Abstract
Background
Surgical decisions and methods of surgery highly influence long term QoL for breast cancer (BC) survivors. This study is aimed towards an exploration of the dynamic changes in quality of life (QoL), anxiety/depression status, and body image (BI) among women with BC who received a mastectomy compared with those receiving breast reconstruction (BR) within an 8-year follow-up period.
Methods
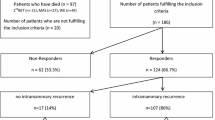
Women with major BC surgeries were invited to complete the World Health Organization Quality of Life–Brief (WHOQOL-BREF), the European quality of life five dimensions questionnaire (EQ-5D), and a body image scale within 8 years of surgery. Kernel smoothing methods were applied to describe dynamic changes in QoL, anxiety/depression, and BI at different time points. Linear mixed effects models were constructed to identify the interaction between time, different types of surgery, and the determinants of QoL in these patients.
Results
After 1:10 propensity score matching, a total of 741 women who had undergone a BR and mastectomy were included. The BR group exhibited a high WHOQOL QoL score one to five years after surgery with some fluctuations. The mastectomy group had comparatively stable QoL scores on WHOQOL items and were less depressed/anxious. The BR group generally showed fluctuating, higher BI scores two years after surgery, but they exhibited more anxiety/depression during follow up for 8 years. Medical comorbidities, the status of anxiety/depression, and BI were the major factors influencing all domains and items of the WHOQOL BREF among women with BC.
Conclusion
The mastectomy group showed a decreased trend toward depression in patients with BC. The BR group showed a significant improvement in QoL in the first 5 years with massive fluctuations. These findings should be considered and discussed in patient participatory decision-making and promotion of QoL for breast cancer survivors.



Similar content being viewed by others
Data availability
The database data used and analyzed during the current study are not publicly available due to confidentiality and regulations regarding personal electronic data protection but are available from the corresponding author after approval from the IRB of the National Cheng Kung University Hospital.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clinicians. 2021;71:209–49.
Lei S, Zheng R, Zhang S, Wang S, Chen R, Sun K, et al. Global patterns of breast cancer incidence and mortality: a population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. 2021;41:1183–94.
Society AC. Breast cancer facts & figures 2019–2020. Am Cancer Soc. 2019; 1–44.
Wu T-Y, Chang T-W, Chang S-M, Lin Y-Y, Wang J-D, Kuo Y-L. Dynamic changes of body image and quality of life in breast cancer patients. Cancer Manag Res. 2019;11:10563.
Wu TY, Chung CH, Lin CN, Hwang JS, Wang JD. Lifetime risks, loss of life expectancy, and health care expenditures for 19 types of cancer in Taiwan. Clin Epidemiol. 2018;10:581–91.
Gradishar WJ, Anderson BO, Balassanian R, Blair SL, Burstein HJ, Cyr A, et al. Breast cancer, version 4.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2018;16:310–20.
Miller AM, Steiner CA, Barrett ML, Fingar KR, Elixhauser A. Breast reconstruction surgery for mastectomy in hospital inpatient and ambulatory settings, 2009–2014: statistical brief# 228. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs (Rockville, MD: Agency for Healthcare Research and Quality (US)). 2017: 1–28.
Bland KI, Chang HR, Copeland EM III. Modified radical mastectomy and simple mastectomy. In: The breast. Amsterdam: Elsevier; 2018. p. 443- 61.e3.
Doherty C, Pearce S, Baxter N, Knowles S, Ross D, McClure JA, et al. Trends in immediate breast reconstruction and radiation after mastectomy: a population study. Breast J. 2020;26:446–53.
Politi MC, Lee CN, Philpott-Streiff SE, Foraker RE, Olsen MA, Merrill C, et al. A randomized controlled trial evaluating the BREASTChoice tool for personalized decision support about breast reconstruction after mastectomy. Ann Surg. 2020;271:230–7.
Honkanen N, Mustonen L, Kalso E, Meretoja T, Harno H. Breast reconstruction after breast cancer surgery—persistent pain and quality of life 1–8 years after breast reconstruction. Scand J Pain. 2021;21:522–9.
