Abstract
Purpose
Emojis are commonly used for daily communication and may be useful in assessing patient-reported outcomes (PROs) in breast cancer. The purpose of this study is to develop and validate a Symptom Illustration Scale (SIS) as a new PRO measurement.
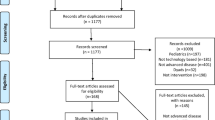
Methods
Eighteen original SIS items were developed from the PRO-CTCAE. In cohort one, the SIS validity and reliability were examined in patients with breast cancer, using a semi-structured five-question survey to investigate content validity. PROs with PRO-CTCAE and SIS were examined twice to determine criteria validity and test–retest reliability. In cohort two, the responsiveness of the scales were examined in patients treated with anthracycline, docetaxel, paclitaxel, and endocrine therapy. PROs with PRO-CTCAE and SIS were investigated two or three times, depending on the therapy.
Results
Patients were enrolled from August 2019 to October 2020. In cohort one (n = 70), most patients had no difficulties with the SIS, but 16 patients indicated that it was difficult to understand severities in the SIS. For criterion validity, Spearman rank correlation coefficients (rs) between PRO-CTCAE and SIS items were ≥ 0.41, except for “Decreased appetite.” For test–retest reliability, κ coefficients of the SIS were ≥ 0.41 for 16/18 items (88.9%). Response time was significantly shorter for the SIS than for PRO-CTCAE (p < 0.001). In cohort two (n = 106), score changes between PRO-CTCAE and SIS for relevant symptoms all had correlations with rs ≥ 0.41.
Conclusion
An original SIS from the PRO-CTCAE for patients with breast cancer were verified the validity, reliability, and responsiveness. Further studies to improve and validate the SIS are needed.




Similar content being viewed by others
Data availability
Upon request, the authors prepare to send relevant documentation or data without sensitive information in the form of confidential proprietary data in order to verify the validity of the results.
References
Harbeck N, Iyer S, Turner N, et al. Quality of life with palbociclib plus fulvestrant in previously treated hormone receptor-positive, HER2-negative metastatic breast cancer: patient-reported outcomes from the PALOMA-3 trial. Ann Oncol Off J Eur Soc Med Oncol. 2016;27:1047–54. https://doi.org/10.1093/annonc/mdw139.
LeBlanc TW, Abernethy AP. Patient-reported outcomes in cancer care - hearing the patient voice at greater volume. Nat Rev Clin Oncol. 2017;14:763–72. https://doi.org/10.1038/nrclinonc.2017.153.
Takashima T, Mukai H, Hara F, et al. Taxanes versus S-1 as the first-line chemotherapy for metastatic breast cancer (SELECT BC): an open-label, non-inferiority, randomised phase 3 trial. Lancet Oncol. 2016;17:90–8. https://doi.org/10.1016/S1470-2045(15)00411-8.
Basch E, Iasonos A, Barz A, et al. Long-term toxicity monitoring via electronic patient-reported outcomes in patients receiving chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol. 2007;25:5374–80. https://doi.org/10.1200/JCO.2007.11.2243.
Judson TJ, Bennett AV, Rogak LJ, et al. Feasibility of long-term patient self-reporting of toxicities from home via the Internet during routine chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31:2580–5. https://doi.org/10.1200/JCO.2012.47.6804.
Wallwiener M, Matthies L, Simoes E, et al. Reliability of an e-PRO Tool of EORTC QLQ-C30 for measurement of health-related quality of life in patients with breast cancer: prospective randomized trial. J Med Internet Res. 2017;19:e322. https://doi.org/10.2196/jmir.8210.
Kikawa Y, Hatachi Y, Rumpold G, et al. Evaluation of health-related quality of life via the computer-based health evaluation system (CHES) for Japanese metastatic breast cancer patients: a single-center pilot study. Breast Cancer Tokyo Jpn. 2019;26:255–9. https://doi.org/10.1007/s12282-018-0905-1.
Yang J, Weng L, Chen Z, et al. Development and testing of a mobile app for pain management among cancer patients discharged from hospital treatment: randomized controlled trial. JMIR MHealth UHealth. 2019;7:e12542. https://doi.org/10.2196/12542.
Nipp RD, El-Jawahri A, Ruddy M, et al. Pilot randomized trial of an electronic symptom monitoring intervention for hospitalized patients with cancer. Ann Oncol Off J Eur Soc Med Oncol. 2019;30:274–80. https://doi.org/10.1093/annonc/mdy488.
Velikova G, Booth L, Smith AB, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol Off J Am Soc Clin Oncol. 2004;22:714–24. https://doi.org/10.1200/JCO.2004.06.078.
