Abstract
Purpose of Review
Cystic fibrosis (CF) is an inherited disease that can progressively affect multiple organs including respiratory tract. CF has been believed to occur infrequently in the Middle East (ME). However, it seems that CF maybe more common in ME countries than expected before. Despite the fact that surveillance of fungal infections is essential, data in the ME region remain scarce. This narrative review aims to evaluate the previously published data on the prevalence of fungal respiratory colonization and infections, spectrum of isolated fungi from the respiratory tract, and antifungal treatment in CF patients across ME countries.
Recent Findings
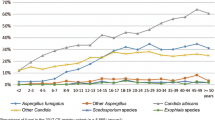
Among different opportunistic fungal pathogens, Aspergillus fumigatus and Candida species were reported as the most prevalent mold and yeast like fungi isolated from respiratory tract of CF patients from ME countries. A. fumigatus was reported as the common filamentous colonizing fungi of the respiratory tract of CF patients from Turkey in the range 10.4–76.3%. Colonization due to Aspergillus also showed the highest frequency for A. fumigatus (50.0%) in CF patients from Qatar. However, in a more comprehensive study from Iran, A. flavus was the most common. Scedosporium spp. has not been reported in CF patients from ME countries except for one study in Iran.
Summary
Future efforts should focus on improving laboratory capacities in ME for detection of common and rare fungal pathogens. National CF registries could help to collect more systematic data on fungal colonization and infection in patients in the ME.

Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Mirtajani SB, Farnia P, Hassanzad M, Ghanavi J, Farnia P, Velayati AA. Geographical distribution of cystic fibrosis; the past 70 years of data analyzis. Biomed Biotechnol Res J. 2017;1(2):105–12. https://doi.org/10.4103/bbrj.bbrj_81_17.
Lopes-Pacheco M. CFTR modulators: the changing face of cystic fibrosis in the era of precision medicine. Front Pharmacol. 2020;10:1662. https://doi.org/10.3389/fphar.2019.01662.
Chillón M, Casals T, Mercier B, Bassas L, Lissens W, Silber S, et al. Mutations in the cystic fibrosis gene in patients with congenital absence of the vas deferens. N Engl J Med. 1995;332(22):1475–80. https://doi.org/10.1056/NEJM199506013322204.
Page A, Goldenberg A, Matthews AL. Lived experiences of individuals with cystic fibrosis on CFTR-modulators. BMC Pulm Med. 2022;22(1):1–12. https://doi.org/10.1186/s12890-022-01825-2.
De Boeck K, Zolin A, Cuppens H, Olesen H, Viviani L. The relative frequency of CFTR mutation classes in European patients with cystic fibrosis. J Cyst Fibros. 2014;13(4):403–9. https://doi.org/10.1016/j.jcf.2013.12.003.
Bonyadi M, Omrani O, Rafeey M, Bilan N. Spectrum of CFTR gene mutations in Iranian Azeri Turkish patients with cystic fibrosis. Genet Test Mol Biomarkers. 2011;15(1–2):89–92. https://doi.org/10.1089/gtmb.2010.0091.
Zamani RAM. Mutation analysis of CFTR gene in 70 Iranian cystic fibrosis patients. Iran J Allergy Asthma Immunol. 2006:3–8
Bobadilla JL, Macek M Jr, Fine JP, Farrell PM. Cystic fibrosis: a worldwide analysis of CFTR mutations—correlation with incidence data and application to screening. Hum Mutat. 2002;19(6):575–606. https://doi.org/10.1002/humu.10041.
Oskooei VK, Dooki MRE, Tabaripour R, Mirzajani S, Pourbagher R, Akhavan-Niaki H. CFTR haplotypes in northern Iranian population. Gene. 2013;512(1):55–60. https://doi.org/10.1016/j.gene.2012.09.096.
