Abstract
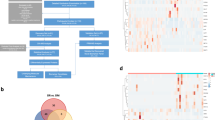
The vegetative state is a complex condition with unclear mechanisms and limited diagnostic, prognostic, and therapeutic methods. In this study, we aimed to explore the proteomic profile of tears from patients in a traumatic vegetative state and identify potential diagnostic markers using tears—a body fluid that can be collected non-invasively. Using iTRAQ quantitative proteomic technology, in the discovery phase, tear samples collected from 16 patients in a traumatic vegetative state and 16 normal individuals were analyzed. Among 1080 identified tear proteins, 57 were upregulated and 15 were downregulated in the patients compared to the controls. Bioinformatics analysis revealed that the differentially-expressed proteins were mainly involved in the wound response and immune response signaling pathways. Furthermore, we verified the levels of 7 differentially-expressed proteins in tears from 50 traumatic vegetative state patients and 50 normal controls (including the samples used in the discovery phase) using ELISA. The results showed that this 7-protein panel had a high discrimination ability for traumatic vegetative state (area under the curve = 0.999). In summary, the altered tear proteomic profile identified in this study provides a basis for potential tear protein markers for diagnosis and prognosis of the traumatic vegetative state and also provides novel insights into the mechanisms of traumatic vegetative state.






Similar content being viewed by others
References
van Erp WS, Lavrijsen JC, Vos PE, Bor H, Laureys S, Koopmans RT. The vegetative state: prevalence, misdiagnosis, and treatment limitations. J Am Med Dir Assoc 2015, 16: 85.e9–85.e14.
Monti MM, Laureys S, Owen AM. The vegetative state. BMJ 2010, 341: c3765.
Hazell AS. The vegetative state and stem cells: therapeutic considerations. Front Neurol 2016, 7: 118.
Marino S, Bramanti P. Neurofunctional imaging in differential diagnosis and evaluation of outcome in vegetative and minimally conscious state. Funct Neurol 2009, 24: 185–188.
Owen AM. Coleman MR. Functional neuroimaging of the vegetative state. Nat Rev Neurosci 2008, 9: 235–243.
Boly M, Tshibanda L, Vanhaudenhuyse A, Noirhomme Q, Schnakers C, Ledoux D, et al. Functional connectivity in the default network during resting state is preserved in a vegetative but not in a brain dead patient. Hum Brain Mapp 2009, 30: 2393–2400.
Coleman MR, Davis MH, Rodd JM, Robson T, Ali A, Owen AM, et al. Towards the routine use of brain imaging to aid the clinical diagnosis of disorders of consciousness. Brain 2009, 132: 2541–2552.
Schnakers C, Perrin F, Schabus M, Majerus S, Ledoux D, Damas P, et al. Voluntary brain processing in disorders of consciousness. Neurology 2008, 71: 1614–1620.
Monti MM, Coleman MR, Owen AM. Executive functions in the absence of behavior: functional imaging of the minimally conscious state. Prog Brain Res 2009, 177: 249–260.
Monti MM. Cognition in the vegetative state. Annu Rev Clin Psychol 2012, 8: 431–454.
Guler A, Kumral E, Sirin TC, Sirin H, Kitis O. Magnetic resonance imaging characteristics of persistent vegetative state due to prolonged hypoglycemia. J Clin Diagn Res 2015, 9: TD01–TD02.
Fernández-Espejo D, Norton L, Owen AM. The clinical utility of fMRI for identifying covert awareness in the vegetative state: a comparison of sensitivity between 3T and 1.5T. PLoS One 2014, 9: e95082.
Shen S, Loo RR, Wanner IB, Loo JA. Addressing the needs of traumatic brain injury with clinical proteomics. Clin Proteomics 2014, 11: 11.
Fraser DD, Close TE, Rose KL, Ward R, Mehl M, Farrell C, et al. Severe traumatic brain injury in children elevates glial fibrillary acidic protein in cerebrospinal fluid and serum. Pediatr Crit Care Med 2011, 12: 319–324.
Liliang PC, Liang CL, Weng HC, Lu K, Wang KW, Chen HJ, et al. Tau proteins in serum predict outcome after severe traumatic brain injury. J Surg Res 2010, 160: 302–307.
