Abstract
Background
Artificial Intelligence (AI) offers an approach to predictive modeling. The model learns to determine specific patterns of undesirable outcomes in a dataset. Therefore, a decision-making algorithm can be built based on these patterns to prevent negative results. This systematic review aimed to evaluate the usefulness of AI in breast reconstruction.
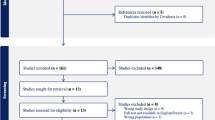
Methods
A systematic review was conducted in August 2022 following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. MEDLINE, EMBASE, SCOPUS, and Google Scholar online databases were queried to capture all publications studying the use of artificial intelligence in breast reconstruction.
Results
A total of 23 studies were full text-screened after removing duplicates, and twelve articles fulfilled our inclusion criteria. The Machine Learning algorithms applied for neuropathic pain, lymphedema diagnosis, microvascular abdominal flap failure, donor site complications associated to muscle sparing Transverse Rectus Abdominis flap, surgical complications, financial toxicity, and patient-reported outcomes after breast surgery demonstrated that AI is a helpful tool to accurately predict patient results. In addition, one study used Computer Vision technology to assist in Deep Inferior Epigastric Perforator Artery detection for flap design, considerably reducing the preoperative time compared to manual identification.
Conclusions
In breast reconstruction, AI can help the surgeon by optimizing the perioperative patients’ counseling to predict negative outcomes, allowing execution of timely interventions and reducing the postoperative burden, which leads to obtaining the most successful results and improving patient satisfaction.




Similar content being viewed by others
References
Feijóo C, Kwon Y, Bauer JM, et al. Harnessing artificial intelligence (AI) to increase wellbeing for all: the case for a new technology diplomacy. Telecommunications Policy. 2020;44(6):101988.
Diaz-Flores E, Meyer T, Giorkallos A. Evolution of artificial intelligence-powered technologies in biomedical research and healthcare. Adv Biochem Eng Biotechnol. 2022;182:23–60.
Asai A, Konno M, Taniguchi M, Vecchione A, Ishii H. Computational healthcare: present and future perspectives (Review). Exp Ther Med. 2021;22(6):1351.
Rajesh A, Asaad M. Artificial intelligence in surgery: a revolution in progress. Am Surg. 2022;31348221117024.
Hamet P, Tremblay J. Artificial intelligence in medicine. Metabolism. 2017;69:S36-s40.
Mintz Y, Brodie R. Introduction to artificial intelligence in medicine. Minim Invasive Ther Allied Technol. 2019;28(2):73–81.
Hashimoto DA, Rosman G, Rus D, Meireles OR. Artificial intelligence in surgery: promises and perils. Ann Surg. 2018;268(1):70–6.
Rimmer L, Howard C, Picca L, Bashir M. The automaton as a surgeon: the future of artificial intelligence in emergency and general surgery. Eur J Trauma Emerg Surg. 2021;47(3):757–62.
Loftus TJ. Introduction to the artificial intelligence in surgery series. Surgery. 2021;169(4):744–5.
Moglia A, Georgiou K, Georgiou E, Satava RM, Cuschieri A. A systematic review on artificial intelligence in robot-assisted surgery. Int J Surg. 2021;95:106151.
Beyaz S. A brief history of artificial intelligence and robotic surgery in orthopedics & traumatology and future expectations. Jt Dis Relat Surg. 2020;31(3):653–5.
Ahmad A. Breast cancer statistics: recent trends. Adv Exp Med Biol. 2019;1152:1–7.
Sun L, Ang E, Ang WHD, Lopez V. Losing the breast: a meta-synthesis of the impact in women breast cancer survivors. Psychooncology. 2018;27(2):376–85.
Ośmiałowska E, Misiąg W, Chabowski M, Jankowska-Polańska B. Coping strategies, pain, and quality of life in patients with breast cancer. J Clin Med. 2021;10(19):4469.
Yin J, Ngiam KY, Teo HH. Role of artificial intelligence applications in real-life clinical practice: systematic review. J Med Internet Res. 2021;23(4):e25759.
Buda M, Saha A, Walsh R, et al. A data set and deep learning algorithm for the detection of masses and architectural distortions in digital breast tomosynthesis images. JAMA Netw Open. 2021;4(8):e2119100.
