Abstract
Background
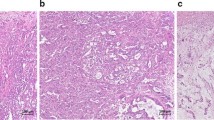
Even after needle biopsy, the preoperative differential diagnoses of intracystic tumors of the breast are challenging because of their nonspecific radiological characteristics and subtle cytological and histological appearance. The aim of this study is to investigate a novel diagnostic method, targeting genomic instability (GIN) in intracystic tumors of the breast, using tumor DNA from samples obtained by fine-needle aspiration biopsy (FNAB).
Methods
Thirteen consecutive intracystic tumors of the breast, including five cancers and eight benign tumors, were studied. Three FNAB passages per tumor were used for array comparative genomic hybridization (aCGH) analysis to quantify GIN in each tumor. Tumor DNA from the main tumor, taken from formalin-fixed, paraffin-embedded (FFPE) blocks corresponding to FNAB samples, was also analyzed to compare cytogenetic profiles between these sample types.
Results
After three FNAB passages, an average of 7.09 μg (0.24–25.0 μg) of DNA was obtained. The quality of the DNA and the aCGH data was excellent, as judged by the mean derivative log ratio spread (DLRSpread) of 0.22 (0.15–0.29). The cytogenetic profiles of paired FNAB and main tumor FFPE samples were highly similar, with an average concordance rate of 97.7 % (81.2–100 %). aCGH analysis from FNAB samples showed significantly more GIN in cancers than in benign tumors, with mean frequencies of aberrant chromosomal regions of 17.5 and 0.34 %, respectively (Wilcoxon’s rank sum test, P = 0.0016).
Conclusions
Our novel diagnostic method, which targets GIN, can clearly distinguish cancers from benign tumors of breast intracystic lesions with minimal invasion, thereby avoiding the need for surgical excisional biopsy.



Similar content being viewed by others
References
Carter D, Orr SL, Merino MJ. Intracystic papillary carcinoma of the breast. After mastectomy, radiotherapy or excisional biopsy alone. Cancer. 1983;52(1):14–9.
Solorzano CC, Middleton LP, Hunt KK, Mirza N, Meric F, Kuerer HM, Ross MI, Ames FC, Feig BW, Pollock RE, et al. Treatment and outcome of patients with intracystic papillary carcinoma of the breast. Am J Surg. 2002;184(4):364–8.
Mulligan AM, O’Malley FP. Metastatic potential of encapsulated (intracystic) papillary carcinoma of the breast: a report of 2 cases with axillary lymph node micrometastases. Int J Surg Pathol. 2007;15(2):143–7.
Fayanju OM, Ritter J, Gillanders WE, Eberlein TJ, Dietz JR, Aft R, Margenthaler JA. Therapeutic management of intracystic papillary carcinoma of the breast: the roles of radiation and endocrine therapy. Am J Surg. 2007;194(4):497–500.
Grabowski J, Salzstein SL, Sadler GR, Blair S. Intracystic papillary carcinoma: a review of 917 cases. Cancer. 2008;113(5):916–20.
Rizzo M, Lund MJ, Oprea G, Schniederjan M, Wood WC, Mosunjac M. Surgical follow-up and clinical presentation of 142 breast papillary lesions diagnosed by ultrasound-guided core-needle biopsy. Ann Surg Oncol. 2008;15(4):1040–7.
Sakr R, Rouzier R, Salem C, Antoine M, Chopier J, Darai E, Uzan S. Risk of breast cancer associated with papilloma. Eur J Surg Oncol. 2008;34(12):1304–8.
Douglas-Jones AG, Verghese A. Diagnostic difficulty arising from displaced epithelium after core biopsy in intracystic papillary lesions of the breast. J Clin Pathol. 2002;55(10):780–3.
Okita R, Ohsumi S, Takashima S, Saeki T, Aogi K, Nishimura R. Synchronous liver metastases of intracystic papillary carcinoma with invasion of the breast. Breast Cancer. 2005;12(4):327–30.
Jagmohan P, Pool FJ, Putti TC, Wong J. Papillary lesions of the breast: imaging findings and diagnostic challenges. Diagn Interv Radiol. 2013;19(6):471–8.
Saddik M, Lai R, Medeiros LJ, McCourty A, Brynes RK. Differential expression of cyclin D1 in breast papillary carcinomas and benign papillomas: an immunohistochemical study. Arch Pathol Lab Med. 1999;123(2):152–6.
