Abstract
Background
The link between Epstein-Barr Virus (EBV) and breast cancer (BC) etiology remains unclear. We utilized the Health of Women (HOW) Study® to understand the association between infectious mononucleosis (IM), a surrogate for EBV infection, and invasive BC.
Methods
The HOW Study® was a web-based survey of BC risk factors with > 40, 000 participants; 183 had IM at < 10 years old, 3, 654 had IM between 10 and 22 years old, 764 had IM at > 22 years old, and 17, 026 never developed IM. Of these 21, 627 women, 2093 had Stages I–III BC and 14, 143 were cancer-free. Binary logistic regression ascertained the association between IM and invasive BC risk by controlling for confounders.
Results
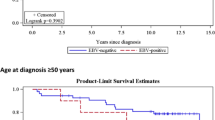
A history of IM was associated with a lower likelihood of developing invasive BC compared to women who did not develop IM (adjusted OR = 0.83, 95% CI 0.72–0.94). That finding was driven by women who had IM between 10 and 22 years old (adjusted OR = 0.83, 95% CI 0.72–0.97) albeit no linear association between age at developing IM and breast cancer (p-trend > 0.05). Women who had IM between 10 and 22 years old were less likely to develop estrogen receptor positive (ER+ ; adjusted OR = 0.84, 95% CI 0.71–0.99) or hormone receptor positive (HR+ ; adjusted OR = 0.86, 95% CI 0.73–1.01) BC. There was no association between IM and ER− or HR− BC.
Conclusion
In the HOW Study®, women diagnosed with IM between the ages of 10 and 22 had a lower risk of developing invasive BC compared to women who never developed IM.
Similar content being viewed by others
References
Cohen JI. Epstein-Barr virus infection. N Engl J Med. 2000;343:481–92.
Evans A. The spectrum of infections with Epstein-Barr virus: a hypothesis. J Infect Dis. 1971;124:330–7.
Kapatai G, Murray P. Contribution of the Epstein-Barr virus to the molecular pathogenesis of Hodgkin lymphoma. J Clin Pathol. 2007;60:1342–9.
Epstein MA, Barr YM. Cultivation in vitro of human lymphoblasts from Burkitt’s malignant lymphoma. Lancet. 1964;283:252–3.
Bass AJ, et al. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–9.
Wolf H, et al. Attempts to detect virus-specific DNA sequences in human tumors – III. Epstein-Barr viral DNA in non-lymphoid nasopharyngeal carcinoma cells. Med Microbiol Immunol. 1975;161:15–21.
Khan G, Fitzmaurice C, Naghavi M, Ahmed LA. Global and regional incidence, mortality and disability-adjusted life-years for Epstein-Barr virus-attributable malignancies, 1990–2017. BMJ Open. 2020;10:e037505.
Labrecque LG, Barnes DM, Fentiman IS, Griffin BE. Epstein-Barr virus in epithelial cell tumors: A breast cancer study. Cancer Res. 1995;55:39–45.
Murray PG, et al. Reactivity with a monoclonal antibody to Epstein-Barr virus (EBV) nuclear antigen 1 defines a subset of aggressive breast cancers in the absence of the EBV genome. Cancer Res. 2003;63:2338–43.
Peng J, et al. Multiplex PCR/mass spectrometry screening of biological carcinogenic agents in human mammary tumors. J Clin Virol. 2014;61:255–9.
Chu PG, Chang KL, Chen YY, Chen WG, Weiss LM. No significant association of Epstein-Barr virus infection with invasive breast carcinoma. Am J Pathol. 2001;159:571–8.
Herrmann K, Niedobitek G. Lack of evidence for an association of Epstein-Barr virus infection with breast carcinoma. Breast Cancer Res. 2002;5:R13.
Joshi D, Quadri M, Gangane N, Joshi R, Gangane N. Association of epstein barr virus infection (ebv) with breast cancer in rural Indian women. PLoS ONE. 2009;4:e8180.
Glashr SL, Ambinder RF, Digiuseppe JA, Horn-Ross PL, Hsu JL. Absence of Epstein-Barr virus EBER-1 transcripts in an epidemiologically diverse group of breast cancers. Int J Cancer. 1998;75:555–8.
Deshpande CG, Badve S, Kidwai N, Longnecker R. Lack of expression of the epstein-barr virus (ebv) gene products, ebers, ebna1, lmp1, and lmp2a, in breast cancer cells. Lab Investig. 2002;82:1193–9.
Pai T, et al. Evidence for the association of Epstein-Barr Virus in breast cancer in Indian patients using in-situ hybridization technique. Breast J. 2018;24:16–22.
Bonnet M, et al. Detection of Epstein-Barr virus in invasive breast cancers. J Natl Cancer Inst. 1999;91:1376–81.
