Abstract
Syncope is defined as a transient loss of consciousness due to cerebral hypoperfusion, characterized by a rapid onset, short duration, and spontaneous complete recovery. It is usually a benign event, but sometimes it may represent the initial presentation of several cardiac disorders associated with sudden cardiac death during physical activity. A careful evaluation is essential particularly in young adults and in competitive athletes in order to exclude the presence of an underlying life-threatening cardiovascular disease. The present review analyzes the main non-cardiac and cardiac causes of syncope and the contribution of the available tools for differential diagnosis. Clinical work-up of the athlete with syncope occurring in extreme environments and management in terms of sports eligibility and disqualification are also discussed.


Similar content being viewed by others
References
Brignole, M., et al. (2018). 2018 ESC guidelines for the diagnosis and management of syncope. European Heart Journal, 39(21), 1883–1948.
Corrado, D., et al. (2003). Does sports activity enhance the risk of sudden death in adolescents and young adults? Journal of the American College of Cardiology, 42(11), 1959–1963.
Christou, G. A., Christou, K. A., & Kiortsis, D. N. (2018). Pathophysiology of noncardiac syncope in athletes. Sports Medicine, 48(7), 1561–1573.
Colivicchi, F., Ammirati, F., & Santini, M. (2004). Epidemiology and prognostic implications of syncope in young competing athletes. European Heart Journal, 25(19), 1749–1753.
Smith, J. J., Porth, C. M., & Erickson, M. (1994). Hemodynamic response to the upright posture. Journal of Clinical Pharmacology, 34(5), 375–386.
Christou, G. A., et al. (2016). A novel strategy for evaluating tilt test in athletes with syncope. European Journal of Preventive Cardiology, 23(9), 1003–1010.
Ogoh, S., et al. (2005). Dynamic cerebral autoregulation during exhaustive exercise in humans. American Journal of Physiology. Heart and Circulatory Physiology, 288(3), H1461–H1467.
Willie, C. K., et al. (2013). Maintained cerebrovascular function during post-exercise hypotension. European Journal of Applied Physiology, 113(6), 1597–1604.
Mundel, T., et al. (2015). Postexercise orthostatic intolerance: Influence of exercise intensity. Experimental Physiology, 100(8), 915–925.
Gisolf, J., et al. (2004). Tidal volume, cardiac output and functional residual capacity determine end-tidal CO2 transient during standing up in humans. The Journal of Physiology, 554(Pt 2), 579–590.
Olshansky, B. (1999). A Pepsi challenge. The New England Journal of Medicine, 340(25), 2006.
Flugelman, M., Halon, D. A., & Goldblatt, H. (1987). Golf syncope. Lancet, 2(8549), 47.
Krediet, C. T., et al. (2004). Exercise related syncope, when it's not the heart. Clinical Autonomic Research, 14(Suppl 1), 25–36.
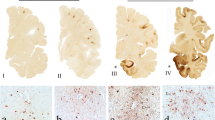
Corrado, D., et al. (2019). Arrhythmogenic right ventricular cardiomyopathy: Evaluation of the current diagnostic criteria and differential diagnosis. European Heart Journal. https://doi.org/10.1093/eurheartj/ehz669.
Marcus, F. I., et al. (2010). Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: Proposed modification of the Task Force Criteria. European Heart Journal, 31(7), 806–814.
D'Ascenzi, F., et al. (2018). Diagnostic Differentiation Between Arrhythmogenic Cardiomyopathy and Athlete'sHeart by Using Imaging. JACC: Cardiovascular Imaging, 11(9), 1327–1339.
Zorzi, A., et al. (2016). Arrhythmogenic right ventricular cardiomyopathy: Risk stratification and indications for defibrillator therapy. Current Cardiology Reports, 18(6), 57.
Finocchiaro, G., et al. (2019). The electrocardiogram in the diagnosis and management of patients with hypertrophic cardiomyopathy. Heart Rhythm, 17(1), 142–151. https://doi.org/10.1016/j.hrthm.2019.07.019.
Authors/Task Force, m, et al. (2014). 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). European Heart Journal, 35(39), 2733–2779.
di Gioia, C. R., et al. (2016). Nonischemic left ventricular scar and cardiac sudden death in the young. Human Pathology, 58, 78–89.
Zorzi, A., et al. (2016). Nonischemic left ventricular scar as a substrate of life-threatening ventricular arrhythmias and sudden cardiac death in competitive athletes. Circulation. Arrhythmia and Electrophysiology, 9(7). https://doi.org/10.1161/CIRCEP.116.004229.
Schnell, F., et al. (2016). Subepicardial delayed gadolinium enhancement in asymptomatic athletes: Let sleeping dogs lie? British Journal of Sports Medicine, 50(2), 111–117.
