Abstract
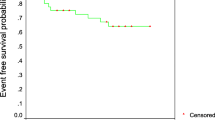
Acute lymphoblastic leukemia (ALL) is the most common cancer in childhood, and the Hispanic race has the highest incidence worldwide. Disparities in survival rates exist among different regions of the world. Due to this heterogeneity and possible differences in the outcomes within Mexico, the aim of this study was to analyze the clinical outcomes of cohort of pediatric patients with ALL treated in a highly specialized medical unit located in the Bajio region of Mexico. Observational retrospective study of a cohort of pediatric patients with ALL treated in a tertiary-level hospital in the Bajio region of Mexico, between January 2016 and December 2021. A total of 146 patients were included with a median age of 7 years. The 68.5% of patients were at high risk. CNS involvement was present in 2.7%, and Philadelphia chromosome positive in 2%. Cytogenetic analysis was performed in 16.4% patients. The median follow-up of entire cohort was 32 months. The most frequently administered chemotherapy treatment was Total Therapy XV in 79.5% of patients. The complete remission rate was 89%. Refractory disease was present in 2.7%. Induction-related mortality was 8.2%. The relapse rate was present in 26%. The 3-years overall survival was 57.5%, and the 3-years event-free survival was 53.4%. A more aggressive course and worse survival occur in our cohort of pediatric patients with ALL. Strategies should be proposed inside Mexico and other low-middle income countries with the aim of improving the overall survival.

Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
National Cancer Institute. NCCR*Explorer: An interactive website for NCCR cancer statistic. Retrieved from https://NCCRExplorer.ccdi.cancer.gov. Accessed 15 Mar 2024
Rivera-Luna R, Shalkow-Klincovstein J, Velasco-Hidalgo L et al (2014) Descriptive Epidemiology in Mexican children with cancer under an open national public health insurance program. BMC Cancer 29(14):790. https://doi.org/10.1186/1471-2407-14-790
Inaba H, Pui CH (2021) Advances in the Diagnosis and Treatment of Pediatric Acute Lymphoblastic Leukemia. J Clin Med 10(9):1926. https://doi.org/10.3390/jcm10091926
Inaba H, Mullighan CG (2020) Pediatric acute lymphoblastic leukemia. Haematologica 105(11):2524–2539. https://doi.org/10.3324/haematol.2020.247031.PMID:33054110;PMCID:PMC7604619
Winestone LE, Aplenc R (2019) Disparities in Survival and Health Outcomes in Childhood Leukemia. Curr Hematol Malig Rep 14(3):179–186. https://doi.org/10.1007/s11899-019-00515-x
Davitt M, Gennarini L, Loeb D, Fazzari M, Hosgood HD (2023) Impact of race/ethnicity and language preferences on pediatric ALL survival outcomes. Cancer Med 11:12827–12836. https://doi.org/10.1002/cam4.5951
Gupta S, Dai Y, Chen Z et al (2023) Racial and ethnic disparities in childhood and young adult acute lymphocytic leukaemia: secondary analyses of eight Children’s Oncology Group cohort trials. Lancet Haematol 10(2):e129–e141. https://doi.org/10.1016/S2352-3026(22)00371-4
Janitz AE, Barber R, Campbell JE et al (2022) Measuring disparities in event-free survival among children with acute lymphoblastic leukemia in an academic institute in Oklahoma, 2005–2019. Cancer Epidemiol 81:102275. https://doi.org/10.1016/j.canep.2022.102275
Eche IJ, Aronowitz T (2020) A Literature Review of Racial Disparities in Overall Survival of Black Children with Acute Lymphoblastic Leukemia Compared with White Children with Acute Lymphoblastic Leukemia. J Pediatr Oncol Nurs 37(3):180–194. https://doi.org/10.1177/1043454220907547
Jaime-Pérez JC, López-Razo ON, García-Arellano G et al (2016) Results of Treating Childhood Acute Lymphoblastic Leukemia in a Low-middle Income Country: 10 Year Experience in Northeast Mexico. Arch Med Res 47(8):668–676. https://doi.org/10.1016/j.arcmed.2017.01.004
Muñoz-Aguirre P, Zapata-Tarrés M, Espinosa-Tamez P, Sánchez-Blas H, Brochier M, Lamadrid-Figueroa H (2022) Childhood acute lymphoblastic leukemia in Mexico: mortality trend analysis, 1998–2018. Salud Publica Mex 64(1):26–34. https://doi.org/10.21149/13210