Hosseini Nami A, Kabiri M, Zafarghandi Motlagh F, Shirzadeh T, Fakhari N, Karimi A, et al. Genetic attributes of Iranian cystic fibrosis patients: the diagnostic efficiency of CFTR mutations in over a decade. Front Genet. 2023;14:1140034. https://doi.org/10.3389/fgene.2023.1140034.
Thomas M, Aboukhalaf S, Darwish T, Ali M, Elsaied O, Al Bakri M, et al. The spectrum of fungal colonization and their attributable effects on cystic fibrosis patients with rare CFTR genetic mutations. Microbiol Res. 2021;12(3):591–605. https://doi.org/10.3390/microbiolres12030042.
Farrell PM. The prevalence of cystic fibrosis in the European Union. J Cyst Fibros. 2008;7(5):450–3. https://doi.org/10.1016/j.jcf.2008.03.007.
Silva Filho LVRF, Castaños C, Ruíz HH. Cystic fibrosis in Latin America—improving the awareness. J Cyst Fibros. 2016;15(6):791–3. https://doi.org/10.1016/j.jcf.2016.05.007.
Scotet V, Gutierrez H, Farrell PM. Newborn screening for CF across the globe—where is it worthwhile? Int J Neonatal Screen. 2020;6(1):18. https://doi.org/10.3390/ijns6010018.
Shteinberg M, Haq IJ, Polineni D, Davies JC. Cystic fibrosis. Lancet. 2021;397(10290):2195–211. https://doi.org/10.1016/s0140-6736(20)32542-3.
Bell SC, Mall MA, Gutierrez H, Macek M, Madge S, Davies JC, et al. The future of cystic fibrosis care: a global perspective. Lancet Respir Med. 2020;8(1):65–124. https://doi.org/10.1016/s2213-2600(19)30337-6.
Guo J, Garratt A, Hill A. Worldwide rates of diagnosis and effective treatment for cystic fibrosis. J Cyst Fibros. 2022;21(3):456–62. https://doi.org/10.1016/j.jcf.2022.01.009.
da Silva LVRF, Zampoli M, Cohen-Cymberknoh M, Kabra SK. Cystic fibrosis in low and middle-income countries (LMIC): a view from four different regions of the world. Paediatr Respir Rev. 2021;38:37–44. https://doi.org/10.1016/j.prrv.2020.07.004.
Aghamohammadi A, Keivanfar M, Navaei S, Shirzadi R, Masiha F, Allameh Z, et al. First cystic fibrosis patient registry annual data report-cystic fibrosis foundation of Iran. Acta Med Iran. 2019:33–41.https://doi.org/10.18502/acta.v57i1.1751.
Dogru D, Çakır E, Şişmanlar T, Çobanoğlu N, Pekcan S, Cinel G, et al. Cystic fibrosis in Turkey: First data from the national registry. Pediatr Pulmonol. 2020;55(2):541–8. https://doi.org/10.1002/ppul.24561.
Stafler P, Mei-Zahav M, Wilschanski M, Mussaffi H, Efrati O, Lavie M, et al. The impact of a national population carrier screening program on cystic fibrosis birth rate and age at diagnosis: Implications for newborn screening. J Cyst Fibros. 2016;15(4):460–6. https://doi.org/10.1016/j.jcf.2015.08.007.
Cuppens H, Boulyjenkov V, Cassiman J, Cutting G, Dodge J, Des Georges M, et al. The molecular genetic epidemiology of cystic fibrosis: report of a joint meeting of WHO/ECFTN/ICF (M) A/ECFS. 2004
Desgeorges M, Mégarbané A, Guittard C, Carles S, Loiselet J, Demaille J, Claustres M. Cystic fibrosis in Lebanon: distribution of CFTR mutations among Arab communities. Hum Genet. 1997;100:279–83. https://doi.org/10.1007/s004390050505.
Al-Mahroos F. Cystic fibrosis in Bahrain incidence, phenotype, and outcome. J Trop Pediatr. 1998;44(1):35–9. https://doi.org/10.1093/tropej/44.1.35.