Cipriani, A., et al. (2019). Predictive value of exercise testing in athletes with ventricular ectopy evaluated by cardiac magnetic resonance. Heart Rhythm, 16(2), 239–248.
Corrado, D., et al. (2019). How to evaluate premature ventricular beats in the athlete: Critical review and proposal of a diagnostic algorithm. British Journal of Sports Medicine. https://doi.org/10.1136/bjsports-2018-100529.
Schwartz, P. J., Crotti, L., & Insolia, R. (2012). Long-QT syndrome: From genetics to management. Circulation. Arrhythmia and Electrophysiology, 5(4), 868–877.
Priori, S. G., et al. (2016). 2015 ESC Guidelines for the Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Revista Española de Cardiología (English Ed), 69(2), 176.
Brugada, J., et al. (2018). Present status of Brugada syndrome: JACC state-of-the-art review. Journal of the American College of Cardiology, 72(9), 1046–1059.
Pflaumer, A., & Davis, A. M. (2019). An update on the diagnosis and management of catecholaminergic polymorphic ventricular tachycardia. Heart, Lung & Circulation, 28(3), 366–369.
Grani, C., et al. (2017). Hybrid CCTA/SPECT myocardial perfusion imaging findings in patients with anomalous origin of coronary arteries from the opposite sinus and suspected concomitant coronary artery disease. Journal of Nuclear Cardiology, 24(1), 226–234.
Basso, C., et al. (2000). Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. Journal of the American College of Cardiology, 35(6), 1493–1501.
Pelliccia, A., et al. (1990). Coronary arteries in physiological hypertrophy: Echocardiographic evidence of increased proximal size in elite athletes. International Journal of Sports Medicine, 11(2), 120–126.
Zeppilli, P., et al. (1987). Echocardiographic visualization of the coronary arteries in endurance athletes. Giornale Italiano di Cardiologia, 17(11), 957–965.
Vettor, G., et al. (2015). Syncope as a warning symptom of sudden cardiac death in athletes. Cardiology Clinics, 33(3), 423–432.
Zorzi, A., Cipriani, A., & Corrado, D. (2018). Circumstances of cardiac arrest during sports activity recorded on video. European Journal of Preventive Cardiology, 25(13), 1452–1454.
Litovsky, S. H., & Antzelevitch, C. (1990). Differences in the electrophysiological response of canine ventricular subendocardium and subepicardium to acetylcholine and isoproterenol. A direct effect of acetylcholine in ventricular myocardium. Circulation Research, 67(3), 615–627.
Corrado, D., et al. (2006). Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA, 296(13), 1593–1601.
Sharma, S., et al. (2018). International recommendations for electrocardiographic interpretation in athletes. European Heart Journal, 39(16), 1466–1480.
Maron, B. J., et al. (2009). Sudden deaths in young competitive athletes: Analysis of 1866 deaths in the United States, 1980-2006. Circulation, 119(8), 1085–1092.
D'Ascenzi, F., et al. (2015). Exercise-induced left-ventricular hypertrabeculation in athlete's heart. International Journal of Cardiology, 181, 320–322.
Pelliccia, A., et al. (2018). European Association of Preventive Cardiology (EAPC) and European Association of Cardiovascular Imaging (EACVI) joint position statement: Recommendations for the indication and interpretation of cardiovascular imaging in the evaluation of the athlete's heart. European Heart Journal, 39(21), 1949–1969.
Palmieri, V., et al. (2018). Anomalous origin of coronary arteries from the "wrong" sinus in athletes: Diagnosis and management strategies. International Journal of Cardiology, 252, 13–20.
Pelliccia, A., Spataro, A., & Maron, B. J. (1993). Prospective echocardiographic screening for coronary artery anomalies in 1,360 elite competitive athletes. The American Journal of Cardiology, 72(12), 978–979.
Shen, W. K., et al. (2017). 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology, 70(5), 620–663.
Zipes, D. P., et al. (2005). Task Force 7: Arrhythmias. Journal of the American College of Cardiology, 45(8), 1354–1363.
Sirico, F., et al. (2019). Exercise stress test in apparently healthy individuals - where to place the finish line? The Ferrari corporate wellness programme experience. European Journal of Preventive Cardiology, 26(7), 731–738.
D'Ascenzi, F., et al. (2017). The prevalence and clinical significance of premature ventricular beats in the athlete. Scandinavian Journal of Medicine & Science in Sports, 27(2), 140–151.
van Dijk, N., et al. (2008). High diagnostic yield and accuracy of history, physical examination, and ECG in patients with transient loss of consciousness in FAST: The fainting assessment study. Journal of Cardiovascular Electrophysiology, 19(1), 48–55.
