Abstract
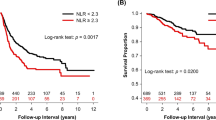
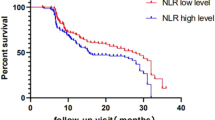
The relationship between chronic inflammation and cancer development is a known entity. There are many studies that have shown that inflammation is not only related to cancer pathogenesis but also to prognosis in the literature. Some serum inflammatory parameters such as neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), and lymphocyte-monocytes ratio (LMR) have been associated with survival in various types of cancer. The aim of this study was to investigate the prognostic relationship between resected non-small cell carcinomas and these parameters. Between January 2010 and December 2018, 693 patients who were operated without neo-adjuvant therapy were included in the study. The cutoff values for NLR, LMR, and PLR were determined by receiver operating curve (ROC) method. The patients were divided into high and low value groups, and Kaplan-Meier, log-rank, and Cox regression analyses were used to investigate the difference in survival between the groups. The optimal cutoff values for NLR, LMR, and PLR were 4.6, 2.95, and 141.2, respectively. In the high NLR group, the survival was significantly worse than in the low NLR group (HR, 1.81, p = 0.02). Similarly, the survival of the high PLR group was significantly poor (HR, 1.4, p = 0.002). On the contrary, OS was found to be significantly worse in the low LMR group generally for all stage and specific for each stage (HR, 2.0, p = 0.001). NLR, LMR, and PLR values obtained from the preoperative blood of the patients are a statistically significant prognostic factor for the survival of resected non-small cell lung cancer. In the prognosis estimation of the patients, inflammatory parameters can be specified besides the stage. Here, we investigated the prognostic significance of inflammatory parameters in surgically treated non-small cell lung cancer in a large series. The median and 5-year OS were found significantly worse in high NLR, high PLR, and low LMR groups. Furthermore, LMR is an independent prognostic factor for each stage of surgically treated non-small cell lung cancers.




Similar content being viewed by others
References
Yang L, He W, Kong P, Jiang C, Yang Q, Xie Q, Xia LP (2017) Clinical baseline and prognostic difference of platelet lymphocyte ratio (PLR) in right-sided and let-sided colon cancers. BMC Cancer 17:873. https://doi.org/10.1186/s12885-017-3862-8
Peng HX, Yang L, He BS, Pan YQ, Ying HQ, Sun HL et al (2017) Combination of preoperative NLR, PLR and CEA could increase the diagnostic efficacy for I-III stage CRC. J Clin Lab Anal 31. https://doi.org/10.1002/jcla.22075
Xia WK, Liu ZL, Shen D, Lin QF, Su J, Mao WD (2016) Prognostic performance of pre-treatment NLR and PLR in patients suffering from osteosarcoma. World J Surg Oncol 14:127. https://doi.org/10.1186/s12957-016-0889-2
Elyasinia F, Keramati MR, Ahmadi F, Rezaei S, Ashouri M, Parsaei R, Yaghoubi M, Elyasinia F, Aboutorabi A, Kaviani A (2017) Neutrophil-lymphocyte ratio in different stages of breast cancer. Acta Med Iran 55:228–232
Hu H, Yao X, Xie X, Wu X, Zheng C, Xia W et al (2017) Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J Urol 35:261–270. https://doi.org/10.1007/s00345-016-1864-9
Şahin F, Aslan AF (2018) Relationship between inflammatory and biological markers and lung cancer. J Clin Med 7:E160. https://doi.org/10.3390/jcm7070160
Deng M, Ma X, Liang X, Zhu C, Wang M (2017) Are pretreatment neutrophil-lymphocyte ratio and platelet-lymphocyte ratio useful in predicting the outcomes of patients with small-cell lung cancer? Oncotarget 8:37200–372007. https://doi.org/10.18632/oncotarget.16553
Gao L, Zhang H, Zhang B, Zhang L, Wang C (2017) Prognostic value of combination of preoperative platelet count and mean platelet volume in patients with resectable non-small cell lung cancer. Oncotarget 8:15632–15641. https://doi.org/10.18632/oncotarget.14921
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444. https://doi.org/10.1038/nature07205
Sanchez-Salcedo P, de-Torres JP, Martinez-Urbistondo D, Gonzalez-Gutierrez J, Berto J, Campo A et al (2016) The neutrophil to lymphocyte and platelet to lymphocyte ratios as biomarkers for lung cancer development. Lung Cancer 97:28–34. https://doi.org/10.1016/j.lungcan.2016.04.010
Goh BK, Kam JH, Lee SY, Chan CY, Allen JC, Jeyaraj P et al (2016) Significance of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and prognostic nutrition index as preoperative predictors of early mortality after liver resection for huge ( > / = 10 cm) hepatocellular carcinoma. J Surg Oncol 113:621–627. https://doi.org/10.1002/jso.24197
Van Egmond M, Bakema JE (2013) Neutrophils as effector cells for antibody-based immunotherapy of cancer. Semin Cancer Biol 23:190–199. https://doi.org/10.1016/j.semcancer.2012.12.002