Zhou L, Beuerman RW. Tear analysis in ocular surface diseases. Prog Retin Eye Res 2012, 31: 527–550.
Zhou L, Zhao SZ, Koh SK, Chen L, Vaz C, Tanavde V, et al. In-depth analysis of the human tear proteome. J Proteomics 2012, 75: 3877–3885.
Von Thun Und Hohenstein-Blaul N, Funke S, Grus FH. Tears as a source of biomarkers for ocular and systemic diseases. Exp Eye Res 2013, 117: 126–137.
Chen W, Cao H, Lin J, Olsen N, Zheng SG. Biomarkers for primary Sjögren’s syndrome, genomics. Proteomics Bioinf 2015, 13: 219–223.
Zhou L, Beuerman RW, Chan CM, Zhao SZ, Li XR, Yang H, et al. Identification of tear fluid biomarkers in dry eye syndrome using iTRAQ quantitative proteomics. J Proteome Res 2009, 8: 4889–4905.
Böhm D, Keller K, Pieter J, Boehm N, Wolters D, Siggelkow W, et al. Comparison of tear protein levels in breast cancer patients and healthy controls using a de novo proteomic approach. Oncol Rep 2012, 28: 429–438.
Dartt DA. Interaction of EGF family growth factors and neurotransmitters in regulating lacrimal gland secretion. Exp Eye Res 2004, 78: 337–345.
Denisin AK, Karns K, Herr AE. Post-collection processing of Schirmer strip-collected human tear fluid impacts protein content. Analyst 2012, 137: 5088–5096.
Draghici S, Khatri P, Tarca AL, Amin K, Done A, Voichita C, et al. A systems biology approach for pathway level analysis. Genome Res 2007, 17: 1537–1545.
Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc 2009, 4: 44–57.
Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res 2010, 89: 219–229.
Guo Y, Lin C, Xu P, Wu S, Fu, X, Xia W, et al. AGEs Induced autophagy impairs cutaneous wound healing via stimulating macrophage polarization to M1 in diabetes. Sci Rep 2016, 6: 36416.
Jones SG, Edwards R, Thomas DW. Inflammation and wound healing: the role of bacteria in the immuno-regulation of wound healing. Int J Low Extrem Wounds 2014, 3: 201–208.
Thomas DR, Burkemper NM. Aging skin and wound healing. Clin Geriatr Med. 2013, 29: xi–xx.
Chen J, Chen Y, Yang Z, You B, Ruan YC, Peng Y. Epidermal CFTR suppresses MAPK/NF-κB to promote cutaneous wound healing. Cell Physiol Biochem 2016, 39: 2262–2274.
Grada A, Falanga V. Novel stem cell therapies for applications to wound healing and tissue repair. Surg Technol Int 2016, XXIX: 29–37.
Li AL, Zhang JD, Xie W, Strong JA, Zhang JM. Inflammatory changes in paravertebral sympathetic ganglia in two rat pain models. Neurosci Bull 2018, 34: 85–97.
Li D, Zhang L, Huang X, Liu L, He Y, Xu L, et al. WIP1 phosphatase plays a critical neuroprotective role in brain injury induced by high-altitude hypoxic inflammation. Neuroci Bull 2017, 33: 292–298.
Rathor MY, Rani MFA, Shahrin TCA, Hashim HZ. Persistent vegetative state after traumatic brain injury: a case report and review of the literature. Bangladesh J Med Sci 2014, 13: 19159.
Zhou L, Beuerman RW. The power of tears: how tear proteomics research could revolutionize the clinic (editorial). Exp Rev Proteomics 2017, 14: 189–191.
Acknowledgements
The work was supported by the National Natural Science Foundation of China (81671198), the Grant of Shanghai Municipal Education Commission-Gaofeng Clinical Medicine (20152212), and the Shanghai Shenkang Clinical Research Plan of the Shanghai Hospital Development Center (16CR3011A).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tang, Q., Zhang, C., Wu, X. et al. Comprehensive Proteomic Profiling of Patients’ Tears Identifies Potential Biomarkers for the Traumatic Vegetative State. Neurosci. Bull. 34, 626–638 (2018). https://doi.org/10.1007/s12264-018-0259-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12264-018-0259-x