Hu H, et al. Epstein-Barr virus infection of mammary epithelial cells promotes malignant transformation. EBioMedicine. 2016;9:148–60.
Arbach H, et al. Epstein-Barr virus (EBV) genome and expression in breast cancer tissue: effect of EBV infection of breast cancer cells on resistance to paclitaxel (taxol). J Virol. 2006;80:845–53.
Mostafaei S, et al. The role of Epstein-Barr virus-expressed genes in breast cancer development. Breast J. 2020;26:2323–6.
Nagi K, et al. High-risk human papillomaviruses and Epstein-Barr virus in breast cancer in Lebanese women and their association with tumor grade: a molecular and tissue microarray study. Cancer Cell Int. 2021;21:13.
Morales-Sánchez A, et al. No association between Epstein-Barr virus and mouse mammary tumor virus with breast cancer in Mexican women. Sci Rep. 2013;3:2970.
Preciado MV, et al. Epstein-Barr virus in breast carcinoma in Argentina. Arch Pathol Lab Med. 2005;129:377–81.
Kadivar M, Monabati A, Joulaee A, Hosseini N. Epstein-Barr virus and breast cancer: lack of evidence for an association in Iranian women. Pathol Oncol Res. 2011;17:489–92.
Fina F, et al. Frequency and genome load of Epstein-Barr virus in 509 breast cancers from different geographical areas. Br J Cancer. 2001;84:783–90.
Hachana M, et al. Investigation of Epstein-Barr virus in breast carcinomas in Tunisia. Pathol Res Pract. 2011;207:695–700.
Huo Q, Zhang N, Yang Q. Epstein-Barr virus infection and sporadic breast cancer risk: a meta-analysis. PLoS ONE. 2012;7:e31656.
Farahmand M, et al. Epstein-Barr virus and risk of breast cancer: a systematic review and meta-analysis. Futur Oncol. 2019;15:2873–85.
Jin Q, Su J, Yan D, Wu S. Epstein-Barr virus infection and increased sporadic breast carcinoma risk: a meta-analysis. Med Princ Pract. 2020;29:195–200.
Yasui Y, et al. Breast cancer risk and ‘delayed’ primary Epstein-Barr virus infection. Cancer Epidemiol Biomark Prevent. 2001;10:9–16.
Hjalgrim H, et al. Risk of Hodgkin’s disease and other cancers after infectious mononucleosis. J Natl Cancer Inst. 2000;92:1522–8.
Massa J, et al. Infectious mononucleosis and risk of breast cancer in a prospective study of women. Cancer Causes Control. 2012;23:1893–8.
Guida JL, et al. The Health of Women (HOW) Study®: a web-based survey of breast cancer risk factors, diagnosis, and treatment. J Cancer Surviv (in press). 2022. https://doi.org/10.1007/s11764-022-01180-5.
Pender MP. Infection of autoreactive B lymphocytes with EBV, causing chronic autoimmune diseases. Trends Immunol. 2003;24:584–8.
Schairer C, Pfeiffer RM, Gadalla SM. Autoimmune diseases and breast cancer risk by tumor hormone-receptor status among elderly women. Int J Cancer. 2018;142:1202–8.
Hardefeldt PJ, Eslick GD, Edirimanne S. Benign thyroid disease is associated with breast cancer: a meta-analysis. Breast Cancer Res Treat. 2012;133:1169–77.
Glaser SL. Correspondence re: Yasui et al., Breast cancer risk and “delayed” primary Epstein-Barr virus infection. 10: 9–16, 2001. Cancer Epidemiol Prevent Biomark. 2003;12:16.
Montoya-Ferrer A, et al. Clinical and biological factors associated with early Epstein-Barr virus infection in human immunodeficiency virus-exposed uninfected infants in eastern Uganda. Clin Infect Dis. 2021;72:1026–32.
Albonico HU, Bräker HU, Hüsler J. Febrile infectious childhood diseases in the history of cancer patients and matched controls. Med Hypotheses. 1998;51:315–20.
Hirth JM, Laz TH, Rahman M, Berenson AB. Racial/ethnic differences affecting adherence to cancer screening guidelines among women. J Women’s Heal. 2016;25:371–80.
Acknowledgements
We thank the staff and participants of the HOW Study ® and the Dr. Susan Love Research Foundation for providing this dataset. GMW is supported by the AVON Foundation, the Breast Cancer Research Foundation, and the Ludwig Center at Harvard Medical School. We thank Leah Eshraghi and Katherine M. Peterson for reading this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Heng, Y.J., Love, S., DeHart, J.C. et al. The association of infectious mononucleosis and invasive breast cancer in The Health of Women (HOW) Study®. Breast Cancer 29, 731–739 (2022). https://doi.org/10.1007/s12282-022-01351-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-022-01351-3