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X
Arber DA, Orazi A, Hasserjian R et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127(20):2391–2405. https://doi.org/10.1182/blood-2016-03-643544
Chadha R, Udayakumar DS, Sangwan S et al (2023) Cytogenetic Risk Stratification of B-Acute Lymphoblastic Leukemia and Its Correlation with Other Prognostic Factors. Indian J Hematol Blood Transfus 39(1):141–145. https://doi.org/10.1007/s12288-022-01541-1
Pui CH, Relling MV, Sandlund JT, Downing JR, Campana D, Evans WE (2004) Rationale and design of Total Therapy Study XV for newly diagnosed childhood acute lymphoblastic leukemia. Ann Hematol 83(Suppl 1):S124–S126. https://doi.org/10.1007/s00277-004-0850-2
Pui CH, Sandlund JT, Pei D et al (2004) Improved outcome for children with acute lymphoblastic leukemia: results of Total Therapy Study XIIIB at St Jude Children’s Research Hospital. Blood 104(9):2690–2696. https://doi.org/10.1182/blood-2004-04-1616
Koka A, Saygin C, Uzunaslan D, Ozdemir N, Apak H, Celkan T (2014) A 17-year experience with ALL-BFM protocol in acute lymphoblastic leukemia: prognostic predictors and interruptions during protocol. Leuk Res 38(6):699–705. https://doi.org/10.1016/j.leukres.2014.03.016
Buchmann S, Schrappe M, Baruchel A et al (2022) Remission, treatment failure, and relapse in pediatric ALL: an international consensus of the Ponte-di-Legno Consortium. Blood 139(12):1785–1793. https://doi.org/10.1182/blood.2021012328
Pui CH, Yang JJ, Hunger SP et al (2015) Childhood Acute Lymphoblastic Leukemia: Progress Through Collaboration. J Clin Oncol 33(27):2938–48. https://doi.org/10.1200/JCO.2014.59.1636
Pieters R, de Groot-Kruseman H, Van der Velden V et al (2016) Successful Therapy Reduction and Intensification for Childhood Acute Lymphoblastic Leukemia Based on Minimal Residual Disease Monitoring: Study ALL10 From the Dutch Childhood Oncology Group. J Clin Oncol 34(22):2591–2601. https://doi.org/10.1200/JCO.2015.64.6364
Vora A, Goulden N, Mitchell C et al (2014) Augmented post-remission therapy for a minimal residual disease-defined high-risk subgroup of children and young people with clinical standard-risk and intermediate-risk acute lymphoblastic leukaemia (UKALL 2003): a randomised controlled trial. Lancet Oncol 15(8):809–818. https://doi.org/10.1016/S1470-2045(14)70243-8
Toft N, Birgens H, Abrahamsson J et al (2018) Results of NOPHO ALL2008 treatment for patients aged 1–45 years with acute lymphoblastic leukemia. Leukemia 32(3):606–615. https://doi.org/10.1038/leu.2017.265
Moreira DC, González-Ramella O, Echavarría Valenzuela M et al (2023) Evaluation of factors leading to poor outcomes for pediatric acute lymphoblastic leukemia in Mexico: a multi-institutional report of 2,116 patients. Front Oncol 18(13):1255555. https://doi.org/10.3389/fonc.2023.1255555
Duffy C, Graetz DE, Lopez AMZ et al (2023) Retrospective analysis of outcomes for pediatric acute lymphoblastic leukemia in South American centers. Front Oncol 30(13):1254233. https://doi.org/10.3389/fonc.2023.1254233
Abdelmabood S, Fouda AE, Boujettif F, Mansour A (2020) Treatment outcomes of children with acute lymphoblastic leukemia in a middle-income developing country: high mortalities, early relapses, and poor survival. J Pediatr (Rio J) 96(1):108–116. https://doi.org/10.1016/j.jped.2018.07.013
Ornelas-Sánchez M, Nuño-Vázquez L, Loera-Reyna A et al (2018) The “Golden Hour”: a capacity-building initiative to decrease life-threating complications related to neutropenic fever in patients with hematologic malignancies in low- and middle-income countries. Blood Adv 2(Suppl 1):63–66. https://doi.org/10.1182/bloodadvances.2018GS112240
Espinoza D, Blanco Lopez JG, Vasquez R, Fu L et al (2023) How should childhood acute lymphoblastic leukemia relapses in low-income and middle-income countries be managed: The AHOPCA-ALL study group experience. Cancer 129(5):771–779. https://doi.org/10.1002/cncr.34572
