Abstract
Purpose
To evaluate the overall survival prognostic value of preoperative 18F-fluorodeoxyglucose positron emission tomography (PET) in breast cancer, as compared with the lymph node ratio (LNR).
Methods
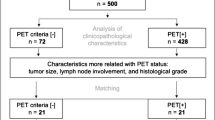
Data were abstracted at a median follow-up 14.7 years from a retrospective cohort of 104 patients who underwent PET imaging before curative surgery. PET-Axillary|Sternal was classified as PET-positive if hypermetabolism was visualized in ipsilateral nodal axillary and/or sternal region, else as PET-negative. The differences of 15 years restricted mean survival time ∆RMST according to PET and LNR were computed from Kaplan–Meier overall survival. The effect of PET and other patients' characteristics was analyzed through rankit normalization, which provides with Cox regression the Royston–Sauerbrei D measure of separation to compare the characteristics (0 indicating no prognostic value). Multivariate analysis of the normalized characteristics used stepwise selection with the Akaike information criterion.
Results
In Kaplan–Meier analysis, LNR > 0.20 versus ≤ 0.20 showed ∆RMST = 3.4 years, P = 0.003. PET-Axillary|Sternal positivity versus PET-negative showed a ∆RMST = 2.6 years, P = 0.008. In Cox univariate analyses, LNR appeared as topmost prognostic separator, D = 1.50, P < 0.001. PET ranked below but was also highly significant, D = 1.02, P = 0.009. In multivariate analyses, LNR and PET-Axillary|Sternal were colinear and mutually exclusive. PET-Axillary|Sternal improved as prognosticator in a model excluding lymph nodes, yielding a normalized hazard ratio of 2.44, P = 0.062.
Conclusion
Pathological lymph node assessment remains the gold standard of prognosis. However, PET appears as a valuable surrogate in univariate analysis at 15-year follow-up. There was a trend towards significance in multivariate analysis that warrants further investigation.



Similar content being viewed by others
Data availability
Data is available on Mendeley. Temporary link for review: https://data.mendeley.com/datasets/sfvtmrd8z9/draft?a=f1f1fe69-2387-4d9a-92ca-e564faa046de. Reserved https://doi.org/10.17632/sfvtmrd8z9.1.
Protocol availability
The protocol is available at: https://www.protocols.io/view/pet2015uz-prognostic-value-of-pre-treatment-18fdg-bf7jjrkn/abstract. http://www.isrctn.com/ISRCTN17962845.
Code availability
The study used software applications available at: https://cran.r-project.org/. Function rnktt is available in Appendix A and shared with the data at: reserved https://doi.org/10.17632/sfvtmrd8z9.1.
References
Kurihara H, Shimizu C, Miyakita Y, Yoshida M, Hamada A, Kanayama Y, et al. Molecular imaging using PET for breast cancer. Breast Cancer. 2016;23:24–32.
Jung NY, Kim SH, Kang BJ, Park SY, Chung MH. The value of primary tumor (18)F-FDG uptake on preoperative PET/CT for predicting intratumoral lymphatic invasion and axillary nodal metastasis. Breast Cancer. 2016;23:712–7.
Vinh-Hung V, Everaert H, Lamote J, Voordeckers M, van Parijs H, Vanhoeij M, et al. Diagnostic and prognostic correlates of preoperative FDG PET for breast cancer. Eur J Nucl Med Mol Imaging. 2012;39:1618–27.
Vinh-Hung V, Everaert H, Farid K, Djassemi N, Baudin-Veronique J, Bougas S, et al. Preoperative [18]fluorodeoxyglucose-positron emission tomography/computed tomography in early stage breast cancer: rates of distant metastases. World J Radiol. 2017;9:312–20.
Diao W, Tian F, Jia Z. The prognostic value of SUVmax measuring on primary lesion and ALN by (18)F-FDG PET or PET/CT in patients with breast cancer. Eur J Radiol. 2018;105:1–7.
Wen W, Xuan D, Hu Y, Li X, Liu L, Xu D. Prognostic value of maximum standard uptake value, metabolic tumor volume, and total lesion glycolysis of positron emission tomography/computed tomography in patients with breast cancer: a systematic review and meta-analysis. PLoS ONE. 2019;14:e0225959.
Vinh-Hung V, Verschraegen C, Promish DI, Cserni G, Van de Steene J, Tai P, et al. Ratios of involved nodes in early breast cancer. Breast Cancer Res. 2004;6:R680–8.