Berry DL, Hong F, Halpenny B, et al. Electronic self-report assessment for cancer and self-care support: results of a multicenter randomized trial. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32:199–205. https://doi.org/10.1200/JCO.2013.48.6662.
Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol Off J Am Soc Clin Oncol. 2016;34:557–65. https://doi.org/10.1200/JCO.2015.63.0830.
Denis F, Lethrosne C, Pourel N, et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. JNCI J Natl Cancer Inst. 2017. https://doi.org/10.1093/jnci/djx029.
Bond DM, Hammond J, Shand AW, Nassar N. Comparing a mobile phone automated system with a paper and email data collection system: substudy within a randomized controlled trial. JMIR MHealth UHealth. 2020;8:e15284. https://doi.org/10.2196/15284.
US National Cancer Institute. Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAETM). http:// outcomes.cancer.gov/tools/pro-ctcae.html. Accessed 10 Apr 2019. 50.
Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad Emerg Med Off J Soc Acad Emerg Med. 2010;17:50–4. https://doi.org/10.1111/j.1553-2712.2009.00620.x.
Lee ACK, Tang SW, Yu GKK, Cheung RTF. The smiley as a simple screening tool for depression after stroke: a preliminary study. Int J Nurs Stud. 2008;45:1081–9. https://doi.org/10.1016/j.ijnurstu.2007.05.008.
Tang Y. Emoticon, emoji, and sticker use in computer-mediated communication: a review of theories and research findings. 2019;27.
Lai D, Lee J, He S. Emoji for the medical community-challenges and opportunities. JAMA. 2021;326:795–6. https://doi.org/10.1001/jama.2021.8409.
Van Dam L, Rietstra S, Van der Drift E, et al. Can an emoji a day keep the doctor away? An explorative mixed-methods feasibility study to develop a self-help app for youth with mental health problems. Front Psychiatry. 2019;10:593. https://doi.org/10.3389/fpsyt.2019.00593.
Bai Q, Dan Q, Mu Z, Yang M. A systematic review of emoji: current research and future perspectives. Front Psychol. 2019;10:2221. https://doi.org/10.3389/fpsyg.2019.02221.
Bieri D, Reeve RA, Champion DG, et al. The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: development, initial validation, and preliminary investigation for ratio scale properties. Pain. 1990;41:139–50. https://doi.org/10.1016/0304-3959(90)90018-9.
Macdonald L, Bruce J, Scott NW, et al. Long-term follow-up of breast cancer survivors with post-mastectomy pain syndrome. Br J Cancer. 2005;92:225–30. https://doi.org/10.1038/sj.bjc.6602304.
Terwee CB, Dekker FW, Wiersinga WM, et al. On assessing responsiveness of health-related quality of life instruments: guidelines for instrument evaluation. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2003;12:349–62. https://doi.org/10.1023/a:1023499322593.
Funding
This study was funded by Pfizer Inc.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study and design. Material preparation, data collection, and analysis were performed by YS, NT, TI, YK, YU, YH, and SY. The first draft of the manuscript was written by YS and all authors commented on versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Tadahiko Shien, Yuichiro Kikawa, and Naruto Taira received an honorarium from Pfizer Inc.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Okayama University Hospital (Cohort one: Date 2019.5.28/No. 1907–038, Cohort two: Date 2019.11.29/No. 1907–042).
Research involving human participants and/or animals
This study involving human participants was in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent to participate
Written informed consent was obtained from all participants in the study.