Chetrit A, Ben-Avraham S, Mandelzweig L, Amitai T, Danieli NS, Silverman B, et al. Breast cancer survivors: physical and mental quality of life 10 years following diagnosis, a case-control study. Breast Cancer Res Treat. 2021. https://doi.org/10.1007/s10549-021-06156-0.
Chen W-L, Chen Y-Y, Wu W-T, Ho C-L, Wang C-C. Life expectancy estimations and determinants of return to work among cancer survivors over a 7-year period. Sci Rep. 2021;11:1–12.
Gonzalez L, Bardach A, Palacios A, Peckaitis C, Ciapponi A, Pichón-Riviere A, et al. Health-related quality of life in patients with breast cancer in Latin America and the Caribbean: a systematic review and meta-analysis. Oncologist. 2021;26:e794–806.
Marinkovic M, Djordjevic N, Djordjevic L, Ignjatovic N, Djordjevic M, Karanikolic V. Assessment of the quality of life in breast cancer depending on the surgical treatment. Support Care Cancer. 2021;29:3257–66.
Mazo C, Kearns C, Mooney C, Gallagher WM. Clinical decision support systems in breast cancer: a systematic review. Cancers. 2020;12:369.
Dauplat J, Kwiatkowski F, Rouanet P, Delay E, Clough K, Verhaeghe J, et al. Quality of life after mastectomy with or without immediate breast reconstruction. J Br Surg. 2017;104:1197–206.
Thorarinsson A, Fröjd V, Kölby L, Ljungdal J, Taft C, Mark H. Long-term health-related quality of life after breast reconstruction: comparing 4 different methods of reconstruction. Plast Reconstruct Surg Glob Open. 2017;5:e1316.
Słowik AJ, Jabłoński MJ, Michałowska-Kaczmarczyk AM, Jach R. Evaluation of quality of life in women with breast cancer, with particular emphasis on sexual satisfaction, future perspectives and body image, depending on the method of surgery. Psychiatr Pol. 2017;51:871–88.
Campbell-Enns HJ, Woodgate RL. The psychosocial experiences of women with breast cancer across the lifespan: a systematic review. Psychooncology. 2017;26:1711–21.
Maguire G, Lee E, Bevington D, Küchemann C, Crabtree R, Cornell C. Psychiatric problems in the first year after mastectomy. Br Med J. 1978;1:963–5.
Fanakidou I, Zyga S, Alikari V, Tsironi M, Stathoulis J, Theofilou P. Mental health, loneliness, and illness perception outcomes in quality of life among young breast cancer patients after mastectomy: the role of breast reconstruction. Qual Life Res. 2018;27:539–43.
Zhang Q, Zhao H, Zheng Y. Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients—a systematic review and meta-analysis. Support Care Cancer. 2019;27:771–81.
Moshina N, Falk R, Hofvind S. Long-term quality of life among breast cancer survivors eligible for screening at diagnosis: a systematic review and meta-analysis. Public Health. 2021;199:65–76.
Domenici L, Caputo GG, Losco L, Di Taranto G, Lo Torto F, Pierazzi DM, et al. Muscle-sparing skin-reducing breast reconstruction with pre-pectoral implants in breast cancer patients: long-term assessment of patients’ satisfaction and quality of life. J Investig Surg. 2021. https://doi.org/10.1080/08941939.2021.1923874.
Archangelo SDCV, Sabino Neto M, Veiga DF, Garcia EB, Ferreira LM. Sexuality, depression and body image after breast reconstruction. Clinics. 2019;74:883.
Eltahir Y, Werners LL, Dreise MM, van Emmichoven IAZ, Jansen L, Werker PM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. 2013;132:201e-e209.
Fang S-Y, Chang H-T, Shu B-C. Objectified body consciousness, body image discomfort, and depressive symptoms among breast cancer survivors in Taiwan. Psychol Women Q. 2014;38:563–74.
Padmalatha S, Tsai Y-T, Ku H-C, Wu Y-L, Yu T, Fang S-Y, et al. Higher risk of depression after total mastectomy versus breast reconstruction among adult women with breast cancer: a systematic review and metaregression. Clin Breast Cancer. 2021;21:e526–38.