Liu D, Chen Y, Deng M, Xie G, Wang J, Zhang L, et al. Lymph node ratio and breast cancer prognosis: a meta-analysis. Breast Cancer. 2014;21:1–9.
Bral S, Vinh-Hung V, Everaert H, De Coninck P, Storme G. The use of molecular imaging to evaluate radiation fields in the adjuvant setting of breast cancer—a feasibility study. Strahlenther Onkol. 2008;184:100–4.
Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81.
Irwin JO. The standard error of an estimate of expectation of life, with special reference to expectation of tumourless life in experiments with mice. J Hyg (Lond). 1949;47:188.
Royston P, Parmar MK. Restricted mean survival time: an alternative to the hazard ratio for the design and analysis of randomized trials with a time-to-event outcome. BMC Med Res Methodol. 2013;13:152.
Royston P, Sauerbrei W. A new measure of prognostic separation in survival data. Stat Med. 2004;23:723–48.
Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19:716–23.
Venables WN, Ripley BD. Modern applied statistics with S. In: Chambers J, Eddy W, Hardle W, editors. Statistics and computing, vol. 4. Springer: New York; 2002. p. 172–6.
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. 2020; R version 3.6.3.
van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–42.
Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model (Statistics for biology and health). New York: Springer; 2000. p. 87–152.
Liu C, Li H, Zhuo R, Wang L, He L, Ruan Q, et al. Grade-lymph node ratio predicts the survival of breast cancer in different molecular types: a surveillance, epidemiology, and end results population-based analysis. Medicine (Baltimore). 2019;98:e16436.
Stephen J, Murray G, Cameron DA, Thomas J, Kunkler IH, Jack W, et al. Time dependence of biomarkers: non-proportional effects of immunohistochemical panels predicting relapse risk in early breast cancer. Br J Cancer. 2014;111:2242–7.
Keam B, Im SA, Koh Y, Han SW, Oh DY, Cho N, et al. Predictive value of FDG PET/CT for pathologic axillary node involvement after neoadjuvant chemotherapy. Breast Cancer. 2013;20:167–73.
Ipsen J, Jerne NK. Graphical evaluation of the distribution of small experimental series. Acta Pathol Microbiol Scand. 1944;21:343–61.
Ulaner GA, Juarez J, Riedl CC, Goldman DA. (18)F-FDG PET/CT for systemic staging of newly diagnosed breast cancer in men. J Nucl Med. 2019;60:472–7.
Choi BB, Lee JS, Kim KH. Association between MRI features and standardized uptake value of 18F-FDG PET/CT in triple-negative breast cancer. Oncol Res Treat. 2018;41:706–11.
Higuchi T, Fujimoto Y, Ozawa H, Bun A, Fukui R, Miyagawa Y, et al. Significance of metabolic tumor volume at baseline and reduction of mean standardized uptake value in (18)F-FDG-PET/CT imaging for predicting pathological complete response in breast cancers treated with preoperative chemotherapy. Ann Surg Oncol. 2019;26:2175–83.
Evangelista L, Cervino AR, Michieletto S, Saibene T, Ghiotto C, Guarneri V, et al. Diagnostic and prognostic impact of fluorine-18-fluorodeoxyglucose PET/CT in preoperative and postoperative setting of breast cancer patients. Nucl Med Commun. 2017;38:537–45.
Vinh-Hung V, Leduc N, Baudin J, Storme G, Nguyen NP, Joachim C, et al. Axillary lymph node involvement in breast cancer: a random walk model of tumor burden. Cureus. 2019;11:e6249.
Tokes T, Kajary K, Szentmartoni G, Lengyel Z, Gyorke T, Torgyik L, et al. Predictive and prognostic value of FDG-PET/CT imaging and different response evaluation criteria after primary systemic therapy of breast cancer. Breast Cancer. 2017;24:137–46.
Nakano Y, Noguchi M, Yokoi-Noguchi M, Ohno Y, Morioka E, Kosaka T, et al. The roles of (18)F-FDG-PET/CT and US-guided FNAC in assessment of axillary nodal metastases in breast cancer patients. Breast Cancer. 2017;24:121–7.
Hayashi M, Murakami K, Oyama T, Domeki Y, Hagiwara S, Katsumata D, et al. PET/CT supports breast cancer diagnosis and treatment. Breast Cancer. 2008;15:224–30.