Hill CB, Yeh IT. Myoepithelial cell staining patterns of papillary breast lesions: from intraductal papillomas to invasive papillary carcinomas. Am J Clin Pathol. 2005;123(1):36–44.
Zhang C, Zhang P, Hao J, Quddus MR, Steinhoff MM, Sung CJ. High nuclear grade, frequent mitotic activity, cyclin D1 and p53 overexpression are associated with stromal invasion in mammary intracystic papillary carcinoma. Breast J. 2005;11(1):2–8.
Shamonki J, Chung A, Huynh KT, Sim MS, Kinnaird M, Giuliano A. Management of papillary lesions of the breast: can larger core needle biopsy samples identify patients who may avoid surgical excision? Ann Surg Oncol. 2013;20(13):4137–44.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Tsuda H, Takarabe T, Susumu N, Inazawa J, Okada S, Hirohashi S. Detection of numerical and structural alterations and fusion of chromosomes 16 and 1 in low-grade papillary breast carcinoma by fluorescence in situ hybridization. Am J Pathol. 1997;151(4):1027–34.
Lininger RA, Park WS, Man YG, Pham T, MacGrogan G, Zhuang Z, Tavassoli FA. LOH at 16p13 is a novel chromosomal alteration detected in benign and malignant microdissected papillary neoplasms of the breast. Hum Pathol. 1998;29(10):1113–8.
Di Cristofano C, Mrad K, Zavaglia K, Bertacca G, Aretini P, Cipollini G, Bevilacqua G, Ben Romdhane K, Cavazzana A. Papillary lesions of the breast: a molecular progression? Breast Cancer Res Treat. 2005;90(1):71–6.
Yoshida M, Mouri Y, Yamamoto S, Yorozuya K, Fujii K, Nakano S, Fukutomi T, Hara K, Tsuda H. Intracystic invasive papillary carcinoma of the male breast with analyses of loss of heterozygosity on chromosome 16q. Breast Cancer 2009;17(2):146–50.
Duprez R, Wilkerson PM, Lacroix-Triki M, Lambros MB, Mackay A, Hern RA, Gauthier A, Pawar V, Colombo PE, Daley F, et al. Immunophenotypic and genomic characterization of papillary carcinomas of the breast. J Pathol. 2012;226(3):427–41.
Oikawa M, Nagayasu T, Yano H, Hayashi T, Abe K, Kinoshita A, Yoshiura K. Intracystic papillary carcinoma of breast harbors significant genomic alteration compared with intracystic papilloma: genome-wide copy number and LOH analysis using high-density single-nucleotide polymorphism microarrays. Breast J. 2011;17(4):427–30.
Oikawa M, Yoshiura K, Kondo H, Miura S, Nagayasu T, Nakashima M. Significance of genomic instability in breast cancer in atomic bomb survivors: analysis of microarray-comparative genomic hybridization. Radiat Oncol. 2011;6:168.
Arai J, Tsuchiya T, Oikawa M, Mochinaga K, Hayashi T, Yoshiura K, Tsukamoto K, Yamasaki N, Matsumoto K, Miyazaki T, et al. Clinical and molecular analysis of synchronous double lung cancers. Lung Cancer. 2012;77(2):281–7.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Nakao K, Oikawa M, Arai J, Mussazhanova Z, Kondo H, Shichijo K, Nakashima M, Hayashi T, Yoshiura K, Hatachi T, et al. A predictive factor of the quality of microarray comparative genomic hybridization analysis for formalin-fixed paraffin-embedded archival tissue. Diagn Mol Pathol. 2013;22(3):174–80.
Symmans WF, Ayers M, Clark EA, Stec J, Hess KR, Sneige N, Buchholz TA, Krishnamurthy S, Ibrahim NK, Buzdar AU, et al. Total RNA yield and microarray gene expression profiles from fine-needle aspiration biopsy and core-needle biopsy samples of breast carcinoma. Cancer. 2003;97(12):2960–71.
Acknowledgments
This study was supported by Grant-in-Aid for Young Scientists (B) #24791382 of Japan Society for the Promotion of Science KAKENHI (2012–2013).
Conflict of interest
No financial or other potential conflicts of interest exist for any of the authors.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Oikawa, M., Yano, H., Matsumoto, M. et al. A novel diagnostic method targeting genomic instability in intracystic tumors of the breast. Breast Cancer 22, 529–535 (2015). https://doi.org/10.1007/s12282-013-0516-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-013-0516-9