Becker AS, Marcon M, Ghafoor S, Wurnig MC, Frauenfelder T, Boss A. Deep learning in mammography: diagnostic accuracy of a multipurpose image analysis software in the detection of breast cancer. Invest Radiol. 2017;52(7):434–40.
Soh CL, Shah V, Arjomandi Rad A, et al. Present and future of machine learning in breast surgery: systematic review. Br J Surg. 2022. https://doi.org/10.1093/bjs/znac224.
Fu MR, Wang Y, Li C, et al. Machine learning for detection of lymphedema among breast cancer survivors. Mhealth. 2018;4:17.
Myung Y, Jeon S, Heo C, et al. Validating machine learning approaches for prediction of donor related complication in microsurgical breast reconstruction: a retrospective cohort study. Sci Rep. 2021;11(1):5615.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Lötsch J, Sipilä R, Dimova V, Kalso E. Machine-learned selection of psychological questionnaire items relevant to the development of persistent pain after breast cancer surgery. Br J Anaesth. 2018;121(5):1123–32.
Juwara L, Arora N, Gornitsky M, Saha-Chaudhuri P, Velly AM. Identifying predictive factors for neuropathic pain after breast cancer surgery using machine learning. Int J Med Inform. 2020;141: 104170.
O’Neill AC, Yang D, Roy M, Sebastiampillai S, Hofer SOP, Xu W. Development and evaluation of a machine learning prediction model for flap failure in microvascular breast reconstruction. Ann Surg Oncol. 2020;27(9):3466–75.
van Egdom LSE, Pusic A, Verhoef C, Hazelzet JA, Koppert LB. Machine learning with PROs in breast cancer surgery; caution: collecting PROs at baseline is crucial. Breast J. 2020;26(6):1213–5.
Naoum GE, Ho AY, Shui A, et al. Risk of developing breast reconstruction complications: a machine-learning nomogram for individualized risk estimation with and without postmastectomy radiation therapy. Plast Reconstr Surg. 2022;149(1):1e–12e.
Pfob A, Mehrara BJ, Nelson JA, Wilkins EG, Pusic AL, Sidey-Gibbons C. Machine learning to predict individual patient-reported outcomes at 2-year follow-up for women undergoing cancer-related mastectomy and breast reconstruction (INSPiRED-001). Breast. 2021;60:111–22.
Pfob A, Mehrara BJ, Nelson JA, Wilkins EG, Pusic AL, Sidey-Gibbons C. Towards patient-centered decision-making in breast cancer surgery: machine learning to predict individual patient-reported outcomes at 1-year follow-up. Ann Surg. 2021. https://doi.org/10.1097/SLA.0000000000004862.
Sidey-Gibbons C, Pfob A, Asaad M, et al. Development of machine learning algorithms for the prediction of financial toxicity in localized breast cancer following surgical treatment. JCO Clin Cancer Inform. 2021;5:338–47.
Shi Y-C, Li J, Li S-J, et al. Flap failure prediction in microvascular tissue reconstruction using machine learning algorithms. World J Clin Cases. 2022;10(12):3729.
Mavioso C, Araujo RJ, Oliveira HP, et al. Automatic detection of perforators for microsurgical reconstruction. Breast. 2020;50:19–24.
Eldaly AS, Avila FR, Torres-Guzman RA, et al. Simulation and artificial intelligence in rhinoplasty: a systematic review. Aesthet Plast Surg. 2022. https://doi.org/10.1007/s00266-022-02883-x.
Chandawarkar A, Chartier C, Kanevsky J, Cress PE. A practical approach to artificial intelligence in plastic surgery. Aesthet Surg J Open Forum. 2020;2:ojaa001.
Eldaly AS, Avila FR, Torres-Guzman RA, et al. Artificial intelligence and lymphedema: state of the art. J Clin Transl Res. 2022;8(3):234–42.
Dembrower K, Wåhlin E, Liu Y, et al. Effect of artificial intelligence-based triaging of breast cancer screening mammograms on cancer detection and radiologist workload: a retrospective simulation study. Lancet Digit Health. 2020;2(9):e468–74.