Havasian MR, Panahi J, Mahdieh N. Cystic fibrosis and distribution and mutation analysis of CFTR gene in Iranian patients. Faslnamahi Kumish. 2014;15(4):431–40.
https://worldpopulationreview.com/country-rankings/middle-east-countries. Accessed November 1, 2023.
Quittner AL, Schechter MS, Rasouliyan L, Haselkorn T, Pasta DJ, Wagener JS. Impact of socioeconomic status, race, and ethnicity on quality of life in patients with cystic fibrosis in the United States. Chest. 2010;137(3):642–50.
Palla JB. Disparities and therapeutic advances in cystic fibrosis. Pediatr Pulmonol. 2023. https://doi.org/10.1002/ppul.26445.
Delhaes L, Monchy S, Fréalle E, Hubans C, Salleron J, Leroy S, et al. The airway microbiota in cystic fibrosis: a complex fungal and bacterial community—implications for therapeutic management. PLoS ONE. 2012;7(4):e36313. https://doi.org/10.1371/journal.pone.0036313.
Emerson J, Rosenfeld M, McNamara S, Ramsey B, Gibson RL. Pseudomonas aeruginosa and other predictors of mortality and morbidity in young children with cystic fibrosis. Pediatr Pulmonol. 2002;34(2):91–100. https://doi.org/10.1002/ppul.10127.
Sagel SD, Gibson RL, Emerson J, McNamara S, Burns JL, Wagener JS, et al. Impact of Pseudomonas and Staphylococcus infection on inflammation and clinical status in young children with cystic fibrosis. J Pediatr. 2009;154(2):183–8. https://doi.org/10.1016/j.jpeds.2008.08.001.
Salsgiver EL, Fink AK, Knapp EA, LiPuma JJ, Olivier KN, Marshall BC, Saiman L. Changing epidemiology of the respiratory bacteriology of patients with cystic fibrosis. Chest. 2016;149(2):390–400. https://doi.org/10.1378/chest.15-0676.
Tracy MC, Moss RB. The myriad challenges of respiratory fungal infection in cystic fibrosis. Pediatr Pulmonol. 2018;53(S3):S75–85. https://doi.org/10.1002/ppul.24126.
Sudfeld CR, Dasenbrook EC, Merz WG, Carroll KC, Boyle MP. Prevalence and risk factors for recovery of filamentous fungi in individuals with cystic fibrosis. J Cyst Fibros. 2010;9(2):110–6. https://doi.org/10.1016/j.jcf.2009.11.010.
Yan K, Yin H, Wang J, Cai Y. Subtle relationships between Pseudomonas aeruginosa and fungi in patients with cystic fibrosis. Acta Clin Belg. 2022;77(2):425–35. https://doi.org/10.1080/17843286.2020.1852850.
Chotirmall SH, McElvaney NG. Fungi in the cystic fibrosis lung: bystanders or pathogens? J Biochem Cell Biol. 2014;52:161–73. https://doi.org/10.1016/j.biocel.2014.03.001.
Touati K, Nguyen DNL, Delhaes L. The airway colonization by opportunistic filamentous fungi in patients with cystic fibrosis: recent updates. Curr Fungal Infect Rep. 2014;8:302–11. https://doi.org/10.1007/s12281-014-0197-7.
Gileles-Hillel A, Shoseyov D, Polacheck I, Korem M, Kerem E, Cohen-Cymberknoh M. Association of chronic Candida albicans respiratory infection with a more severe lung disease in patients with cystic fibrosis. Pediatr Pulmonol. 2015;50(11):1082–9. https://doi.org/10.1002/ppul.23302.
De Jong C, Slabbers L, Engel T, Yntema J, van Westreenen M, Croughs P, et al. Clinical relevance of Scedosporium spp. and Exophiala dermatitidis in patients with cystic fibrosis: A nationwide study. Med Mycol. 2020;58(7):859–66. https://doi.org/10.1093/mmy/myaa003.
