Abstract
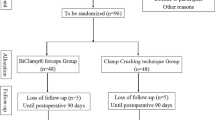
Liver resection is considered challenging because of the complex anatomy and abundant vascularity of the liver. Blood loss is an important determinant of outcome, and the risk of bleeding is highest during parenchymal transection. Various techniques and devices have been devised to improve accuracy and speed of parenchymal transection, while minimizing blood loss and collateral tissue damage. There has been a wide adoption of tissue-selective parenchymal transection devices for liver resection with growth of living donor liver transplantation. However, there is inconsistent and conflicting evidence regarding superiority of one device over the other. We compared two most commonly used tissue-selective parenchymal transection devices, Cavitron Ultrasonic Surgical Aspirator (CUSA) and Waterjet for differences in efficacy and adverse effects. A single-center prospective, randomized comparative trial was performed. Patients undergoing elective liver resections in the hepatobiliary and liver transplant unit of a tertiary referral hospital over 2 years were randomized to either the CUSA or Waterjet groups. Blood loss before, during, and after liver parenchymal transection were recorded. Postoperative adverse events, serial bilirubin, prothrombin time (PT) levels, and liver enzymes were monitored until discharge. Fifty patients were randomized equally between the CUSA and Waterjet groups. Parenchymal transection times for the Waterjet and CUSA were 181 SD12 min and 174 SD 7.8 min, respectively (p-value 0.6). Mean blood loss in the Waterjet and CUSA were 496.2 SD 48.66 mL and 471.5 SD 43.61 mL, respectively (p-value = 0.59). Peak aspartate transaminase (AST) levels in the Waterjet and CUSA were 386.32 SD 45.80 U/L and 389.84 SD 63.54 U/L, respectively. ALT levels in the Waterjet and CUSA were 348.76 SD 44.32 U/L and 339.24 SD 40.97 U/L (p = 0.87). Peak bilirubin levels in the Waterjet and CUSA groups were 3.076 SD 0.48 and 3.10 SD 0.39 mg/dL, respectively (p = 0.969). Peak prothrombin time in the postoperative period in the Waterjet and CUSA were 17.36 SD 0.40 and 18.24 SD 0.98 s, respectively (p = 0.414). The CUSA and Waterjet were similar in terms of time taken for liver parenchymal transection and blood loss. There was no significant difference in morbidity, mortality, or markers of hepatocyte injury with either technique. In the absence of a clear difference, availability and surgeon preference is likely to determine the choice of device for liver resections.

Similar content being viewed by others
References
Romano F, Garancini M, Uggeri F, Degrate L, Nespoli L, Gianotti L, Nespoli A, Uggeri F (2012) Bleeding in hepatic surgery: sorting through methods to prevent it. HPB Surgery 2012
Fan ST, Ng IO, Poon RT, Lo CM, Liu CL, Wong J (1999) Hepatectomy for hepatocellular carcinoma: the surgeon’s role in long-term survival. Arch Surg 134(10):1124–1130
Poon RT, Fan ST, Lo CM, Ng IO, Liu CL, Lam CM, Wong J (2001) Improving survival results after resection of hepatocellular carcinoma: a prospective study of 377 patients over 10 years. Ann Surg 234(1):63
Lesurtel M, Selzner M, Petrowsky H, McCormack L, Clavien PA (2005) How should transection of the liver be performed? A prospective randomized study in 100 consecutive patients: comparing four different transection strategies. Ann Surg 242(6):814
Yamamoto Y, Ikai I, Kume M, Sakai Y, Yamauchi A, Shinohara H, Morimoto T, Shimahara Y, Yamamoto M, Yamaoka Y (1999) New simple technique for hepatic parenchymal resection using a Cavitron Ultrasonic Surgical Aspirator® and bipolar cautery equipped with a channel for water dripping. World J Surg 23(10):1032–1037
Rau HG, Wichmann MW, Schinkel S, Buttler E, Pickelmann S, Schauer R, Schildberg FW (2001) Surgical techniques in hepatic resections: Ultrasonic aspirator versus Jet-Cutter A prospective randomized clinical trial. Zentralblatt fur Chirurgie 126(8):586–90
Takayama T, Makuuchi M, Kubota K, Harihara Y, Hui AM, Sano K, Ijichi M, Hasegawa K (2001) Randomized comparison of ultrasonic vs clamp transection of the liver. Arch Surg 136(8):922–928