Huang SH, Loh JK, Tsai JT, Houg MF, Shi HY. Predictive model for 5-year mortality after breast cancer surgery in Taiwan residents. Chin J Cancer. 2017;36(1):23.
Lou SJ, Hou MF, Chang HT, et al. Machine learning algorithms to predict recurrence within 10 years after breast cancer surgery: a prospective cohort study. Cancers (Basel). 2020;12(12):3817.
Eldaly AS, Avila FR, Torres-Guzman RA, et al. Radiomics and artificial intelligence in predicting axillary lymph node metastasis in breast cancer: a systematic review. Curr Med Imaging. 2022. https://doi.org/10.2174/1573405618666220822093226.
Choi RY, Coyner AS, Kalpathy-Cramer J, Chiang MF, Campbell JP. Introduction to machine learning, neural networks, and deep learning. Transl Vis Sci Technol. 2020;9(2):14.
Badillo S, Banfai B, Birzele F, et al. An introduction to machine learning. Clin Pharmacol Ther. 2020;107(4):871–85.
Maita K, Garcia JP, Torres RA, et al. Imaging biomarkers for diagnosis and treatment response in patients with lymphedema. Biomark Med. 2022;16(4):303–16.
Manrique OJ, Bustos SS, Ciudad P, et al. Overview of lymphedema for physicians and other clinicians: a review of fundamental concepts. Mayo Clin Proc. 2020;97:1920–35.
Guliyeva G, Huayllani MT, Boczar D, Avila FR, Forte AJ. Correlation of older age with severity of lymphedema in breast cancer survivors: a systematic review. Breast Dis. 2021;40(3):191–7.
Bouhassira D, Attal N, Alchaar H, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005;114(1–2):29–36.
Lötsch J, Ultsch A. Machine learning in pain research. Pain. 2018;159(4):623–30.
Wilkins EG, Hamill JB, Kim HM, et al. Complications in postmastectomy breast reconstruction: one-year outcomes of the mastectomy reconstruction outcomes consortium (MROC) study. Ann Surg. 2018;267(1):164–70.
Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG. Comparison of 2-year complication rates among common techniques for postmastectomy breast reconstruction. JAMA Surg. 2018;153(10):901–8.
Kruppa J, Ziegler A, König IR. Risk estimation and risk prediction using machine-learning methods. Hum Genet. 2012;131(10):1639–54.
Boulesteix AL, Schmid M. Machine learning versus statistical modeling. Biom J. 2014;56(4):588–93.
Nelson JA, Lee IT, Disa JJ. The functional impact of breast reconstruction: an overview and update. Plast Reconstr Surg Glob Open. 2018;6(3): e1640.
Browne JP, Cano SJ, Smith S. Using patient-reported outcome measures to improve health care: time for a new approach. Med Care. 2017;55(10):901–4.
Santosa KB, Qi J, Kim HM, Hamill JB, Wilkins EG, Pusic AL. Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg. 2018;153(10):891–9.
Zhang C, Hu G, Biskup E, Qiu X, Zhang H, Zhang H. Depression induced by total mastectomy, breast conserving surgery and breast reconstruction: a systematic review and meta-analysis. World J Surg. 2018;42(7):2076–85.
Gordon LG, Merollini KMD, Lowe A, Chan RJ. A systematic review of financial toxicity among cancer survivors: we can’t pay the co-pay. Patient. 2017;10(3):295–309.
Acknowledgements
None.
Funding
This work was funded by Mayo Clinic Clinical Research Operations Group, Mayo Clinic Center for Regenerative Medicine.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. They have accepted responsibility for the entire content of this manuscript and approved its submission. Francisco R Avila, and Ricardo A Torres-Guzman, John P Garcia, Gioacchino D De Sario Velasquez, and Sahar Borna conducted the data collection and studies selection. Karla C Maita analyzed the results and wrote the first draft of the article. Olivia S Ho, Sally A Brown, Clifton R Haider, and Antonio Jorge Forte performed a critical revision of the manuscript. Finally, all the authors approved the last version for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
Ethical approval
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Maita, K.C., Avila, F.R., Torres-Guzman, R.A. et al. The usefulness of artificial intelligence in breast reconstruction: a systematic review. Breast Cancer (2024). https://doi.org/10.1007/s12282-024-01582-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12282-024-01582-6