Abstract
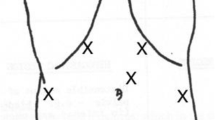
Laparoscopic Heller’s myotomy (LHM) and endoscopic balloon dilation are two main treatment modalities for achalasia cardia. The best treatment modality in Indian setting, however, is still unknown. Here, we present the early results of LHM in achalasia. Hospital data from January 2009 to October 2013 was analyzed. Preoperative assessment included Eckardt’s scoring, esophagogastroduodenoscopy, barium swallow examination, and esophageal manometry. Thirty-five patients (19 males and 16 females, median age 31 years, range 12–65) underwent LHM with partial fundoplication (with intraoperative endoscopy). All patients had dysphagia (median duration 48 months, range 1–240), and eight (22.8 %) had chest pain. Four (11 %) patients had recurrent achalasia. Most of the patients (80 %) came from rural areas, and 68.5 % were ≤40 years of age. Fundoplication was added in all except four patients (megaesophagus in one, left lobe hepatomegaly in one, and postsurgical recurrent achalasia in two). The median operative time was 180 min (range 120–300). Intraoperative complications included esophageal mucosal injury (n = 2) and pleural breach (n = 3) with one conversion. The median postoperative stay was 7 days (range 4–27) with a morbidity of 5.7 % (leak in one and subphrenic collection in one patient) and a mortality of 1 % (due to myocardial infarction). After a median follow-up of 9.5 months (range 1–47 months), four (11.4 %) patients had recurrent dysphagia and three (8.5 %) had gastroesophageal reflux. Most of the patients (six of eight) had relief in chest pain. To conclude, predominance of rural, young, and male patients in this study suggests that LHM might be the first-line treatment for achalasia in developing countries like India where predominant population is still rural that prefers one-time treatment, though it needs to be compared with a newly described procedure per oral endoscopic myotomy (POEM).
Similar content being viewed by others
References
Zaninotto G, Patti MG (2012) The never-ending story of dilatation versus surgery for oesophageal achalasia. Br J Surg 99:305–306
Boeckxstaens GE, Annese V, Varannes SB, Chaussade S, Costantini M, Cuttitta A et al (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816
Eckardt AJ, Eckardt VF (2011) Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol 8:311–319
Sugahara S, Ohara K, Yoshioka H (2006) Improvement of swallowing function in patients with esophageal cancer treated by radiology. J Jpn Soc Cancer Ther 31:1124–1130
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ (2008) Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 135:1526–1533
Allaix ME, Patti MG (2013) What is the best primary therapy for achalasia: medical or surgical treatment? Who owns achalasia? J Gastrointest Surg 17:1547–1549
Yaghoobi M, Mayrand S, Martel M, Afshar IR, Bijarchi R, Barkun A (2013) Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 78:468–475
Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108:1238–1249
Ghoshal UC, Rangan M (2011) A review of factors predicting outcome of pneumatic dilation in patients with achalasia cardia. J Neurogastroenterol Motil 17:9–13
Rohof WO, Boeckxstaens GE (2012) Treatment of the patient with achalasia. Curr Opin Gastroenterol 28:389–394
Ghoshal UC, Kumar S, Saraswat VA, Aggarwal R, Misra A, Choudhuri G (2004) Long-term follow-up after pneumatic dilation for achalasia cardia: factors associated with treatment failure and recurrence. Am J Gastroenterol 99:2304–2310
Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD (2012) SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 26:296–311
Palanivelu C, Maheshkumar GS, Jani K, Parthasarthi R, Sendhilkumar K, Rangarajan M (2007) Minimally invasive management of achalasia cardia: results from a single center study. JSLS 11:350–357
Parshad R, Hazrah P, Saraya A, Garg P, Makharia G (2008) Symptomatic outcome of laparoscopic cardiomyotomy without an antireflux procedure: experience in initial 40 cases. Surg Laparosc Endosc Percutan Tech 18:139–143
Pratap N, Kalapala R, Darisetty S, Joshi N, Ramchandani M, Banerjee R et al (2011) Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil 17:48–53
Biluts H, Ali A, Tena M (2007) Surgical treatment of achalasia cardia in Tikur Anbessa Hospital, Ethiopia. Ethiop Med J 45:267–273
Nadeem A, Ahmed H, Malik AM (2005) Surgical management and outcome in achalasia cardia. J Coll Physicians Surg Pak 15:644–645
Ahmed A, Yusufu LM, Ukwenya YA, Khalid L, Garba ES (2008) Surgical management of achalasia in Zaria, Northern Nigeria. S Afr J Surg 46:48–51
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Gupta, V., Hatimi, H., Kumar, S. et al. Laparoscopic Heller’s Myotomy for Achalasia Cardia: One-Time Treatment in Developing Countries?. Indian J Surg 79, 401–405 (2017). https://doi.org/10.1007/s12262-016-1496-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-016-1496-8