Abstract
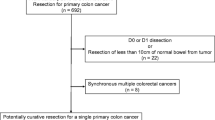
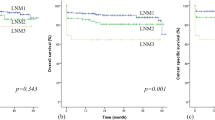
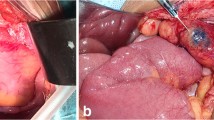
The objective of this study is to assess the success of lymph nodal harvest, extent of nodal spread in pericolic and apical stations, and factors affecting nodal metastasis in freshly resected colon cancer specimens. Following surgery, the lymph nodes were dissected off the specimen in the presence of an onco-pathologist. Apical lymph nodes were stationed according to “Japanese society of nodal classification for colon and rectum,” and pericolic lymph nodes were put into zones, proximally and distally, according to the distances from the tumor epicenter. Pathological analysis was done to see the pattern of nodal spread. Age, sex, T-stage, grade, and lymphovascular invasion (LVI) had no significant association with total lymph nodal yield. The chance of finding positive pericolic lymph nodes within proximal and distal 5 cm (p = 0.002 vs. p = 0.011) and proximal 5 to 10 cm (p = 0.010) of the tumor was significantly high. Beyond 10 cm proximal and 5 cm distal of the tumor epicentre, there were no pericolic positive nodes. Apical lymph nodal harvest rate was 74.64%, and positivity rate was 7% (5 out of 71). T-stage, grade, lymphovascular invasion (LVI), and perineural invasion (PNI) have statistically significant association with pericolic and apical node metastasis. In the fresh colonic specimen, pericolic nodal positivity beyond 10 cm proximal and 5 cm distal of tumor epicenter is rare. Apical and pericolic lymph node positivity is highly dependent upon multiple clinicopathological factors like T-stage, grade, and the presence of LVI and PNI. The lymph nodal yield is much better in fresh specimens by a surgeon under the supervision of a pathologist than fixed specimen. Trial Registered under Clinical Trials Registry-India (CTRI), REF/2019/05/025631.


Similar content being viewed by others
References
Sung H, Ferlay J et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality for 36 cancers in 185 countries. ACS J CA: A Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Bray F, Ferlay J et al (2018) Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
The Cancer Genome Atlas Network (2012) Comprehensive molecular characterization of human colon and rectal cancer. Nature 487:330–337
Guinney J, Dienstmann R et al (2015) The consensus molecular subtypes of colorectal cancer. Nat Med 21:1350–1356. https://doi.org/10.1038/nm.3967
Yaeger R, Chatila WK et al (2018) Clinical sequencing defines the genomic landscape of metastatic colorectal cancer. Cancer Cell 33:125-136.e3. https://doi.org/10.1016/j.ccell.2017.12.004
Dienstmann R, Vermeulen L et al (2017) Consensus molecular subtypes and the evolution of precision medicine in colorectal cancer. Nat Rev Cancer 17:79–92. https://doi.org/10.1038/nrc.2016.126
Zhang MR, Chi JL et al (2016) Prognostic role of the lymph node ratio in node positive colorectal cancer: a meta-analysis. Oncotarget. 7(45):72898–72907. https://doi.org/10.18632/oncotarget.12131
Ong MLH, Schofield JB (2016) Assessment of lymph node involvement in colorectal cancer. World J Gastrointestinal Surg 8(3):179–192. https://doi.org/10.4240/wjgs.v8.i3.179
Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma (2019) The 3rd English Edition, Journal of the Anus, Rectum and Colon 3(4):175–195. https://doi.org/10.23922/jarc.2019-018
Tsai HL, Huang C-W et al (2016) Factors affecting number of lymph nodes harvested and the impact of examining a minimum of 12 lymph nodes in stage I-III colorectal cancer patients: a retrospective single institution cohort study of 1167 consecutive patients. BMC Surg. 16:17. https://doi.org/10.1186/s12893-016-0132-7
Hamza A, Sakhi R et al (2018) Role of “second look” lymph node search in harvesting optimal number of lymph nodes for staging of colorectal carcinoma. Gastroenterol Res Practice 2018:6. https://doi.org/10.1155/2018/1985031
Bilimoria KY, Bentrem DJ et al (2008) Lymph node evaluation as a colon cancer quality measure: a national hospital report card. J Natl Cancer Inst 100(18):1310–1317. https://doi.org/10.1093/jnci/djn293
Gonen M, Schrag D, Weiser MR (2009) Nodal staging score: a tool to assess adequate staging of node-negative colon cancer. J Clin Oncol. 27(36):6166–6171. https://doi.org/10.1200/JCO.2009.23.7958
Guner OS, Tumay LV (2020) Higher cut-offs for the number of lymph nodes harvested do not predict better prognosis in patients with colon cancer. J Coloproctol 40(4):315–320. https://doi.org/10.1016/j.jcol.2020.06.009
Kazushige Kawai and Teppei Morikawa. (2018) The effect of formalin fixation on the size of pelvic sidewall lymph nodes. International Journal of Colorectal Disease 33(10); June 2018. https://doi.org/10.1007/s00384-018-3103-x.
