Abstract
Purpose of Review
This review highlights the important features of conidiobolomycosis infection and describes its presentation in pediatric population. The importance of a broaden differential diagnosis to include fungal infections taking into account the geographical location and history of exposure.
Recent Findings
There is evidence of conidiobolomycosis affecting not only immunocompetent hosts but also more susceptible individuals that can present with atypical or systemic/disseminated disease, including children.
Summary
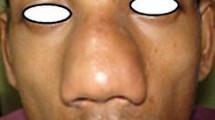
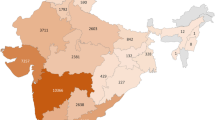
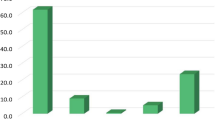
Conidiobolomycosis is a rare fungal infection caused by species of the genera Conidiobolus. It affects skin and soft tissue mainly from nasal and face location, though atypical presentation which consists of orbital/eye/maxillary sinus involvement and disseminated/systemic disease can be present. These forms of disease are more frequent in children and immunocompromised/chronic patients. Diagnosis should be established with culture and histopathology. Treatment is not standardized, but combination of antifungal drugs with surgical interventions has shown highest efficacy.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Vilela R, Mendoza L. Human pathogenic entomophthorales. Am Soc Microbiol. 2018;31:e00014–8 This paper provides a profound and updated review in the biology, taxonomic classification, physiopathology, clinical presentation and treatment strategies for entomophthoromycosis.
• Shaikh N, Hussain KA, Petraitiene R, Schuetz AN, Walsh TJ. Entomophthoramycosis: a neglected tropical mycosis. Clin Microbiol Infect. Elsevier Ltd; 2016;22:688–94. This paper provides a review on entomophthorales, it explains some theories concerning the low incidence of this fungal infection even though it affects immunocompetent hosts in tropical regions.
•• Choon SE, Kang J, Neafie RC, Ragsdale B, Klassen-Fischer M, Carlson JA. Conidiobolomycosis in a young malaysian woman showing chronic localized fibrosing leukocytoclastic vasculitis: a case report and meta-analysis focusing on clinicopathologic and therapeutic correlations with outcome. Am J Dermatopathol. 2012;34:511–22 This paper presents a meta-analysis of cases of entomophthoromycosis found in literature and analyses the epidemiological and clinical features of these cases. This paper also differentiates typical cutaneous involvement from atypical and systemic/disseminated disease.
Humber R. Entomophthoromycota: a new phylum and reclassification for entomophthoroid fungi. Mycotaxon. 2012;120:477–92.
Raveenthiran V, Mangayarkarasi V, Kousalya M, Viswanathan P, Dhanalakshmi M, Anandi V. Subcutaneous entomophthoromycosis mimicking soft-tissue sarcoma in children. J Pediatr Surg. Elsevier Inc.; 2015;50:1150–5.
Bras G, Gordon C, Emmons C, Prendegast K, Sugar M. A case of phycomycosis observed in Jamaica; infection with Entomphthora coronata. Am J Trop Med Hyg. 1965;14:141–5.
Mayorga J, Muñoz-Estrada F, Arosemena S. Infección nasal y paranasal por Conidiobolus coronatus. Primer caso en México. Rev Iberoam Micol. 1996:6–7.
•• Falces-Romero I, Alastruey-Izquierdo A, García-Rodríguez J. First isolation of Conidiobolus sp. in a respiratory sample of a patient in Europe. Clin Microbiol Infect. European Society of Clinical Microbiology and Infectious Diseases. 2017;23:834 This paper presents the molecular biology techniques for the identification of Conidiobolus sp. presents the first case of a patient from Germany with no history of traveling to tropical regions with isolation of Conidiobolus in a respiratory sample.
• Erker C, Huppler AR, Walsh TJ, McCormick ME, Suchi M, Bhatt NS, et al. Successful treatment of invasive conidiobolus infection during therapy for acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2018;40:e446–9 This paper presents the case of an immunocompromised patient the had a successful outcome with the use of antifungal treatment, surgery and the use of granulocyte transfusions.
• Temple ME, Brady MT, Koranyi KI, Nahata MC. Periorbital cellulitis secondary to Conidiobolus incongruus. Pharmacotherapy. 2001;21:351–4 This paper presents a pediatric case with good outcome.
Wüppenhorst N, Lee MK, Rappold E, Kayser G, Beckervordersandforth J, De With K, et al. Rhino-orbitocerebral zygomycosis caused by Conidiobolus incongruus in an immunocompromised patient in Germany. J Clin Microbiol. 2010;48:4322–5.
Kimura M, Yaguchi T, Sutton DA, Fothergill AW, Thompson EW, Wickes BL. Disseminated human conidiobolomycosis due to Conidiobolus lamprauges. J Clin Microbiol. 2011;49:752–6.
Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect European Society of Clinical Infectious Diseases. 2004;10:31–47.
Das SK, Das C, Maity AB, Maiti PK, Hazra TK, Bandyopadhyay SN. Conidiobolomycosis: an unusual fungal disease—our experience. Indian J Otolaryngol Head Neck Surg Springer India. 2019;71:1821–6.
Pestana J, Carmo A, Ribeiro JC, Tomé R. Chronic invasive rhinosinusitis by Conidiobolus coronatus, an emerging microorganism. J Mycol Med. 2019;29:67–70.
• Blumentrath CG, Grobusch MP, Matsiégui PB, Pahlke F, Zoleko-Manego R, Nzenze-Aféne S, et al. Classification of Rhinoentomophthoromycosis into atypical, early, intermediate, and late disease: a proposal. PLoS Negl Trop Dis. 2015;9:1–17 This paper proposes a classification for disease presentation in entomophthoromycosis.
Bonifaz A. Micología Médica Básica. cuarta edi. McGrawHil; 2012. p. 416–23.
• Pornpanich K, Uiprasertkul M, Luemsamran P, Jantharaworamet B, Vangveeravong S. Entomophthoramycosis: a rare fungal orbital infection presenting with dacryocystitis. Orbit. 2011;30:21–3 This paper presents a pediatric case from a tropical region with good outcome.
• Lithander J, Louon A, Scrimgeour E, Worthing E, Ganesh A. Orbital entomophthoramycosis in an infant: recovery following surgical debrodement, combination antifungal therapy and use of hyperaric oxygen. Br J Ophthalmol. 2000;154–8. This paper presents a pediatric case that was manage with combination of antifungal drugs, surgery, hyperbaric oxygen therapy and GM-CSF.
• Radhakrishnan N, Sachdeva A, Oberoi J, Prakash YS. Conidiobolomycosis in relapsed acute lymphoblastic leukemia. Pediatr Blood Cancer. 2009;53:1321–3 This paper presents a case of a immunocompromised pediatric patient with conidiobolomycosis with fatal outcome.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Deborah Palacios-Reyes and Alexandro Bonifaz declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Infections of Skin and Subcutaneous Tissue
Rights and permissions
About this article
Cite this article
Palacios-Reyes, D., Bonifaz, A. Conidiobolomycosis in Pediatric Patients. Curr Fungal Infect Rep 14, 203–208 (2020). https://doi.org/10.1007/s12281-020-00401-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-020-00401-7