Parker C, Waters R, Leighton C et al (2010) Effect of mitoxantrone on outcome of children with first relapse of acute lymphoblastic leukaemia (ALL R3): an open-label randomised trial. Lancet 376(9757):2009–17. https://doi.org/10.1016/S0140-6736(10)62002-8
Shoag JM, Barredo JC, Lossos IS, Pinheiro PS (2020) Acute lymphoblastic leukemia mortality in Hispanic Americans. Leuk Lymphoma 61(11):2674–2681. https://doi.org/10.1080/10428194.2020.1779260
Mishra V, Jain S, Anand V, Malhotra P, Tejwani N, Kapoor G (2023) Impact of minimal residual disease on relapse in childhood acute lymphoblastic leukemia: Lessons learnt from a tertiary cancer center in India. Pediatr Hematol Oncol 40(6):517–528. https://doi.org/10.1080/08880018.2023.2186553
Pui CH (2020) Precision medicine in acute lymphoblastic leukemia. Front Med 14(6):689–700. https://doi.org/10.1007/s11684-020-0759-8
Toksvang LN, Als-Nielsen B, Bacon C et al (2022) Thiopurine Enhanced ALL Maintenance (TEAM): study protocol for a randomized study to evaluate the improvement in disease-free survival by adding very low dose 6-thioguanine to 6-mercaptopurine/methotrexate-based maintenance therapy in pediatric and adult patients (0–45 years) with newly diagnosed B-cell precursor or T-cell acute lymphoblastic leukemia treated according to the intermediate risk-high group of the ALLTogether1 protocol. BMC Cancer 22(1):483. https://doi.org/10.1186/s12885-022-09522-3
Jeha S, Pei D, Choi J et al (2019) Improved CNS Control of Childhood Acute Lymphoblastic Leukemia Without Cranial Irradiation: St Jude Total Therapy Study 16. J Clin Oncol 37(35):3377–3391. https://doi.org/10.1200/JCO.19.01692
Pawinska-Wasikowska K, Wieczorek A, Balwierz W, Bukowska-Strakova K, Surman M, Skoczen S (2022) Blinatumomab as a Bridge Therapy for Hematopoietic Stem Cell Transplantation in Pediatric Refractory/Relapsed Acute Lymphoblastic Leukemia. Cancers (Basel) 14(2):458. https://doi.org/10.3390/cancers14020458
Pacheco C, Lucchini G, Valsecchi MG et al (2014) Childhood acute lymphoblastic leukemia in Nicaragua: long-term results in the context of an international cooperative program. Pediatr Blood Cancer 61(5):827–832. https://doi.org/10.1002/pbc.24871
O’Connor D, Bate J, Wade R et al (2014) Infection-related mortality in children with acute lymphoblastic leukemia: an analysis of infectious deaths on UKALL2003. Blood 124(7):1056–1061. https://doi.org/10.1182/blood-2014-03-560847
Inaba H, Pei D, Wolf J et al (2017) Infection-related complications during treatment for childhood acute lymphoblastic leukemia. Ann Oncol 28(2):386–392. https://doi.org/10.1093/annonc/mdw557.PMID:28426102;PMCID:PMC5834143
Harvey RC, Mullighan CG, Chen IM et al (2010) Rearrangement of CRLF2 is associated with mutation of JAK kinases, alteration of IKZF1, Hispanic/Latino ethnicity, and a poor outcome in pediatric B-progenitor acute lymphoblastic leukemia. Blood 115(26):5312–21. https://doi.org/10.1182/blood-2009-09-245944
Das N, Banavali S, Bakhshi S et al (2022) Protocol for ICiCLe-ALL-14 (InPOG-ALL-15–01): a prospective, risk stratified, randomised, multicentre, open label, controlled therapeutic trial for newly diagnosed childhood acute lymphoblastic leukaemia in India. Trials 23(1):102. https://doi.org/10.1186/s13063-022-06033-1
Parihar M, Singh MK, Islam R et al (2018) A triple-probe FISH screening strategy for risk-stratified therapy of acute lymphoblastic leukaemia in low-resource settings. Pediatr Blood Cancer 65(12):e27366. https://doi.org/10.1002/pbc.27366
Acknowledgements
Nancy E. Carbajal Rodríguez M.D. and Martha M. Orozco León M.D.
Funding
This research did not receive any external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martínez Villegas, O., Alatoma Medina, N.E., Romero Vázquez, M.J. et al. Clinical Outcomes of Pediatric Acute Lymphoblastic Leukemia in the Bajio Region of Mexico: A Retrospective Cohort Study. Indian J Hematol Blood Transfus (2024). https://doi.org/10.1007/s12288-024-01787-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12288-024-01787-x