Abstract
Background
The aim of this study was to investigate the surgical treatment of neurologically compromised advanced Kümmell’s disease. The surgical treatment of Kümmell’s disease has various options according to clinical and radiologic status. Far collapsed Kümmell’s disease patients with neurological deficit need to be treated surgically.
Materials and methods
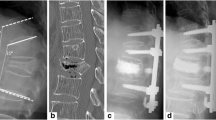
We retrospectively analyzed 22 patients operated to our hospital with neurologically compromised Kümmell’s disease between January 2011 and January 2014. Surgical approach was vertebrectomy, mesh cage insertion and segmental cement-augmented pedicle screw fixation. Corpectomy tissue was examined histopathologically. Anterior vertebral heights, kyphotic angle, the visual analog scale (VAS) and the Frankel classification were used to evaluate the effects of the surgery.
Results
The mean time of follow-up was 26 months (range, 13–40 months). The VAS, anterior vertebral heights, kyphotic angle and neurological state were improved significantly immediate postoperatively and at the last follow-up compared with the preoperative examinations (P < 0.05). Most of the patients in this study exhibited intravertebral clefts, and postoperative pathology revealed bone necrosis.
Conclusion
Posterior vertebrectomy with mesh cage insertion and segmental cement-augmented pedicle screw fixation is an effective option for advanced Kümmell’s disease with neurological deficits.

Similar content being viewed by others
References
Nickell LT, Schucany WG, Opatowsky MJ (2013) Kummell disease. Proc (Bayl Univ Med Cent) 26(3):300–301
Linn J, Birkenmaier C, Hoffmann RT, Reiser M, Baur-Melnyk A (2009) The intravertebral cleft in acute osteoporotic fractures: fluid in magnetic resonance imaging-vacuum in computed tomography? Spine (Phila Pa 1976) 34(2):E88–E93
Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y (2005) Intravertebral cleft sign on fat-suppressed contrast-enhanced MR: correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol 12(8):992–999
Wu AM, Ni WF, Weng W, Chi YL, Xu HZ, Wang XY (2012) Outcomes of percutaneous kyphoplasty in patients with intravertebral vacuum cleft. Acta Orthop Belg 78(6):790–795
Wu AM, Chi YL, Ni WF (2013) Vertebral compression fracture with intravertebral vacuum cleft sign: pathogenesis, image, and surgical intervention. Asian Spine J 7(2):148–155
Osterhouse MD, Kettner NW (2002) Delayed posttraumatic vertebral collapse with intravertebral vacuum cleft. J Manipulative Physiol Ther 25(4):270–275
Zhang X, Hu W, Yu J, Wang Z, Wang Y (2016) An effective treatment option for Kummell disease with neurological deficits: modified transpedicular subtraction and disc osteotomy combined with long-segment fixation. Spine (Phila Pa 1976) 41(15):E923–E930
Nakamae T, Fujimoto Y, Yamada K, Hashimoto T, Olmarker K (2015) Efficacy of percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures with intravertebral cleft. Open Orthop J 9:107–113
Capaul M, Zollinger H, Satz N, Dietz V, Lehmann D, Schurch B (1994) Analyses of 94 consecutive spinal cord injury patients using ASIA definition and modified Frankel score classification. Paraplegia 32(9):583–587
Maldague BE, Noel HM, Malghem JJ (1978) The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology 129(1):23–29
Malghem J, Maldague B, Labaisse MA, Dooms G, Duprez T, Devogelaer JP et al (1993) Intravertebral vacuum cleft: changes in content after supine positioning. Radiology 187(2):483–487
Hatano H, Oike N, Ariizumi T, Sasaki T, Kawashima H (2016) Intravertebral cleft in pathological vertebral collapse resulting from cancer metastasis: report of three cases. Skeletal Radiol 45(12):1747–1750
Kawaguchi S, Horigome K, Yajima H, Oda T, Kii Y, Ida K et al (2010) Symptomatic relevance of intravertebral cleft in patients with osteoporotic vertebral fracture. J Neurosurg Spine 13(2):267–275
Chen GD, Lu Q, Wang GL, Zou J, Yang HL, Yang Y et al (2015) Percutaneous kyphoplasty for Kummell disease with severe spinal canal stenosis. Pain Physician 18(6):E1021–E1028
Park YS, Kim HS (2014) Prevention and treatment of multiple osteoporotic compression fracture. Asian Spine J 8(3):382–390
Kim SB, Jeon TS, Lee WS, Roh JY, Kim JY, Park WK (2010) Comparison of kyphoplasty and lordoplasty in the treatment of osteoporotic vertebral compression fracture. Asian Spine J 4(2):102–108
Huang Y, Peng M, He S, Tang X, Dai M, Tang C (2016) Clinical efficacy of percutaneous kyphoplasty at the hyperextension position for the treatment of osteoporotic Kummell disease. Clin Spine Surg 29(4):161–166
Jung JY, Lee MH, Ahn JM (2006) Leakage of polymethylmethacrylate in percutaneous vertebroplasty: comparison of osteoporotic vertebral compression fractures with and without an intravertebral vacuum cleft. J Comput Assist Tomogr 30(3):501–506
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author (Yongjae Cho) declares that he has no conflict of interest. The institutional review board in our hospital approved the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was conducted in accordance with approval from the ethics committee of our institute.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Cho, Y. Corpectomy and circumferential fusion for advanced thoracolumbar Kümmell’s disease. Musculoskelet Surg 101, 269–274 (2017). https://doi.org/10.1007/s12306-017-0480-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-017-0480-1