Abdolrasouli A, Bercusson AC, Rhodes JL, Hagen F, Buil JB, Tang AY, et al. Airway persistence by the emerging multi-azole-resistant Rasamsonia argillacea complex in cystic fibrosis. Mycoses. 2018;61(9):665–73. https://doi.org/10.1111/myc.12789.
Hoenigl M, Salmanton-García J, Walsh TJ, Nucci M, Neoh CF, Jenks JD, et al. Global guideline for the diagnosis and management of rare mould infections: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiology. Lancet Infect Dis. 2021. https://doi.org/10.1016/s1473-3099(20)30784-2.
Sedlacek L, Graf B, Schwarz C, Albert F, Peter S, Würstl B, et al. Prevalence of Scedosporium species and Lomentospora prolificans in patients with cystic fibrosis in a multicenter trial by use of a selective medium. J Cyst Fibros. 2015;14(2):237–41. https://doi.org/10.1016/j.jcf.2014.12.014.
Seufert R, Sedlacek L, Kahl B, Hogardt M, Hamprecht A, Haase G, et al. Prevalence and characterization of azole-resistant Aspergillus fumigatus in patients with cystic fibrosis: a prospective multicentre study in Germany. J Antimicrob Chemother. 2018;73(8):2047–53. https://doi.org/10.1093/jac/dky147.
Stathi A, Loukou I, Kirikou H, Petrocheilou A, Moustaki M, Velegraki A, Zachariadou L. Isolation of Candida auris from cystic fibrosis patient, Greece, April 2019. Euro Surveill. 2019;24(29):1900400. https://doi.org/10.2807/1560-7917.ES.2019.24.29.1900400.
Jenks JD, Seidel D, Cornely OA, Chen S, van Hal S, Kauffman C, et al. Voriconazole plus terbinafine combination antifungal therapy for invasive Lomentospora prolificans infections: analysis of 41 patients from the FungiScope® registry 2008–2019. Clin Microbiol Infect. 2020:S1198–743X(20)30037–9.https://doi.org/10.1016/j.cmi.2020.01.012.
Boyer J, Feys S, Zsifkovits I, Hoenigl M, Egger M. Treatment of invasive Aspergillosis: how it’s going, where it’s heading. Mycopathologia. 2023. https://doi.org/10.1007/s11046-023-00727-z.
Janahi IA, Rehman A, Al-Naimi AR. Allergic bronchopulmonary aspergillosis in patients with cystic fibrosis. Ann Thorac Med. 2017;12(2):74. https://doi.org/10.4103/atm.ATM_231_16.
Amin R, Dupuis A, Aaron SD, Ratjen F. The effect of chronic infection with Aspergillus fumigatus on lung function and hospitalization in patients with cystic fibrosis. Chest. 2010;137(1):171–6. https://doi.org/10.1378/chest.09-1103.
Baxter CG, Dunn G, Jones AM, Webb K, Gore R, Richardson MD, Denning DW. Novel immunologic classification of aspergillosis in adult cystic fibrosis. J Allergy Clin Immunol. 2013;132(3):560–6. https://doi.org/10.1016/j.jaci.2013.04.007.
King J, Brunel SF, Warris A. Aspergillus infections in cystic fibrosis. J Infect. 2016;72:S50–5.
Antunes J, Fernandes A, Borrego LM, Leiria-Pinto P, Cavaco J. Cystic fibrosis, atopy, asthma and ABPA. Allergol Immunopathol (Madr). 2010;38(5):278–84. https://doi.org/10.1016/j.aller.2010.06.002.
Henry M, Bennett D, Kiely J, Kelleher N, Bredin C. Fungal atopy in adult cystic fibrosis. Respir Med. 2000;94(11):1092–6. https://doi.org/10.1053/rmed.2000.0918.
