Abstract
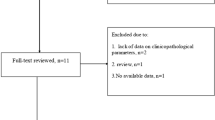
Delphian node (DLN) involvement is well known for its poor prognosis in laryngeal malignancies. With less than 10 studies available with respect to DLN and carcinoma thyroid, this prospective study to analyze the significance of DLN in management of thyroid carcinoma was planned. Study included 151 patients with histopathologically proven papillary carcinoma thyroid. Histopathological factors analyzed included size of the tumor, isthmus involvement, tumor capsule involvement, extrathyroidal extension, multifocality, lymphovascular invasion, thyroiditis, and pyramidal lobe association. DLN was harvested in 80 patients (53%). Seventeen patients (21.25%) had DLN metastasis. Male gender, capsular involvement, and extrathyroidal extension were independently associated with metastatic in DLN. DLN metastasis had accuracy of 83.8% to predict central compartment neck nodal involvement, risk of which is increased by 24.7 times compared to DLN with no nodal metastasis. Similarly, DLN metastasis is associated with an accuracy of 81.3% to predict lateral compartment neck nodal involvement risk of which is increased by 9.8 times compared to DLN with no nodal metastasis, both of which showed a significant p value of 0.0001. DLN involvement is a predictor of nodal metastasis which mandates an aggressive treatment and a close follow-up. When DLN is involved with total thyroidectomy with central compartment neck dissection has to be performed and lateral neck dissection is preferred on the side of disease when DLN is involved with capsular invasion, extrathyroidal extension and in case of male gender, after radiological correlation.

Similar content being viewed by others
References
Kim WW, Yang SI, Kim JH, Choi YS, Park YH, Kwon SK (2012) Experience and analysis of Delphian lymph node metastasis in patients with papillary thyroid carcinoma. World J Surg Oncol 10(1):226
Lan X, Sun W, Zhang H, Dong W, Wang Z, Zhang T (2015) A meta-analysis of central lymph node metastasis for predicting lateral involvement in papillary thyroid carcinoma. Otolaryngol Head Neck Surg 153(5):731–738
Wang YJ, Chu PY, Tai SK (2010) Ectopic thyroid papillary carcinoma presenting as bilateral neck masses. J Chin Med Assoc 73(4):219–221
Olsen KD, Desanto LW, Pearson BW (1987) Positive Delphian lymph node: clinical significance in laryngeal cancer. Laryngoscope 97(9):1033–1037
Isaacs JD, Lundgren CI, Sidhu SB, Sywak MS, Edhouse PJ, Delbridge LW (2008) The Delphian lymph node in thyroid cancer. Ann Surg 247(3):477–482
Shaha AR (2013) Thyroid cancer and Delphian node. Eur Arch Otorhinolaryngol 270:2381–2382
Dy BM, Shaha AR, Tuttle RM (2017) The Delphian Node revisited: an uncommon site of recurrence. J Endocr Soc 1(12):1527–1530
Chai YJ, Kim SJ, Choi JY, Koo DH, Lee KE, Youn YK (2014) Papillary thyroid carcinoma located in the isthmus or upper third is associated with Delphian lymph node metastasis. World J Surg 38(6):1306–1311
Isaacs JD, McMullen TP, Sidhu SB, Sywak MS, Robinson BG, Delbridge LW (2010) Predictive value of the Delphian and level VI nodes in papillary thyroid cancer. ANZ J Surg 80(11):834–838
Oh EM, Chung YS, Lee YD (2013) Clinical significance of Delphian lymph node metastasis in papillary thyroid carcinoma. World J Surg 37(11):2594–2599
Tan Z, Ge MH, Zheng CM, Wang QL, Nie XL, Jiang LH (2017) The significance of Delphian lymph node in papillary thyroid cancer. Asia Pac J Clin Oncol 13(5):e389–393
Iyer NG, Kumar A, Nixon IJ, Patel SG, Ganly I, Tuttle RM, Shah JP, Shaha AR (2011) Incidence and significance of Delphian node metastasis in papillary thyroid cancer. Ann Surg 253(5):988–991
Zheng G, Zhang H, Hao S, Liu C, Xu J, Ning J, Wu G, Jiang L, Li G, Zheng H, Song X (2017) Patterns and clinical significance of cervical lymph node metastasis in papillary thyroid cancer patients with Delphian lymph node metastasis. Oncotarget. 8(34):57089
Lee YC, Shin SY, Kwon KH, Eun YG (2013) Incidence and clinical characteristics of prelaryngeal lymph node metastasis in papillary thyroid cancer. Eur Arch Otorhinolaryngol 270(9):2547–2550
Murono S, Hirota K, Kondo S, Wakisaka N, Furukawa M, Yoshizaki T (2009) An extremely rare case of large Delphian node metastasis preceding primary laryngeal cancer. Auris Nasus Larynx 36(5):614–617
Ferlito A, Shaha AR, Rinaldo A (2002) Prognostic value of Delphian lymph node metastasis from laryngeal and hypopharyngeal cancer. Acta Otolaryngol 122(4):456–457
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Riju, J., George, N.A., Mony, R.P. et al. A Prospective Study to Find the Significance of Delphian Nodal Metastasis in Papillary Carcinoma Thyroid. Indian J Surg 82, 19–24 (2020). https://doi.org/10.1007/s12262-019-01888-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-019-01888-2