Abstract
Purpose
In order to evaluate the diagnostic and therapeutic potential of mammary ductoscopy and watchful follow-up for treating bloody nipple discharge, we investigated the incidence of cancer evolving from the location related to the affected duct and the disappearance of nipple discharge.
Patients and methods
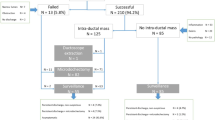
Between April 1998 and March 2008, we assessed 709 lesions among 624 patients without a diagnosis of malignancy at the time of 6 months after mammary ductoscopy. The median follow-up time was 5.5 years. We reviewed the subjects’ charts retrospectively and investigated the dates on which discharge-related cancer was diagnosed and the disappearance of discharge was noted after the initial examination with mammary ductoscopy.
Results
The incidence of cancer evolving from the location related to the pathological duct was 11 % (78/709). Nipple discharge disappeared in 480 (85.1 %) of the 564 followed up lesions, with the exception of 78 breast cancers and 67 resected benign lesions. The rate of disappearance for nipple discharge in the cases of intraductal papilloma at the first examination was 82.5 %. In cases in which no obvious lesions were observed on mammary ductoscopy, there was a 90 % probability that the nipple discharge would disappear, and the rate of evolving breast cancer in the cases of atypical papillary lesions at the first examination was significantly higher than that observed in the cases of intraductal papilloma, at 50 and 8.9 %, respectively.
Conclusions
Information revealed by mammary ductoscopy is useful for differentiating patients who should be subjected to intensive examinations and those who should expect disappearance of their discharge. Mammary ductoscopy and watchful follow-up can substitute microdochectomy in patients with bloody nipple discharge.




Similar content being viewed by others
References
Cabioglu N, Hunt KK, Singletary SE, Stephens TW, Marcy S, Ross MI, et al. Surgical decision making and factors determining a diagnosis of breast carcinoma in women presenting with nipple discharge. J Am Coll Surg. 2003;196(3):354–64.
Dooley WC, Ljung B-M, Veronesi U, Cazzaniga M, Elledge RM, O’Shaughnessy JA, et al. Ductal lavage for detection of cellular atypia in women at high risk for breast cancer. J Natl Cancer Inst. 2001;93(21):1624–32.
Wrensch MR, Petrakis NL, King EB, Miike R, Mason L, Chew KL, et al. Breast cancer incidence in women with abnormal cytology in nipple aspirates of breast fluid. Am J Epidemiol. 1992;135(2):130–41.
Teboul M. A new concept inbreast investigation; echo-histological acino-ductal analytic echography. Biomed Pharmacother. 1988;42:289–96.
Makita M, Sakamoto G, Akiyama F, Namba K, Sugano H, Kasumi F, et al. Duct endoscopy and endoscopic biopsy in the evaluation of nipple discharge. Breast Cancer Res Treat. 1991;18:179–88.
Tang SS, Twelves DJ, Isacke CM, Gui GP. Mammary ductoscopy in the current management of breast disease. Surg Endosc. 2011;25(6):1712–22.
Hunerbein M, Schwarz LE, Schneider U, Schlag PM. Evaluation of pathologic nipple discharge with ductoscopy. J Am Coll Surg. 2003;197:697–8.
Shen RW, Wu J, Lu JS, Han QX, Shen ZZ, Nguyen M, et al. Fiberoptic ductoscopy for patients with nipple discharge. Cancer. 2000;89(7):1512–9.
Dominguez-Cunchillos F, Armendariz P, Perez-Cabanas I, Artieda C, Oteiza F, Sanz MA. Endoscopic technique for the localization of intraduct papillomas. Brit J Surg. 1999;86:1470–1.
Pereira B, Mokbel K. Mammary ductoscopy: past, present, and future. Int J Clin Oncol. 2005;10:112–6.
Al Sarakbi W, Salhab M, Mokbel K. Does mammary ductoscopy have a role in clinical practice? Int Semin Surg Oncol. 2006;3:16.
Dooley WC. Routine operative breast endoscopy during lumpedomy. Ann Surg Oncol. 2003;10:38–42.
Makita M, Namba K, Aoyama E, Mizutani M, Murata H, Yamao R, et al. Endoscopic diagnosis of intraductal lesions in patients with nipple discharge. Jpn J Breast Cancer. 1996;11(1):134–41 (in Japanese with English summary).
Dillon MF, Mohd Nazri SR, Nasir S, Mc Dermott EW, Evoy D, Crotty TB, et al. The role of major duct excision and microdochectomy in the detection of breast carcinoma. BMC Cancer. 2006;6:164. doi:10.1186/1471-2407-6-164.
Kamali S, Bender O, Kamali GH, Aydin MT. Karatepe, and Yuney E:Diagnostic and therapeutic value of ductoscopy in nipple discharge and intraductal proliferations compared with standard methods. Breast Cancer. 2014;21(2):154–61.
Makita M, Akiyama F, Gomi N, Ikenaga M, Yoshimoto M, Kasumi F, et al. Endoscopic classification of intraductal lesions and histological diagnosis. Breast Cancer. 2002;9(3):220–5.
Ashfaq A, Senior D, Pockaj BA, Wasif N, Pizzitola VJ, Giurescu ME, et al. Validation study of a modern treatment algorithm for nipple discharge. Am J Surg. 2014. doi:10.1016/j.amjsurg.2013.12.035.
Matsunaga T, Kawakami Y, Namba K, et al. Intraductal biopsy for diagnosis and treatment of intraductal lesions of the breast. Cancer. 2004;101(10):2164–9.
Nelson RS, Hoehn JL. Twenty-year outcome following central duct resection for bloody nipple discharge. Ann Surg. 2006;243(4):522–4.
Dupont WD, Page DL. Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med. 1985;312(3):146–51.
Haagensen CD (1986) Solitary intraductal papilloma, multiple intraductal papilloma. Disease of the breast, 3rd edn. Philadelphia: W.B. Saunders Co.; 1986. p. 136–191.
Ali-Fehmi R, Carolin K, Wallis T, Visscher DW. Clinicopathologic analysis of breast lesions associated with multiple papillomas. Hum Pathol. 2003;34:234–9.
Makita M, Akiyama F, Gomi N, Iwase T, Kasumi F, Sakamoto G. Endoscopic and histological findings of intraductal lesions presenting with nipple discharge. Breast J. 2006;12(s2):s210–7.
Makita M, Akiyama F, Kimura K, et al. Mammary ductoscopic diagnosis of intraductal spread of breast cancer. Jpn J Breast Cancer. 2001;16(3):274–8 (in Japanese with English summary).
Simpson JS, Connolly EM, Leong WL, Escallon J, McCready D, Reedijk M, et al. Mammary ductoscopy in the evaluation and treatment of pathologic nipple discharge: a Canadian experience. Can J Surg. 2009;52(6):E245–8.
Ballesio L, Maggi C, Savelli S, Angeletti M, De Felice C, Meggiorini ML, et al. Role of breast magnetic resonance imaging (MRI) in patients with unilateral nipple discharge: preliminary study. Radiol Med. 2008;113(2):249–64.
Acknowledgments
This study was supported by a Grant from Foundation for Promotion of Cancer Research.
Conflict of interest
No authors have any conflict of interest to declare in association with this study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Makita, M., Akiyama, F., Gomi, N. et al. Mammary ductoscopy and watchful follow-up substitute microdochectomy in patients with bloody nipple discharge. Breast Cancer 23, 242–251 (2016). https://doi.org/10.1007/s12282-014-0561-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-014-0561-z