Ho PJ, Gernaat SA, Hartman M, Verkooijen HM. Health-related quality of life in Asian patients with breast cancer: a systematic review. BMJ Open. 2018;8: e020512.
Yang S-C, Kuo C-W, Lai W-W, Lin C-C, Su W-C, Chang S-M, et al. Dynamic changes of health utility in lung cancer patients receiving different treatments: a 7-year follow-up. J Thorac Oncol. 2019;14:1892–900.
Kao Y-L, Ou C-H, Lin S-H, Chang S-M, Wang J-D, Tsai Y-S. Dynamic changes of generic quality of life after different treatments for localized prostate cancer. J Clin Med. 2021;10:158.
Pirnia B, Homayounfar N, Hosseini N, Ebrahimi F, Haj Sadeghi Z, Malekanmehr P. The predictive role of body image and sexual function in quality of life after modified radical mastectomy regarding the mediating role of emotion; a cross sectional study. Int J Cancer Manag. 2020. https://doi.org/10.5812/ijcm.101371.
Group W. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28:551–8.
Group W. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9.
Yao G, Chung C-W, Yu C-F, Wang J-D. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J Formos Med Assoc. 2002;101:342–51.
Lin C-Y, Hwang J-S, Wang W-C, Lai W-W, Su W-C, Wu T-Y, et al. Psychometric evaluation of the WHOQOL-BREF, Taiwan version, across five kinds of Taiwanese cancer survivors: Rasch analysis and confirmatory factor analysis. J Formos Med Assoc. 2019;118:215–22.
Yao G, Wu C-H. Factorial invariance of the WHOQOL-BREF among disease groups. Qual Life Res. 2005;14:1881–8.
Hwang J-S, Wang J-D. Integrating health profile with survival for quality of life assessment. Qual Life Res. 2004;13:1–10.
Pickard AS, Ray S, Ganguli A, Cella D. Comparison of FACT- and EQ-5D-based utility scores in cancer. Value in Health. 2012;15:305–11.
Tachi T, Teramachi H, Tanaka K, Asano S, Osawa T, Kawashima A, et al. The impact of outpatient chemotherapy-related adverse events on the quality of life of breast cancer patients. PLoS One. 2015;10: e0124169.
Lee H-Y, Hung M-C, Hu F-C, Chang Y-Y, Hsieh C-L, Wang J-D. Estimating quality weights for EQ-5D (EuroQol-5 dimensions) health states with the time trade-off method in Taiwan. J Formos Med Assoc. 2013;112:699–706.
Claessens AK, Ramaekers BL, Lobbezoo DJ, van Kampen RJ, de Boer M, van de Wouw AJ, et al. Quality of life in a real-world cohort of advanced breast cancer patients: a study of the SONABRE Registry. Qual Life Res. 2020;29:3363–74.
Hopwood P, Fletcher I, Lee A, Al GS. A body image scale for use with cancer patients. Eur J Cancer. 2001;37:189–97.
Spatuzzi R, Vespa A, Lorenzi P, Miccinesi G, Ricciuti M, Cifarelli W, et al. Evaluation of social support, quality of life, and body image in women with breast cancer. Breast Care. 2016;11:28–32.
Yang S-C, Lin C-C, Lai W-W, Chang S-M, Hwang J-S, Su W-C, et al. Dynamic changes in quality of life after three first-line therapies for EGFR mutation-positive advanced non-small-cell lung cancer. Ther Adv Med Oncol. 2018;10:1758834018755072.
Ahern TP, Lash TL, Thwin SS, Silliman RA. Impact of acquired comorbidities on all-cause mortality rates among older breast cancer survivors. Med Care. 2009;47:73.
Moradzadeh R, Mansournia MA, Baghfalaki T, Ghiasvand R, Noori-Daloii MR, Holakouie-Naieni K. Misclassification adjustment of family history of breast cancer in a case-control study: a Bayesian approach. Asian Pac J Cancer Prev. 2016;16:8221–6.