Tobin M, Maguire O, Reen D, Tempany E, Fitzgerald M. Atopy and bronchial reactivity in older patients with cystic fibrosis. Thorax. 1980;35(11):807–13. https://doi.org/10.1136/thx.35.11.807.
Poore TS, Meier M, Towler E, Martiniano SL, Brinton JT, DeBoer EM, et al. Clinical characteristics of people with cystic fibrosis and frequent fungal infection. Pediatr Pulmonol. 2022;57(1):152–61. https://doi.org/10.1002/ppul.25741.
Poore TS, Hong G, Zemanick ET. Fungal infection and inflammation in cystic fibrosis. Pathogens. 2021;10(5):618. https://doi.org/10.3390/pathogens10050618.
Hassanzad M, Mortezaee V, Bongomin F, Poorabdollah M, Sharifynia S, Maleki M, et al. Successful control of exacerbation of allergic bronchopulmonary aspergillosis due to Aspergillus terreus in a cystic fibrosis patient with short-term adjunctive therapy with voriconazole: a case report. J Mycol Med. 2019;29(2):189–92. https://doi.org/10.1016/j.mycmed.2019.02.001.
Maleki M, Mortezaee V, Hassanzad M, Mahdaviani S, Poorabdollah M, Mehrian P, et al. Prevalence of allergic bronchopulmonary aspergillosis in cystic fibrosis patients using two different diagnostic criteria. Eur Ann Allergy Clin Immunol. 2020;52(3):104–11. https://doi.org/10.23822/eurannaci.1764-1489.121.
Alyasin S, Moghtaderi M, Farjadian S, Babaei M, Teshnizi SH. Allergic bronchopulmonary aspergillosis in patients with cystic fibrosis and non-cystic fibrosis bronchiectasis. Electron Physician. 2018;10(1):6273. https://doi.org/10.19082/6273.
Khalilzadeh S, Hassanzad M, Toutkaboni MP, Nejad ST, Sheikholeslami F-M, Velayati AA. Reappraisal of frequency of common cystic fibrosis transmembrane conductance regulator gene mutations in Iranian cystic fibrosis patients. Tanaffos. 2018;17(2):73.
Yakut N, Kadayifci EK, Eralp EE, Gokdemir Y. Successful treatment of allergic bronchopulmonary aspergillosis with posaconazole in a child with cystic fibrosis: case report and review of the literature. Lung India. 2020;37(2):161. https://doi.org/10.4103/lungindia.lungindia_288_19.
Cakir E, Uyan Z, Ersu RH, Karadag B, Karakoc F, Dagli E. Mucoid impaction: an unusual form of allergic bronchopulmonary aspergillosis in a patient with cystic fibrosis. Pediatr Pulmonol. 2006;41(11):1103–7. https://doi.org/10.1002/ppul.20499.
Emiralioglu N, Dogru D, Tugcu GD, Yalcin E, Kiper N, Ozcelik U. Omalizumab treatment for allergic bronchopulmonary aspergillosis in cystic fibrosis. Ann Pharmacother. 2016;50(3):188–93. https://doi.org/10.1177/1060028015624204.
Nasri E, Fakhim H, Vaezi A, Khalilzadeh S, Ahangarkani F, Laal Kargar M, et al. Airway colonisation by Candida and Aspergillus species in Iranian cystic fibrosis patients. Mycoses. 2019;62(5):434–40. https://doi.org/10.1111/myc.12898.
Kartal G. Asthma-like symptom or “cystic fibrosis asthma”? Tuberk Toraks. 2021;69(2):167–76. https://doi.org/10.5578/tt.20219806.
Emiralioğlu N, Dogru D, Dogan Ö, Gulmez D, Akdagli S, Polat S, et al. Diverse clinical characteristics of Aspergillus growth in patients with cystic fibrosis. Turk J Pediatr. 2020;62(4).https://doi.org/10.24953/turkjped.2020.04.005.
