head circumference and brain size in autism spectrum disorder: a systematic review and meta-analysis. Psychiatry Res. 2015;234(2):239–51.
Webb SJ, Sparks BF, Friedman SD, Shaw DW, Giedd J, Dawson G, et al. Cerebellar vermal volumes and behavioral correlates in children with autism spectrum disorder. Psychiatry Res. 2009;172(1):61–7.
Cleavinger HB, Bgler ED, Johnson JL, Lu J, McMahon W, Lainhart JE. Quantitative magnetic resonance image analysis of the cerebellum in macrocephalic and normocephalic children and adults with autism. J Int Neuropsychol Soc. 2008;14(3):401–13.
Courchesne E, Karns CM, Davis HR, Ziccardi R, Carper RA, Tigue ZD, et al. Unusual brain growth patterns in early life in patients with autistic disorder: an mri study. Neurology. 2001;57(2):245–54.
Hanaie R, Mohri I, Kagitani-Shimono K, Tachibana M, Matsuzaki J, Watanabe Y, et al. Abnormal corpus callosum connectivity, socio-communicative deficits, and motor deficits in children with autism spectrum disorder: a diffusion tensor imaging study. J Autism Dev Disord. 2014;44(9):2209–20.
Hazlett HC, Poe M, Gerig G, Smith RG, Provenzale J, Ross A, et al. Magnetic resonance imaging and head circumference study of brain size in autism: birth through age 2 years. Arch Gen Psychiatry. 2005;62(12):1366–76.
Hodge S, Makris N, Kennedy D, Caviness VS Jr, Howard J, McGrath L, et al. Cerebellum, language, and cognition in autism and specific language impairment. J Autism Dev Disord. 2010;40(3):300–16.
Piven J, Saliba K, Bailey J, Arndt S. An mri study of autism: the cerebellum revisited. Neurology. 1997;49(2):546–51.
Scott JA, Schumann CM, Goodlin-Jones BL, Amaral DG. A comprehensive volumetric analysis of the cerebellum in children and adolescents with autism spectrum disorder. Autism Res. 2009;2(5):246–57.
Hallahan B, Daly EM, McAlonan G, Loth E, Toal F, O’Brien F, et al. Brain morphometry volume in autistic spectrum disorder: a magnetic resonance imaging study of adults. Psychol Med. 2009;39(2):337–46.
Koziol LF, Budding D, Andreasen N, D’Arrigo S, Bulgheroni S, Imamizu H, Ito M, Manto M, Marvel C, Parker KJTC. 2014. Consensus paper: the cerebellum’s role in movement and cognition. 13(1):151-177.
Stoodley CJ. The cerebellum and neurodevelopmental disorders. Cerebellum. 2016;15(1):34–7.
Hannant P, Tavassoli T, Cassidy S. The role of sensorimotor difficulties in autism spectrum conditions. Front Neurol. 2016;7:124.
Patriquin MA, DeRamus T, Libero LE, Laird A, Kana RK. Neuroanatomical and neurofunctional markers of social cognition in autism spectrum disorder. Hum Brain Mapp. 2016;37(11):3957–78.
Kaufmann WE, Cooper KL, Mostofsky SH, Capone GT, Kates WR, Newschaffer CJ, et al. Specificity of cerebellar vermian abnormalities in autism: a quantitative magnetic resonance imaging study. J Child Neurol. 2003;18(7):463–70.
Sparks BF, Friedman SD, Shaw DW, Aylward EH, Echelard D, Artru AA, et al. Brain structural abnormalities in young children with autism spectrum disorder. Neurology. 2002;59(2):184–92.
Retico A, Giuliano A, Tancredi R, Cosenza A, Apicella F, Narzisi A, et al. The effect of gender on the neuroanatomy of children with autism spectrum disorders: a support vector machine case-control study. Mol Autism. 2016;7(1):5.
Tepest R, Jacobi E, Gawronski A, Krug B, Moller-Hartmann W, Lehnhardt FG, et al. Corpus callosum size in adults with high-functioning autism and the relevance of gender. Psychiatry Res. 2010;183(1):38–43.
Libero LE, Nordahl CW, Li DD, Ferrer E, Rogers SJ, Amaral DG. Persistence of megalencephaly in a subgroup of young boys with autism spectrum disorder. Autism Res. 2016;9(11):1169–82.
Tummers B, van der Laan J, Huyser K. (2006) Datathief iii. 1.6 ed
Courchesne E, Yeung-Courchesne R, Hesselink JR, Jernigan TL. Hypoplasia of cerebellar vermal lobules vi and vii in autism. N Engl J Med. 1988;318(21):1349–54.