Lan H, Zhou L, Chi D, Zhou Q, Tang X, Zhu D et al (2017) Preoperative platelet to lymphocyte and neutrophil to lymphocyte ratios are independent prognostic factors for patients undergoing lung cancer radical surgery: a single institutional cohort study. Oncotarget 8:35301–35310. https://doi.org/10.18632/oncotarget
Liu D, Huang Y, Li L, Song J, Zhang L, Li W (2017) High neutrophil-to-lymphocyte ratios confer poor prognoses in patients with small cell lung cancer. BMC Cancer 17:882. https://doi.org/10.1186/s12885-017-3893-1
Cedrés S, Torrejon D, Martínez A, Martinez P, Navarro A, Zamora E, Mulet-Margalef N, Felip E (2012) Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clin Transl Oncol 14:864–869. https://doi.org/10.1007/s12094-012-0872-5
Takahashi Y, Horio H, Hato T, Harada M, Matsutani N, Morita S, Kawamura M (2015) Prognostic significance of preoperative neutrophil–lymphocyte ratios in patients with stage I non-small cell lung cancer after complete resection. Ann Surg Oncol 22:S1324–S1331. https://doi.org/10.1245/s10434-015-4735-5
Thomas MR, Storey RF (2015) The role of platelets in inflammation. Thromb Haemost 114:449–458. https://doi.org/10.1160/TH14-12-1067
Ding N, Pang Z, Shen H, Ni Y, Du J, Liu Q (2016) The prognostic value of PLR in lung cancer, a meta-analysis based on results from a large consecutive cohort. Sci Rep 6:34823. https://doi.org/10.1038/srep34823
Han Y, Wang J, Hong L, Sun L, Zhuang H, Sun B, Wang H, Zhang X, Ren X (2017) Platelet-lymphocyte ratio is an independent prognostic factor in patients with ALK-positive non-small-cell lung cancer. Future Oncol 13:51–61. https://doi.org/10.2217/fon-2016-0317
Liu H, Wu Y, Wang Z, Yao Y, Chen F, Zhang H, Wang Y, Song Y (2013) Pretreatment platelet-to-lymphocyte ratio (PLR) as a predictor of response to first-line platinum-based chemotherapy and prognosis for patients with non-small cell lung cancer. J Thorac Dis 5:783–789. https://doi.org/10.3978/j.issn.2072-1439.2013.12.34
Pan YC, Jia ZF, Cao DH, Wu YH, Jiang J, Wen SM, Zhao D, Zhang SL, Cao XY (2018) Preoperative lymphocyte-to-monocyte ratio (LMR) could independently predict overall survival of resectable gastric cancer patients. Medicine (Baltimore) 97:e13896. https://doi.org/10.1097/MD.0000000000013896
Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y (2015) Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev 41:971–978. https://doi.org/10.1016/j.ctrv.2015.10.003
Lin JP, Lin JX, Cao LL, Zheng CH, Li P, Xie JW et al (2017) Preoperative lymphocyte-to-monocyte ratio as a strong predictor of survival and recurrence for gastric cancer after radical-intent surgery. Oncotarget 8:79234–79247. https://doi.org/10.18632/oncotarget.17058
Chen Y, Wang W, Zhang X, Yu X, Xi K, Wen Y, Wang G, Feng X, Zhang L (2018) Prognostic significance of combined preoperative platelet-to-lymphocyte ratio and lymphocyte-to-monocyte ratio in patients undergoing surgery with stage IB non-small-cell lung cancer. Cancer Manag Res 10:5411–5422. https://doi.org/10.2147/CMAR.S177320
Mao Y, Chen D, Duan S, Zhao Y, Wu C, Zhu F, Chen C, Chen Y (2018) Prognostic impact of pretreatment lymphocyte-to-monocyte ratio in advanced epithelial cancers: a meta-analysis. Cancer Cell Int 18:201. https://doi.org/10.1186/s12935-018-0698-5
Author information
Authors and Affiliations
Contributions
Muhammet Sayan, Aykut Kankoc, Nur Dilvin Ozkan, Aynur Bas, Ali Celik, Ismail Cuneyt Kurul, Olgun Kadir Aribas, and Abdullah Irfan Tastepe: conceptualization, study design, and project and writing management
Muhammet Sayan, Nur Dilvin Ozkan, Ali Celik, and Abdullah Irfan Tastepe: defining the study
Muhammet Sayan, Aykut Kankoc, Nur Dilvin Ozkan, and Aynur Bas: extensive literature search
Muhammet Sayan, Aykut Kankoc, Nur Dilvin Ozkan, Ali Celik, Ismail Cuneyt Kurul, Olgun Kadir Aribas, and Abdullah Irfan Tastepe performed the study, namely, experiments, practical work, and operative work
Muhammet Sayan, Aykut Kankoc, Nur Dilvin Ozkan, Ismail Cuneyt Kurul, Olgun Kadir Aribas, and Abdullah Irfan Tastepe: data acquisition
Muhammet Sayan, Aykut Kankoc, and Nur Dilvin Ozkan: data analysis. Muhammet Sayan and Aykut Kankoc: statistical inferences
Muhammet Sayan, Aykut Kankoc, Nur Dilvin Ozkan, and Ali Celik: manuscript writing
Ali Celik, Ismail Cuneyt Kurul, Olgun Kadir Aribas, and Abdullah Irfan Tastepe: repeated editing and reviewing
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was performed in Gazi University, Department of Thoracic Surgery, Ankara, Turkey.
Rights and permissions
About this article
Cite this article
Sayan, M., Kankoc, A., Ozkan, N.D. et al. Simple Peripheral Blood Cell Parameters to Predict Prognosis in Non-Small Cell Lung Cancer. Indian J Surg 83, 170–175 (2021). https://doi.org/10.1007/s12262-020-02237-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02237-4