Consent to publish
The authors affirm that all patients provided informed consent for publication of all figures and tables.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12282_2023_1480_MOESM1_ESM.tif
Supplementary file1 Figure S1 Correlation coefficients, κ coefficients, and concordance rates between the PRO-CTCAE and SIS at T2. The forest plots show correlation coefficients between the PRO-CTCAE and SIS at T1. κ coefficients and concordance rates are also shown. A, amount; CC: correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient-reported outcome; ROC, rate of concordance; S, severity (TIF 128 KB)
12282_2023_1480_MOESM2_ESM.tif
Supplementary file2 Figure S2 Correlation coefficients, κ coefficients, and concordance rates between the PRO-CTCAE and SIS at T1 in the PRO-CTCAE group. The forest plots show correlation coefficients between the PRO-CTCAE and SIS at T1 in the PRO-CTCAE group. κ coefficients and concordance rates are also shown. A, amount; CC, correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient- reported outcome; ROC, rate of concordance; S, Severity (TIF 132 KB)
12282_2023_1480_MOESM3_ESM.tif
Supplementary file3 Figure S3 Correlation coefficients, κ coefficients, and concordance rates between the PRO-CTCAE and SIS questionnaires at T1 in the SIS group. The forest plots show correlation coefficients between the PRO-CTCAE and SIS at T1 in the SIS group. κ coefficient and concordance are also shown. A, amount; CC, correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient-reported outcome; ROC, rate of concordance; S, severity (TIF 132 KB)
12282_2023_1480_MOESM4_ESM.tif
Supplementary file4 Figure S4 Test-retest reliability between T1 and T2 in the PRO-CTCAE group. The forest plots show the κ coefficient and 95% confidence interval between T1 and T2 in the PRO-CTCAE group. Concordance rates are also shown. A, amount; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient-reported outcome; ROC, rate of concordance; S, severity (TIF 136 KB)
12282_2023_1480_MOESM5_ESM.tif
Supplementary file5 Figure S5 Test-retest reliability between T1 and T2 in the SIS group. The forest plots show κ coefficients and 95% confidence intervals between T1 and T2 in the SIS group. Concordance rates are also shown. A, amount;. CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient-reported outcome; ROC, rate of concordance; S, severity (TIF 136 KB)
12282_2023_1480_MOESM6_ESM.tif
Supplementary file6 Figure S6 Correlation coefficients for score changes from T1 to T3 between the PRO-CTCAE and SIS questionnaires in the anthracyline group. The forest plots show correlation coefficients of score changes from T1 to T3 between the PRO-CTCAE and SIS. A, amount; CC, correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient-reported outcome; S, severity (TIF 111 KB)
12282_2023_1480_MOESM7_ESM.tif
Supplementary file7 Figure S7 Correlation coefficients for score changes from T1 to T2 between the PRO-CTCAE and SIS questionnaires in the docetaxel group. The forest plots show correlation coefficients of score changes from T1 to T2 between the PRO-CTCAE and SIS. A, amount; CC, correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, Interference; P, presence/absence; PRO, patient-reported outcome; S, severity (TIF 111 KB)
12282_2023_1480_MOESM8_ESM.tif
Supplementary file8 Figure S8 Correlation coefficients for score changes from T1 to T3 between the PRO-CTCAE and SIS in the docetaxel group. The forest plots show correlation coefficient of score changes from T1 to T3 between the PRO-CTCAE and SIS. A, amount; CC, correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO: patient-reported outcome; S, severity (TIF 111 KB)
12282_2023_1480_MOESM9_ESM.tif
Supplementary file9 Figure S9 Correlation coefficients for score changes from T1 to T2 between the PRO-CTCAE and SIS in the paclitaxel group. The forest plots show correlation coefficients of score changes from T1 to T2 between the PRO-CTCAE and SIS. A, amount; CC, correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, Frequency; I, Interference; P, presence/absence; PRO, patient-reported outcome; S, severity (TIF 111 KB)
12282_2023_1480_MOESM10_ESM.tif
Supplementary file10 Figure S10 Correlation coefficients for score changes from T1 to T3 between the PRO-CTCAE and SIS in the paclitaxel group. The forest plots show the correlation coefficient of score changes from T1 to T3 between the PRO-CTCAE and SIS. A, amount; CC, corelation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient-reported outcome; S, severity (TIF 110 KB)
12282_2023_1480_MOESM11_ESM.tif
Supplementary file11 Figure S11 Correlation coefficients for score changes from T1 to T2 between the PRO-CTCAE and SIS in the endocrine cohort. The forest plots show correlation coefficients of score changes from T1 to T2 between the PRO-CTCAE and SIS. A, amount; CC, correlation coefficient; CI, confidence interval; SIS, Symptom Illustration Scale; F, frequency; I, interference; P, presence/absence; PRO, patient-reported outcome; S, severity (TIF 111 KB)
12282_2023_1480_MOESM12_ESM.tif
Supplementary file12 Figure S12 Questionnaire for the Symptom Illustration Scale v.1.0. English translations were added to the original Japanese version for publication: 5) Diarrhea, 6) Shortness of breath, 7) Swelling, 8) Rash, 9) Hair loss, 10) Numbness & tingling, 11) General pain, 12) Joint pain, 13) Insomnia, 14) Fatigue, 15) Anxious, 16) Vaginal discharge, 17) Vaginal dryness, and 18) Hot flashes, continued from Figure 4 (TIF 292 KB)
About this article
Cite this article
Suzuki, Y., Iwamoto, T., Uno, M. et al. Development and validation of a symptom illustration scale from the patient-reported outcome common terminology criteria for adverse events for patients with breast cancer. Breast Cancer 30, 856–868 (2023). https://doi.org/10.1007/s12282-023-01480-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-023-01480-3