Abstract
Background
To compare the breast cancer detection performance in digital mammograms of a panel of three unaided human readers (HR) versus a stand-alone artificial intelligence (AI)-based Transpara system in a population of Japanese women.
Methods
The subjects were 310 Japanese female outpatients who underwent digital mammographic examinations between January 2018 and October 2018. A panel of three HR provided a Breast Imaging Reporting and Data System (BI-RADS) score, and Transpara system provided an interactive decision support score and an examination-based cancer likelihood score. The area under the receiver operating characteristic curve (AUC), sensitivity, and specificity were compared under each of reading conditions.
Results
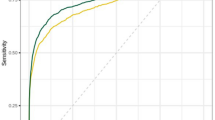
The AUC was higher for human readers than with stand-alone Transpara system (human readers 0.816; Transpara system 0.706; difference 0.11; P < 0.001). The sensitivity of the unaided HR for diagnosis was 89% and specificity was 86%. The sensitivity of stand-alone Transpara system for cutoff scores of 4 and 7 were 93% and 85%, and specificities were 45% and 67%, respectively.
Conclusions
Although the diagnostic performance of Transpara system was statistically lower than that of HR, the recent advances in AI algorithms are expected to reduce the difference between computers and human experts in detecting breast cancer.





Similar content being viewed by others
References
Fenton JJ, Taplin SH, Carney PA, Abraham L, Sickles EA, D’Orsi C, et al. Influence of computer-aided detection on performance of screening mammography. N Engl J Med. 2007;356:1399–409.
Lehman CD, Wellman RD, Buist DS, Kerlikowske K, Tosteson AN, Miglioretti DL, et al. Diagnostic accuracy of digital screening mammography with and without computer-aided detection. JAMA Intern Med. 2015;175:1828–37.
Litjens G, Kooi T, Bejnordi BE, Setio AAA, Ciompi F, Ghafoorian M, et al. A survey on deep learning in medical image analysis. Med Image Anal. 2017;42:60–88.
Wahab N, Khan A, Lee YS. Transfer learning based deep CNN for segmentation and detection of mitoses in breast cancer histopathological images. Microscopy. 2019;68:216–33.
Khan A, Sohail A, Zahoora U, Qureshi AS. A survey of the recent architectures of deep convolutional neural networks. arXiv. 2019; 1901.06032.
Geras K, Mann R, Moy L. Artificial intelligence for mammography and digital breast tomosynthesis: current concepts and future perspectives. Radiology. 2019;293:246–59.
Rodriguez-Ruiz A, La˚ng K, Gubern-Merida A, Broeders M, Gennaro G, Clauser P, et al. Stand-Alone Artificial Intelligence for Breast Cancer Detection in Mammography: Comparison With 101 Radiologists. J Natl Cancer Inst. 2019; 111: djy222
Rodríguez-Ruiz A, Krupinski E, Mordang JJ, Schilling K, Heywang-Köbrunner SH, Sechopoulos I, et al. Detection of breast cancer with mammography: effect of an artificial intelligence support system. Radiology. 2019;290:305–14.
Bria A, Karssemeijer N, Tortorella F. Learning from unbalanced data: a cascade-based approach for detecting clustered microcalcifications. Med Image Anal. 2014;18:241–52.
Kooi T, Litjens G, van Ginneken B, Gubern-Mérida A, Sánchez CI, Mann R, et al. Large scale deep learning for computer aided detection of mammographic lesions. Med Image Anal. 2017;35:303–12.
Hupse R, Karssemeijer N. Use of normal tissue context in computer-aided detection of masses in mammograms. IEEE Trans Med Imaging. 2009;28:2033–41.
Kanda Y. Investigation of the freely available easy-to-use soft- ware ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Karssemeijer N, Otten JDM, Roelofs AAJ, Woudenberg S, Hendriks JH. Effect of independent multiple reading of mammograms on detection performance. SPIE medical Imaging 2004.
Gur D, Bandos AI, Cohen CS, Cohen CS, Hakim CM, Hardesty LA, et al. The “laboratory” effect: comparing radiologists’ performance and variability during prospective clinical and laboratory mammography interpretations. Radiology. 2008;249:47–53.
Evans KK, Birdwell RL, Wolfe JM. If you don’t find it often, you often don’t find it: why some cancers are missed in breast cancer screening. PLoS ONE. 2013;8:e64366.
Acknowledgements
The author would like to thank Nico Karssemeijer, ScreenPoint Medical BV, Nijmegen, The Netherlands, for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alejandro Rodríguez-Ruiz is employee of ScreenPoint Medical BV, who provided crucial technical support with the AI system but is not involved in data acquisition and analysis. The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sasaki, M., Tozaki, M., Rodríguez-Ruiz, A. et al. Artificial intelligence for breast cancer detection in mammography: experience of use of the ScreenPoint Medical Transpara system in 310 Japanese women. Breast Cancer 27, 642–651 (2020). https://doi.org/10.1007/s12282-020-01061-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-020-01061-8