Hashimoto T, Tayama M, Murakawa K, Yoshimoto T, Miyazaki M, Harada M, et al. Development of the brainstem and cerebellum in autistic patients. J Autism Dev Disord. 1995;25(1):1–18.
Steinman KJ, Mostofsky SH, Denckla MB. Toward a narrower, more pragmatic view of developmental dyspraxia. J Child Neurol. 2010;25(1):71–81.
Crucitti J, Hyde C, Stokes MA. Hammering that nail: varied praxis motor skills in younger autistic children. J Autism Dev Disord. 2019:1–10. https://doi.org/10.1007/s10803-019-04136-4.
Mostofsky SH, Dubey P, Jerath VK, Jansiewicz EM, Goldberg MC, Denckla MB. Developmental dyspraxia is not limited to imitation in children with autism spectrum disorders. J Int Neuropsychol Soc. 2006;12(3):314–26.
Dowell LR, Mahone EM, Mostofsky SH. Associations of postural knowledge and basic motor skill with dyspraxia in autism: implication for abnormalities in distributed connectivity and motor learning. Neuropsychology. 2009;23(5):563–70.
Wang SSH, Kloth AD, Badura A. The cerebellum, sensitive periods, and autism. Neuron. 2014;83(3):518–32.
Bailey A, Luthert P, Dean A, Harding B, Janota I, Montgomery M, et al. A clinicopathological study of autism. Brain J Neurol. 1998;121(5):889–905.
Fatemi SH, Halt AR, Realmuto G, Earle J, Kist DA, Thuras P, et al. Purkinje cell size is reduced in cerebellum of patients with autism. Cell Mol Neurobiol. 2002;22(2):171–5.
Whitney ER, Kemper TL, Rosene DL, Bauman ML, Blatt GJ. Density of cerebellar basket and stellate cells in autism: evidence for a late developmental loss of purkinje cells. J Neurosci Res. 2009;87(10):2245–54.
Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol. 2005;57(1):67–81.
Cavanagh J, Krishnadas R, Batty GD, Burns H, Deans KA, Ford I, et al. Socioeconomic status and the cerebellar grey matter volume. Data from a well-characterised population sample. Cerebellum. 2013;12(6):882–91.
Lai M-C, Lombardo MV, Ruigrok ANV, Chakrabarti B, Auyeung B, Szatmari P, et al. Quantifying and exploring camouflaging in men and women with autism. Autism. 2017;21(6):690–702.
He W, Goodkind D, Kowal PR. An aging world: 2015. Washington, DC: United States Census Bureau; 2016.
Ciesielski KT, Harris RJ, Hart BL, Pabst HF. Cerebellar hypoplasia and frontal lobe cognitive deficits in disorders of early childhood. Neuropsychologia. 1997;35(5):643–55.
Hardan AY, Minshew NJ, Harenski, K, Keshavan, MS. Posterior Fossa Magnetic Resonance Imaging in Autism. J Am Acad Child Psy. 2001;40(6):666–72.
Minshew NJ. Autism. In: Berg, BO. Principles of child neurology. New York: McGraw-Hill; 1996:1713–30.
Palmen SJMC, Hulshoff Pol HE, Kemner C, Schnack HG, Janssen J, Kahn RS, et al. Larger brains in medication naive high-functioning subjects with pervasive developmental disorder. J Autism Dev Disord. 2004;34(6):603–13.
Palmen SJMC, Hulshoff Pol HE, Kemner C, Schnack HG, Durston S, Lahuis BE, et al. Increased gray-matter volume in medication-naive high-functioning children with autism spectrum disorder. Psychol Med. 2005;35(4):561–70.
Piven J, Nehme E, Simon J, Barta P, Pearlson G, Folstein SE. Magnetic resonance imaging in autism: measurement of the cerebellum, pons, and fourth ventricle. Biol Psychiatry. 1992;31(5):491–504.
Zeegers M, Hulshoff Pol H, Durston S, Nederveen H, Schnack H, van Daalen E, et al. No differences in MR-based volumetry between 2- and 7-year-old children with autism spectrum disorder and developmental delay. Brain Dev. 2009;31(10):725–30.
Crucitti J, Hyde C, Enticott, PG, Stokes MA. Head circumference trends in autism: 0 to 100 months. Autism. in-press.
Acknowledgements
We would like to thank the authors whom made data available to be included in the present study.
Data Access
Data access can be obtained by contacting the corresponding author via email. Data will be provided in all reasonable requests.
Funding
Peter Enticott is supported by a Future Fellowship from the Australian Research Council (FT160100077).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Crucitti, J., Hyde, C., Enticott, P.G. et al. Are Vermal Lobules VI–VII Smaller in Autism Spectrum Disorder?. Cerebellum 19, 617–628 (2020). https://doi.org/10.1007/s12311-020-01143-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-020-01143-5