Brignole, M., et al. (2006). A new management of syncope: Prospective systematic guideline-based evaluation of patients referred urgently to general hospitals. European Heart Journal, 27(1), 76–82.
Sivakumaran, S., et al. (2003). A prospective randomized comparison of loop recorders versus Holter monitors in patients with syncope or presyncope. The American Journal of Medicine, 115(1), 1–5.
Ruwald, M. H., & Zareba, W. (2013). ECG monitoring in syncope. Progress in Cardiovascular Diseases, 56(2), 203–210.
Brignole, M., et al. (2006). Lack of correlation between the responses to tilt testing and adenosine triphosphate test and the mechanism of spontaneous neurally mediated syncope. European Heart Journal, 27(18), 2232–2239.
Deharo, J. C., et al. (2006). An implantable loop recorder study of highly symptomatic vasovagal patients: The heart rhythm observed during a spontaneous syncope is identical to the recurrent syncope but not correlated with the head-up tilt test or adenosine triphosphate test. Journal of the American College of Cardiology, 47(3), 587–593.
Maines, M., et al. (2018). Clinical impact, safety, and accuracy of the remotely monitored implantable loop recorder Medtronic reveal LINQTM. Europace, 20(6), 1050–1057.
Stein, K. M., et al. (2001). Formal analysis of the optimal duration of tilt testing for the diagnosis of neurally mediated syncope. American Heart Journal, 141(2), 282–288.
Kapoor, W. N., Smith, M. A., & Miller, N. L. (1994). Upright tilt testing in evaluating syncope: A comprehensive literature review. The American Journal of Medicine, 97(1), 78–88.
Hastings, J. L., & Levine, B. D. (2012). Syncope in the athletic patient. Progress in Cardiovascular Diseases, 54(5), 438–444.
Gati, S., Sharma, S., & Pennell, D. (2018). The role of cardiovascular magnetic resonance imaging in the assessment of highly trained athletes. JACC: Cardiovascular Imaging, 11(2 Pt 1), 247–259.
Nucifora, G., et al. (2014). Prevalence and prognostic value of concealed structural abnormalities in patients with apparently idiopathic ventricular arrhythmias of left versus right ventricular origin: A magnetic resonance imaging study. Circulation. Arrhythmia and Electrophysiology, 7(3), 456–462.
Andreini, D., et al. (2019). CMR for identifying the substrate of ventricular arrhythmia in patients with Normal echocardiography. JACC: Cardiovascular Imaging, 13(2 Pt 1), 410–421.
Pilichou, K., et al. (2016). Arrhythmogenic cardiomyopathy. Orphanet Journal of Rare Diseases, 11, 33.
Habib, M., Hoss, S., & Rakowski, H. (2019). Evaluation of hypertrophic cardiomyopathy: Newer Echo and MRI approaches. Current Cardiology Reports, 21(8), 75.
Fattori, R., et al. (2010). Significance of magnetic resonance imaging in apical hypertrophic cardiomyopathy. The American Journal of Cardiology, 105(11), 1592–1596.
Task Force, M., et al. (2013). 2013 ESC guidelines on the management of stable coronary artery disease: The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. European Heart Journal, 34(38), 2949–3003.
Berrettini, U., Trivelloni, P., & Patteri, G. (2010). Syncope in the hyperbaric environment. Giornale Italiano di Cardiologia (Rome), 11(10 Suppl 1), 122S–125S.
Craig Jr., A. B. (1961). Causes of loss of consciousness during underwater swimming. Journal of Applied Physiology, 16, 583–586.
Hong, S. K., et al. (1963). Diving pattern, lung volumes, and alveolar gas of the Korean diving woman (ama). Journal of Applied Physiology (Bethesda, MD: 1985), 18(3), 457–465.
Joulia, F., et al. (2013). Plasma adenosine release is associated with bradycardia and transient loss of consciousness during experimental breath-hold diving. International Journal of Cardiology, 168(5), e138–e141.
Berrettini, U., Landolfi, A., & Patteri, G. (2008). The heart in extreme sports: hyperbaric activity and microgravity. Giornale Italiano di Cardiologia (Rome), 9(10 Suppl 1), 94S–98S.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Associate Editor Domingo A. Pascual-Figal oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
D’Ascenzi, F., Zorzi, A., Sciaccaluga, C. et al. Syncope in the Young Adult and in the Athlete: Causes and Clinical Work-up to Exclude a Life-Threatening Cardiac Disease. J. of Cardiovasc. Trans. Res. 13, 322–330 (2020). https://doi.org/10.1007/s12265-020-09989-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-09989-0