Hamad SG, Abu-Hasan M, AbdulWahab A. Use of intravenous pulse steroids to treat allergic bronchopulmonary aspergillosis in a non-compliant asthmatic adolescent. Children. 2022;9(2):252. https://doi.org/10.3390/children9020252.
Hedayati MT, Tavakoli M, Maleki M, Heidari S, Mortezaee V, Gheisari M, et al. Fungal epidemiology in cystic fibrosis patients with a special focus on Scedosporium species complex. Microb Pathog. 2019;129:168–75. https://doi.org/10.1016/j.micpath.2019.02.009.
Atay Ö, Asilsoy S, Köse S, Atakul G, Al S, Boyacioğlu ÖK, et al. The importance of aeroallergen sensitivity in children with cystic fibrosis. Allergol Immunopathol (Madr). 2022;50(3):1–9. https://doi.org/10.15586/aei.v50iSP3.764.
AbdulWahab A, Salah H, Chandra P, Taj-Aldeen SJ. Persistence of Candida dubliniensis and lung function in patients with cystic fibrosis. BMC Res Notes. 2017;10(1):1–5. https://doi.org/10.1186/s13104-017-2656-z.
Irmak I, Damadoğlu E, Güven DK, Huseynova X, İnkaya AÇ, Er B, et al. Clinical implications of fungal isolation from sputum in adult patients with cystic fibrosis. Turk J Med Sci. 2021;51(3):1191–200. https://doi.org/10.3906/sag-2006-94.
Asef A, Ghafaripour HA, Jamaati H, Varahram M, Adcock IM, Mortaz E. The role of HLA-DRB1 alleles in pulmonary cystic fibrosis. Iran J Allergy Asthma Immunol. 2022:1–8.https://doi.org/10.18502/ijaai.v21i2.9226.
Magee LC, Louis M, Khan V, Micalo L, Chaudary N. Managing fungal infections in cystic fibrosis patients: challenges in clinical practice. Infect Drug Resist. 2021:1141–53.https://doi.org/10.2147/IDR.S267219.
Schwarz C, Bouchara J-P, Buzina W, Chrenkova V, Dmeńska H, de La Pedrosa EGG, et al. Organization of patient management and fungal epidemiology in cystic fibrosis. Mycopathologia. 2018;183:7–19. https://doi.org/10.1007/s11046-017-0205-x.
Ghazanfari M, Arastehfar A, Davoodi L, Yazdani Charati J, Moazeni M, Abastabar M, et al. Pervasive but neglected: a perspective on COVID-19-associated pulmonary mold infections among mechanically ventilated COVID-19 patients. Front Med (Lausanne). 2021;8:649675. https://doi.org/10.3389/fmed.2021.649675.
Hassanzad M, Boloursaz MR, Darougar S, Nejad ST, Mohajerani SA, Baghaie N, et al. Long term outcome of cystic fibrosis patients with multisystem evaluation. Adv Respir Med. 2016;84(6):310–5. https://doi.org/10.5603/ARM.2016.0040.
Güngör Ö, Tamay Z, Güler N, Erturan Z. Frequency of fungi in respiratory samples from Turkish cystic fibrosis patients. Mycoses. 2013;56(2):123–9. https://doi.org/10.1111/j.1439-0507.2012.02221.x.
Taj-Aldeen S, El Shafie S, Alsoub H, Eldeeb Y, De Hoog G. Isolation of Exophiala dermatitidis from endotracheal aspirate of a cancer patient. Mycoses. 2006;49(6):504–9. https://doi.org/10.1111/j.1439-0507.2006.01280.x.
Koch C, Høiby N. Diagnosis and treatment of cystic fibrosis. Respiration. 2000;67(3):239–47. https://doi.org/10.1159/000029503.
Aidoo E, Alexander S,Alshafi K, Al-Yaghchi C, Anderson AK, Balfour-Lynn I, et al. Clinical guidelines: care of children with cystic fibrosis. 2023. Available on www.rbht.nhs.uk/childrencf.