Chen SL, Bilchik AJ (2006) More extensive nodal dissection improves survival for stages I to III of colon cancer: a population-based study. Ann Surg 244(4):602–610. https://doi.org/10.1097/01.sla.0000237655.11717.50
Vather R, Sammour T et al (2009) Lymph node examination as a predictor of long-term outcome in Dukes B colon cancer. Int J Colorectal Dis 24(3):283–288. https://doi.org/10.1007/s00384-008-0540-y
Appaiah NNB, Iqbal MR et al (2021) Clinicopathological factors affecting lymph node yield and positivity in left sided colon and rectal cancers. Cureus 13(10):19115. https://doi.org/10.7759/cureus.19115
Yuichiro Tsukada, Masaaki Ito (2022) Japanese D3 dissection in cancer of colon: technique and results. Chapter 12. The lymphatic system of colorectal cancer. 2022;193–214
Hideki Ueno and Kenichi Sugihara (2018) Japanese D3 dissection. Surgical treatment of colon cancer. 259–266. https://doi.org/10.1007/978-981-10-5143-2_23
Glasgow SC, Lowry AC et al (2012) Meta-analysis of histopathological features of primary colorectal cancers that predict lymph node metastases. J Gastrointest Surg. 16(5):1019–1028. https://doi.org/10.1007/s11605-012-1827-4
Park IJ, Choi GS et al (2009) Lymph node metastasis patterns in right-sided colon cancers: is segmental resection of these tumors oncologically safe? Ann Surg Oncol 16(6):1501–1506. https://doi.org/10.1245/s10434-009-0368-x
Toyota S, Ohta H, Anazawa S (1995) Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum 38(7):705–711. https://doi.org/10.1007/BF02048026
Chin CC, Yeh CY et al (2008) The oncologic benefit of high ligation of the inferior mesenteric artery in the surgical treatment of rectal or sigmoid colon cancer. Int J Colorectal Dis. 23(8):783–788. https://doi.org/10.1007/s00384-008-0465-5
Acknowledgements
We would like to record our acknowledgements and thanks to patients and to those who have contributed immensely to making this study as useful and purposeful as possible in its major objectives.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design: conceptualization—Dr. Chandramohan K., Dr. Sandeep Kumar Behera, and Dr. Madhu Muralee; methodology—Dr. Chandramohan K. and Dr. Sandeep Kumar Behera; material preparation and data collection—Dr. Sandeep Kumar Behera and Dr. Renu Sughosh; statistical analysis—K. M. Jagannath Krishna and Dr. Sandeep Kumar Behera; first draft of the manuscript written—Dr. Sandeep Kumar Behera; and writing, review, and editing—Dr. Chandramohan K and Dr. Sandeep Kumar Behera.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and scientific research committee.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Behera, S.K., Chandramohan. K., Muralee, M. et al. Determinants of Lymph Node Yield and Involvement in Resectable Colon Cancer: A Study of Anatomical, Pathological, and Fresh, Nonfixed Specimen Dissection. Indian J Surg 85, 1177–1183 (2023). https://doi.org/10.1007/s12262-023-03706-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-023-03706-2