Li R, Daniel R, Rachet B. How much do tumor stage and treatment explain socioeconomic inequalities in breast cancer survival? Applying causal mediation analysis to population-based data. Eur J Epidemiol. 2016;31:603–11.
Miller AM, Steiner CA, Barrett ML, Fingar KR, Elixhauser A. Breast reconstruction surgery for mastectomy in hospital inpatient and ambulatory settings, 2009–2014: statistical brief# 228. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs (Rockville, MD: Agency for Healthcare Research and Quality (US)). 2017: 1–28
Siegel EL, Whiting J, Kim Y, Sun W, Laronga C, Lee MC. Effect of surgical complications on outcomes in breast cancer patients treated with mastectomy and immediate reconstruction. Breast Cancer Res Treat. 2021;188:641–8.
Riggio AI, Varley KE, Welm AL. The lingering mysteries of metastatic recurrence in breast cancer. Br J Cancer. 2021;124:13–26.
Trayes KP, Cokenakes SE. Breast cancer treatment. Am Fam Physician. 2021;104:171–8.
Lavdaniti M, Owens DA, Liamopoulou P, Marmara K, Zioga E, Mantzanas MS, et al. Factors influencing quality of life in breast cancer patients six months after the completion of chemotherapy. Diseases. 2019;7:26.
Tsai HY, Kuo RNC, Chung KP. Quality of life of breast cancer survivors following breast-conserving therapy versus mastectomy: a multicenter study in Taiwan. Jpn J Clin Oncol. 2017;47:909–18.
Huang C-C, Lien H-H, Tu S-H, Huang C-S, Jeng J-Y, Chao H-L, et al. Quality of life in Taiwanese breast cancer survivors with breast-conserving therapy. J Formos Med Assoc. 2010;109:493–502.
Hung YN, Liu TW, Wen FH, Chou WC, Tang ST. Escalating health care expenditures in cancer decedents’ last year of life: a decade of evidence from a retrospective population-based cohort study in Taiwan. Oncologist. 2017;22:460.
Siegel EL, Whiting J, Kim Y, Sun W, Laronga C, Lee MC. Effect of surgical complications on outcomes in breast cancer patients treated with mastectomy and immediate reconstruction. Breast Cancer Res Treat. 2021;188:1–8.
Gangane N, Khairkar P, Hurtig A-K, San SM. Quality of life determinants in breast cancer patients in central rural India. Asian Pac J Cancer Prev APJCP. 2017;18:3325.
Coombes RC, Tovey H, Kilburn L, Mansi J, Palmieri C, Bartlett J, et al. Effect of celecoxib vs placebo as adjuvant therapy on disease-free survival among patients with breast cancer: the REACT randomized clinical trial. JAMA Oncol. 2021;7:1291–301.
de Boniface J, Szulkin R, Johansson AL. Survival after breast conservation vs mastectomy adjusted for comorbidity and socioeconomic status: a swedish national 6-year follow-up of 48 986 women. JAMA Surg. 2021;56:69.
Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104:386–405.
Siqueira HFF, de Almeida Teixeira JL, da Silva Lessa Filho R, Hora EC, Brasileiro FF, de Souza Borges K, et al. Patient satisfaction and quality of life in breast reconstruction: assessment of outcomes of immediate, delayed, and nonreconstruction. BMC Res Notes. 2020;13:1–7.
Hojan K. Does the weight of an external breast prosthesis play an important role for women who undergone mastectomy? Rep Pract Oncol Radiother. 2020;25:574–8.
Qiu J, Hou S, Li P, Huang L. Medical professionals’ knowledge of the use of external breast prostheses among breast cancer patients in China—a cross-sectional study. Gland Surg. 2021;10:595.
Anishya A, Appavu S. External breast prosthesis for post mastectomy women. Asian J Nurs Educ Res. 2021;11:427–30.
Taghian NR, Miller CL, Jammallo LS, O’Toole J, Skolny MN. Lymphedema following breast cancer treatment and impact on quality of life: a review. Crit Rev Oncol Hematol. 2014;92:227–34.