Aaron SD, Vandemheen KL, Freitag A, Pedder L, Cameron W, Lavoie A, et al. Treatment of Aspergillus fumigatus in patients with cystic fibrosis: a randomized, placebo-controlled pilot study. PLoS ONE. 2012;7(4):e36077. https://doi.org/10.1371/journal.pone.0036077.
Coughlan CA, Chotirmall SH, Renwick J, Hassan T, Low TB, Bergsson G, et al. The effect of Aspergillus fumigatus infection on vitamin D receptor expression in cystic fibrosis. Am J Respir Crit Care Med. 2012;186(10):999–1007. https://doi.org/10.1164/rccm.201203-0478OC.
Blomquist A, Inghammar M, Al Shakirchi M, Ericson P, Krantz C, Svedberg M, et al. Persistent Aspergillus fumigatus infection in cystic fibrosis: impact on lung function and role of treatment of asymptomatic colonization-a registry-based case-control study. BMC Pulm Med. 2022;22(1):263. https://doi.org/10.1186/s12890-022-02054-3.
Soleimani Z, Teymouri P, Boloorani AD, Mesdaghinia A, Middleton N, Griffin DW. An overview of bioaerosol load and health impacts associated with dust storms: a focus on the Middle East. Atmos Environ. 2020;223:117187. https://doi.org/10.1016/j.atmosenv.2019.117187.
Nnadi NE, Carter DA. Climate change and the emergence of fungal pathogens. PLoS Pathog. 2021;17(4):e1009503. https://doi.org/10.1371/journal.ppat.1009503.
Gadre A, Enbiale W, Andersen LK, Coates SJ. The effects of climate change on fungal diseases with cutaneous manifestations: a report from the International Society of Dermatology Climate Change Committee. J Clim Chang Health. 2022:100156. https://doi.org/10.1016/j.joclim.2022.100156.
Chang YC, Tsai H-F, Karos M, Kwon-Chung K. THTA, a thermotolerance gene of Aspergillus fumigatus. Fungal Genet Biol. 2004;41(9):888–96. https://doi.org/10.1016/j.fgb.2004.06.004.
Kwon-Chung KJ, Sugui JA. Aspergillus fumigatus—what makes the species a ubiquitous human fungal pathogen? PLoS Pathog. 2013;9(12):e1003743. https://doi.org/10.1371/journal.ppat.1003743.
van Rhijn N, Bromley M. The consequences of our changing environment on life threatening and debilitating fungal diseases in humans. J Fungi (Basel). 2021;7(5):367. https://doi.org/10.3390/jof7050367.
Krishnan S, Manavathu EK, Chandrasekar PH. Aspergillus flavus: an emerging non-fumigatus Aspergillus species of significance. Mycoses. 2009;52(3):206–22. https://doi.org/10.1111/j.1439-0507.2008.01642.x.
Erami M, Hashemi SJ, Raiesi O, Fattahi M, Getso MI, Momen-Heravi M, et al. COVID-19-associated pulmonary aspergillosis (CAPA) in Iranian patients admitted with severe COVID-19 pneumonia. Infection. 2023;51(1):223–30. https://doi.org/10.1007/s15010-022-01907-7.
Lang-Yona N, Shuster-Meiseles T, Mazar Y, Yarden O, Rudich Y. Impact of urban air pollution on the allergenicity of Aspergillus fumigatus conidia: outdoor exposure study supported by laboratory experiments. Sci Total Environ. 2016;541:365–71. https://doi.org/10.1016/j.scitotenv.2015.09.058.
Lee P-H, Park S, Lee Y-G, Choi S-M, An M-H, Jang A-S. The impact of environmental pollutants on barrier dysfunction in respiratory disease. Allergy Asthma Immunol Res. 2021;13(6):850. https://doi.org/10.4168/aair.2021.13.6.850.