Aldrighetti L, Pulitanò C, Arru M, Catena M, Finazzi R, Ferla G (2006) “Technological” approach versus clamp crushing technique for hepatic parenchymal transection: a comparative study. J Gastrointest Surg 10(7):974–979
Wrightson WR, Edwards MJ, McMasters KM (2000) The role of the ultrasonically activated shears and vascular cutting stapler in hepatic resection. Am Surg 66(11):1037
Koo BN, Kil HK, Choi JS, Kim JY, Chun DH, Hong YW (2005) Hepatic resection by the Cavitron Ultrasonic Surgical Aspirator® increases the incidence and severity of venous air embolism. Anesth Analg 101(4):966–970
Papachristou DN, Barters R (1982) Resection of the liver with a water jet. Br J Surg 69(2):93–94
Izumi R, Yabushita K, Shimizu K, Yagi M, Yamaguchi A, Konishi K, Nagakawa T, Miyazaki I (1993) Hepatic resection using a water jet dissector. Surg Today 23(1):31–35
Rau HG, Duessel AP, Wurzbacher S (2008) The use of water-jet dissection in open and laparoscopic liver resection. HPB 10(4):275–280
Sakamoto Y, Yamamoto J, Kokudo N, Seki M, Kosuge T, Yamaguchi T, Muto T, Makuuchi M (2004) Bloodless liver resection using the monopolar floating ball plus LigaSure diathermy: preliminary results of 16 liver resections. World J Surg 28(2):166–172
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205
Belghiti J, Hiramatsu K, Benoist S, Massault PP, Sauvanet A, Farges O (2000) Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg 191(1):38–46
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH (2002) Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 236(4):397
Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J (2004) Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg 240(4):698
Sun HC, Qin LX, Wang L, Ye QH, Wu ZQ, Fan J, Tang ZY (2005) Risk factors for postoperative complications after liver resection. Hepatobiliary Pancreat Dis Int 4(3):370–374
Wei AC, Tung-Ping Poon R, Fan ST, Wong J (2003) Risk factors for perioperative morbidity and mortality after extended hepatectomy for hepatocellular carcinoma. Br J Surg 90(1):33–41
Nakayama H, Masuda H, Shibata M, Amano S, Fukuzawa M (2003) Incidence of bile leakage after three types of hepatic parenchymal transection. Hepato- gastroenterology 50(53):1517–1520
Tanaka S, Hirohashi K, Tanaka H, Shuto T, Lee SH, Kubo S, Takemura S, Yamamoto T, Uenishi T, Kinoshita H (2002) Incidence and management of bile leakage after hepatic resection for malignant hepatic tumors. J Am Coll Surg 195(4):484–489
Nagano Y, Togo S, Tanaka K, Masui H, Endo I, Sekido H, Nagahori K, Shimada H (2003) Risk factors and management of bile leakage after hepatic resection. World J Surg 27(6):695–698
Pamecha V, Gurusamy KS, Sharma D, Davidson BR (2009) Techniques for liver parenchymal transection: a meta-analysis of randomized controlled trials. HPB 11(4):275–281
Arita J, Hasegawa K, Kokudo N, Sano K, Sugawara Y, Makuuchi M (2005) Randomized clinical trial of the effect of a saline-linked radiofrequency coagulator on blood loss during hepatic resection. Br J Surg 92:954–959
Smyrniotis V, Arkadopoulos N, Kostopanagiotou G, Farantos C, Vassiliou J, Contis J, Karvouni E (2005) Sharp liver transection versus clamp crushing technique in liver resections: a prospective study. Surgery 137(3):306–311
Lupo L, Gallerani A, Panzera P, Tandoi F, Di Palma G, Memeo V (2007) Randomized clinical trial of radiofrequency-assisted vs. clamp-crushing liver resection. Br J Surg 94:287–291
Author information
Authors and Affiliations
Contributions
Azaz Ahmed: conceptualization, methodology, investigation, writing—original draft.
Pardhasaradhi Paleela: writing—review and editing.
Pavan Kumar P B: writing—review and editing.
Nirmal J: writing—review and editing.
Anand Ramamurthy: visualization, conceptualization, methodology, writing—review and editing, supervision.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahmed, A., Paleela, P., P. B, P.K. et al. A Randomized Comparative Study of CUSA and Waterjet in Liver Resections. Indian J Surg 84 (Suppl 2), 390–397 (2022). https://doi.org/10.1007/s12262-022-03288-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03288-5