Abstract
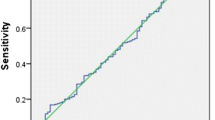
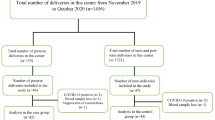
Twenty five percent of pregnant women have some degree of vaginal bleeding during the first trimester, and about 50% of those pregnancies end in spontaneous abortion (SA) because the fetus is not developing typically. As studies have reported that inadequacies of trace metals such as Copper (Cu), Zinc (Zn), Magnesium (Mg) can predispose to various adverse pregnancy outcomes (PO); multiple micronutrient (MMN) supplementations are given without justifying their deficiency and toxicities on the fetus. Earlier studies on effects of MMN supplementations during pregnancy have not considered the need, duration, dose, and time of initiation of supplementations leading to inconclusive results. So, there is a need to optimize this to prevent their abuse and side effects. This study can help in establishing critical cut-offs of these minerals in maternal serum that can forecast future pregnancy outcomes. Study measured the serum Zn, Cu, Mg, and Fe in pregnant women who presented with (n = 80) and without (n = 100) SA at 5–2 weeks of pregnancy using iron -ferrozine method, magnesium-calmagite method, zinc reaction with nitro-PAPS, copper reaction with Di-Br- PAESA methods, respectively. Data analyzed using the student t test and cutoff value was established using Receiver Operating Characteristic (ROC) by SPSS software. Maternal serum Cu, Mg, Fe, and Zn levels measured were significantly lower in SA as compared to that of controls (p < 0.005) (Fig. 1) and maternal age and Body mass index were not statistically significant different among study group. Maternal serum Cu, Mg, Zn and Iron (Fe) measured in 5–12 weeks of pregnancy has the potential to forecast future occurrence of SA. The study has been registered under “The Clinical Trials Registry- India (CTRI),” -REF/2020/01/030393.

Similar content being viewed by others
References
Turan K, Arslan A, Uçkan K, Demir H, Demir C. Change of the levels of trace elements and heavy metals in threatened abortion. J Chin Med Assoc. 2019;82(7):554–7.
Thaker R, Oza H, Shaikh I, Kumar S. Correlation of copper and zinc in spontaneous abortion. Int J Fertility Sterility. 2019;13(2):97.
Sami AS, Suat E, Alkis I, Karakus Y, Guler S. The role of trace element, mineral, vitamin and total antioxidant status in women with habitual abortion. J Matern Fetal Neonatal Med. 2021;34(7):1055–62.
Wu G, Imhoff-Kunsch B, Girard AW. Biological mechanisms for nutritional regulation of maternal health and fetal development. Paediatr Perinat Epidemiol. 2012;26:4–26.
Borella P, Szilagyi A, Than G, Csaba I, Giardino A, Facchinetti F. Maternal plasma concentrations of magnesium, calcium, zinc and copper in normal and pathological pregnancies. Sci Total Environ. 1990;99(1–2):67–76.
Kojima C, Shoji H, Ikeda N, Kitamura T, Hisata K, Shimizu T. Association of zinc and copper with clinical parameters in the preterm newborn. Pediatr Int. 2017;59(11):1165–8.
Pathak P, Kapil U. Role of trace elements zinc, copper and magnesium during pregnancy and its outcome. Indian J Pediatrics. 2004;71(11):1003–5.
Pérez-Debén S, Gonzalez-Martin R, Palomar A, Quiñonero A, Salsano S, Dominguez F. Copper and lead exposures disturb reproductive features of primary endometrial stromal and epithelial cells. Reprod Toxicol. 2020;93:106–17.
Brown B, Wright C. Safety and efficacy of supplements in pregnancy. Nutr Rev. 2020;78(10):813–26.
Saxena T, Agarwal BK, Makwane HS, Kare P. Study of serum zinc and magnesium levels in patients of liver cirrhosis. Biomed Pharmacol J. 2015;5(2):327–31.
Ahmed SE, Maher FT, Naji NA. Effect of Thyroid Hormones and Trace Elements (Zn, Mg) on Obesity. Tikrit J Pure Sci. 2018;21(6):78–84.
Walle BM, Adekunle AO, Arowojolu AO, Dugul TT, Mebiratie AL. Micronutrients deficiency and their associations with pregnancy outcomes: a review. Nutr Diet Suppl. 2020;12:237.
Ahmadi R, Ziaei S, Parsay S. Association between nutritional status with spontaneous abortion. Int J Fertility Sterility. 2017;10(4):337.
Bakhshandeh Nosrat S, Ghaemi EA, Ahmadi A, Behnampour N, Marjani A, Mansourian AR. Maternal serum copper concentration in premature rupture of membrane: a case-control study. J Biol Sci. 2014;14(1):73–6.
Wang H, Hu YF, Hao JH, Chen YH, Su PY, Wang Y, et al. Maternal zinc deficiency during pregnancy elevates the risks of fetal growth restriction: a population-based birth cohort study. Sci Rep. 2015;5(1):1.
Okunade KS, Oluwole AA, Adegbesan-Omilabu MA. A study on the association between low maternal serum magnesium level and preterm labour. Advances in medicine. 2014.
Miodovnik M, Mimouni F, Siddiqi TA, Tsang RC. Periconceptional metabolic status and risk for spontaneous abortion in insulin-dependent diabetic pregnancies. Am J Perinatol. 1988;5(04):368–73.
Ying Y, Pan P, Zou C, Wang Y, Tang Y, Hou X, et al. Tebuconazole exposure disrupts placental function and causes fetal low birth weight in rats. Chemosphere. 2021;264:128432.
Díaz-López A, Ribot B, Basora J, Arija V. High and low haemoglobin levels in early pregnancy are associated to a higher risk of miscarriage: a population-based cohort study. Nutrients. 2021;13(5):1578.
Acknowledgements
The authors thank the Indian Council of Medical Research (ICMR), New Delhi, India [File No 5/7/79/MH/Adhoc/2020-RBMCH] for funding this research project to Mahadev Rao. All the authors stated in the study equally contributed to the study design, and the principal author made analysis and performance of the study. The article was written and reviewed by the principal and corresponding author. We acknowledge Kasturba hospital, Manipal, Manipal Academy of higher education to permit us and provide patients for the study.
Funding
The present study analysis funding contributed by Kasturba medical college, Manipal, Manipal Academy of higher education, Manipal, India.
Author information
Authors and Affiliations
Contributions
S-Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing, Patient recruitment. KP-Protocol/project development, Manuscript writing/editing. VGP-Protocol/project development, Patient recruitment. SS-Protocol/project development. MR- Protocol/project development. AK-Statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Ethical Approval
This study was approved by the appropriate institutional ethics committee- Kasturba medical college and the hospital institutional ethical committee (IEC:182/2018) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study has been registered under “The Clinical Trials Registry- India (CTRI),” -REF/2020/01/030393.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sairoz, Prabhu, K., Poojari, V.G. et al. Maternal Serum Zinc, Copper, Magnesium, and Iron in Spontaneous Abortions. Ind J Clin Biochem 38, 128–131 (2023). https://doi.org/10.1007/s12291-022-01043-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12291-022-01043-x