Bertuzzi M, Hayes GE, Icheoku UJ, Van Rhijn N, Denning DW, Osherov N, Bignell EM. Anti-Aspergillus activities of the respiratory epithelium in health and disease. J Fungi (Basel). 2018;4(1):8. https://doi.org/10.3390/jof4010008.
Ramsay K, Stockwell R, Bell S, Kidd T. Infection in cystic fibrosis: impact of the environment and climate. Expert Rev Respir Med. 2016;10(5):505–19. https://doi.org/10.1586/17476348.2016.1162715.
Lanz B, Dietz S, Swanson T. The expansion of modern agriculture and global biodiversity decline: an integrated assessment. Ecol Econ. 2018;144:260–77. https://doi.org/10.1016/j.ecolecon.2017.07.018.
Alkhalifah DHM, Damra E, Melhem MB, Hozzein WN. Fungus under a changing climate: modeling the current and future global distribution of Fusarium oxysporum using geographical information system data. Microorganisms. 2023;11(2):468. https://doi.org/10.3390/microorganisms11020468.
Garrett KA, Nita M, De Wolf E, Esker PD, Gomez-Montano L, Sparks AH. Plant pathogens as indicators of climate change. Climate change: Elsevier; 2021. 499–513.https://doi.org/10.1016/B978-0-12-821575-3.00024-4.
Snelders E, Huis in’t Veld RA, Rijs AJ, Kema GH, Melchers WJ, Verweij PE. Possible environmental origin of resistance of Aspergillus fumigatus to medical triazoles. Appl Environ Microbiol. 2009;75(12):4053–7. https://doi.org/10.1128/AEM.00231-09.
Namdar R, Karami E, Keshavarz M. Climate change and vulnerability: the case of MENA countries. Int J Geo-Inf. 2021;10(11):794. https://doi.org/10.3390/ijgi10110794.
King JA, Nichols A-L, Bentley S, Carr SB, Davies JC. An update on CFTR modulators as new therapies for cystic fibrosis. Paediatr Drugs. 2022;24(4):321–33. https://doi.org/10.1007/s40272-022-00509-y.
Salah H, Lackner M, Houbraken J, Theelen B, Lass-Flörl C, Boekhout T, et al. The emergence of rare clinical Aspergillus species in Qatar: molecular characterization and antifungal susceptibility profiles. Front Microbiol. 2019;10:1677. https://doi.org/10.3389/fmicb.2019.01677.
Güngör Ö, Sampaio-Maia B, Amorim A, Araujo R, Erturan Z. Determination of azole resistance and TR 34/L98H mutations in isolates of Aspergillus section Fumigati from Turkish cystic fibrosis patients. Mycopathologia. 2018;183:913–20. https://doi.org/10.1007/s11046-018-0297-y.
Karaman M, Firinci F, Karaman O, Uzuner N, Hakki Bahar I. Long-term oropharyngeal colonization by C. albicans in children with cystic fibrosis. Yeast. 2013;30(11):429–36. https://doi.org/10.1002/yea.2977.
Wahab AA, Janahi I, Marafia M, El-Shafie S. Microbiological identification in cystic fibrosis patients with CFTR I1234V mutation. J Trop Pediatr. 2004;50(4):229–33. https://doi.org/10.1093/tropej/50.4.229.
Al Arrayed SS, Abdulla F. Incidence of cystic fibrosis in Bahrain. J Bahrain Med Soc. 1996;8:157–60.
Author information
Authors and Affiliations
Contributions
M.T.H., M.G., B.N.S., S.A.S., S.G., S.Y., S.P., S.H. and N.H. wrote the different part of the manuscript text and B.N.S. prepared figure and table. M.T.H. and M.H. conceptualized, supervised, reviewed and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hedayati, M.T., Ghazanfari, M., Shirvan, B.N. et al. Fungal Respiratory Colonization and Infections in Cystic Fibrosis Patients in the Middle East. Curr Fungal Infect Rep 18, 40–50 (2024). https://doi.org/10.1007/s12281-024-00486-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-024-00486-4