Razek AA, Lattif MA, Denewer A, Farouk O, Nada N. Assessment of axillary lymph nodes in patients with breast cancer with diffusion-weighted MR imaging in combination with routine and dynamic contrast MR imaging. Breast Cancer. 2016;23:525–32.
Kato F, Kudo K, Yamashita H, Baba M, Shimizu A, Oyama-Manabe N, et al. Predicting metastasis in clinically negative axillary lymph nodes with minimum apparent diffusion coefficient value in luminal A-like breast cancer. Breast Cancer. 2019;26:628–36.
Murakami W, Tozaki M, Nakamura S, Ide Y, Inuzuka M, Hirota Y, et al. The clinical impact of MRI screening for BRCA mutation carriers: the first report in Japan. Breast Cancer. 2019;26:552–61.
Izumori A, Kokubu Y, Sato K, Gomi N, Morizono H, Sakai T, et al. Usefulness of second-look ultrasonography using anatomical breast structures as indicators for magnetic resonance imaging-detected breast abnormalities. Breast Cancer. 2020;27:129–39.
Nakashima K, Uematsu T, Takahashi K, Nishimura S, Tadokoro Y, Hayashi T, et al. Does breast cancer growth rate really depend on tumor subtype? Measurement of tumor doubling time using serial ultrasonography between diagnosis and surgery. Breast Cancer. 2019;26:206–14.
Nagasaka K, Satake H, Ishigaki S, Kawai H, Naganawa S. Histogram analysis of quantitative pharmacokinetic parameters on DCE-MRI: correlations with prognostic factors and molecular subtypes in breast cancer. Breast Cancer. 2019;26:113–24.
Yuen S, Monzawa S, Yanai S, Matsumoto H, Yata Y, Ichinose Y, et al. The association between MRI findings and breast cancer subtypes: focused on the combination patterns on diffusion-weighted and T2-weighted images. Breast Cancer. 2020;27:1029–37.
Nguyen-Thu H, Hanaoka H, Nakajima T, Yamaguchi A, Nguyen-Cong T, Kartamihardja AAP, et al. Early prediction of triple negative breast cancer response to cisplatin treatment using diffusion-weighted MRI and (18)F-FDG-PET. Breast Cancer. 2018;25:334–42.
Tabouret-Viaud C, Botsikas D, Delattre BM, Mainta I, Amzalag G, Rager O, et al. PET/MR in breast cancer. Semin Nucl Med. 2015;45:304–21.
Seo YY, Yoo IR, Park SY, Oh JK, Kim SH, Sohn HS. Ductal carcinoma in situ and ductal carcinoma in situ with microinvasion: correlation of FDG uptake with histological and biological prognostic factors. Breast Cancer. 2017;24:353–61.
Funding
The study received no funding.
Author information
Authors and Affiliations
Contributions
VVH and HE designed and conceptualized the study; VVH, HE and MDR drafted the study protocol; VVH and HE analyzed the PET-scan images; VVH, HVP, GV, MV, GS, CF, JL, and MDR contributed patients data; VVH, OG, NPN and CV analyzed the data and wrote the first draft; VVH, OG, HVP, GV, MV, GS, CF, JL, JP, KF, NPN, CV, and MDR revised the manuscript; all authors critically reviewed the manuscript and gave final approval.
Corresponding author
Ethics declarations
Conflict of interest
Vincent Vinh-Hung received non-financial support from AddMedica, AstraZeneca, Bayer HealthCare SAS, Bristol-Myers Squibb, Ipsen Pharma, Janssen-Cilag, GlaxoSmithKline, Pfizer SAS, Roche SAS, Sanofi Aventis France, Sepropharm International. Vincent Vinh-Hung and Nam P. Nguyen hold a patent on the Mean absolute dose deviation, unrelated to the present study. Olena Gorobets received non-financial support from AstraZeneca. The other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. The study was approved by the Medical Ethics Committee of the Universitair Ziekenhuis Brussel. Informed consent was obtained from all individual participants included in the study. The study was registered at: http://www.isrctn.com/ISRCTN17962845.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Vinh-Hung, V., Everaert, H., Gorobets, O. et al. Breast cancer preoperative 18FDG-PET, overall survival prognostic separation compared with the lymph node ratio. Breast Cancer 28, 956–968 (2021). https://doi.org/10.1007/s12282-021-01234-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-021-01234-z