Jørgensen MG, Toyserkani NM, Hansen FG, Bygum A, Sørensen JA. The impact of lymphedema on health-related quality of life up to 10 years after breast cancer treatment. NPJ Breast Cancer. 2021;7:1–8.
Togawa K, Ma H, Smith AW, Neuhouser ML, George SM, Baumgartner KB, et al. Self-reported symptoms of arm lymphedema and health-related quality of life among female breast cancer survivors. Sci Rep. 2021;11:1–13.
El Haidari R, Abbas LA, Nerich V, Anota A. Factors associated with health-related quality of life in women with breast cancer in the Middle East: a systematic review. Cancers. 2020;12:696.
Zhou K, Wang W, Li M, An J, Huo L, He X, et al. Body image mediates the relationship between post-surgery needs and health-related quality of life among women with breast cancer: a cross-sectional study. Health Qual Life Outcomes. 2020;18:1–11.
Okati-Aliabad H, Ansari-Moghadam A, Mohammadi M, Kargar S, Shahraki-Sanavi F. The prevalence of anxiety and depression and its association with coping strategies, supportive care needs, and social support among women with breast cancer. Suppor Care Cancer. 2021;30:1–8.
Park J, Rodriguez JL, O’Brien KM, Nichols HB, Hodgson ME, Weinberg CR, et al. Health-related quality of life outcomes among breast cancer survivors. Cancer. 2021;127:1114–25.
Lu I-C, Jean M-CY, Lei S-M, Cheng H-H, Wang J-D. BSRS-5 (5-tem Brief Symptom Rating Scale) scores affect every aspect of quality of life measured by WHOQOL-BREF in healthy workers. Qual Life Res. 2011;20:1469–75.
Chang Y-C, Yao G, Hu SC, Wang J-D. Depression affects the scores of all facets of the WHOQOL-BREF and may mediate the effects of physical disability among community-dwelling older adults. PLoS One. 2015;10: e0128356.
Marsh S, Borges VF, Coons HL, Afghahi A. Sexual health after a breast cancer diagnosis in young women: clinical implications for patients and providers. Breast Cancer Res Treat. 2020;184:1–9.
Franzoi MA, Agostinetto E, Perachino M, Del Mastro L, de Azambuja E, Vaz-Luis I, et al. Evidence-based approaches for the management of side-effects of adjuvant endocrine therapy in patients with breast cancer. Lancet Oncol. 2021;22:e303–13.
Colomo N, Olveira C, Hernández-Pedrosa J, Bergero T, Fábrega-Ruz J, Porras N, et al. Validity of self-rating screening scales for the diagnosis of depression and anxiety in adult patients with bronchiectasis. Archivos de Bronconeumología (English Edition). 2021;57:179–85.
Acknowledgements
I am especially indebted to the National Cheng Kung university to support funding for my studies. Also, I wish to express my appreciation for those who had helped with the English editing of the manuscript.
Funding
The collection of patient’s reported outcome data was supported by serial grants from the Ministry of Science and Technology (MOST 108-2627-M-006-001, MOST 109-2621-M-006-007, MOST 110-2627-M-006-010). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: SPKM, N-YK, J-DW, S-YF; methodology: SPKM, N-YK, J-DW, S-YF; formal analysis and investigation: SPKm, SK, Y-LW, CCC, C-NL. Writing—original draft preparation: SPKM; writing—review and editing: H-CK, Y-TT, SK, N-YKJ-DW, S-YF; funding acquisition: SPKM, N-YK, J-DW; resources: SPKM, N-YK; supervision: N-YK, J-DW, S-YF.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by The Institutional Review Board of the National Cheng Kung University Hospital before initiation (review No: B-ER-110–050).
Informed consent
Informed consent was obtained from every patient before adding the data to the database.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Konara Mudiyanselage, S.P., Wu, YL., Kukreti, S. et al. Dynamic changes in quality of life, psychological status, and body image in women who underwent a mastectomy as compared with breast reconstruction: an 8-year follow up. Breast Cancer 30, 226–240 (2023). https://doi.org/10.1007/s12282-022-01413-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-022-01413-6