Abstract
Background
In Bulgaria, lung cancer incidence and mortality rates are rising in both men and women. The study aims to present a picture of lung cancer diagnosis and treatment process and to identify factors affecting survival in advanced lung cancer patients (LCP) treated with systemic therapy.
Patients and methods
Data from LCP admitted at the Medical Oncology Department were retrospectively collected from electronic and hard-paper database for a 10-year period (January 2005–2015). The test for frequencies was used to describe parameters. Kaplan–Mayer estimates with two-sided 95 % confidence interval (CI) were calculated for clinical and laboratory prognostic factors in advanced LCP who received medical therapy. Cox-regression model was used for the evaluation of significant prognostic factors’ impact on survival. Statistical analyses were performed using SPSS 9.0 software.
Results
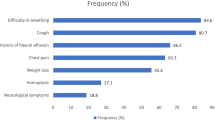
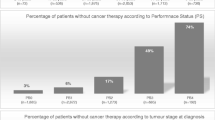
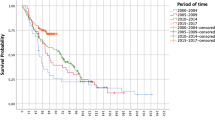
Data from 204 LCP were retrospectively analyzed for a period between January 2005 and January 2015. LCP characteristics were as follows: median age 60.2 years (range 28–78), male/female (M/F) 159/55, Eastern Cooperative Oncology Group (ECOG) performance status (PS) 0–1/> 2 136/63, no comorbidity/with comorbidity 36/168, smoking history never/ever 37/149; 86.3 % LCP had stage IIIB and IV disease. In 43.2 % of LCP with negative or not performed fibrobronchoscopy (FBS), pathological diagnosis was obtained by other methods including surgical. Before treatment, patients obtained morphological verification of lung cancer—98.5 % histologically versus 1.5 % cytologically. The prevalent histo-type found was adenocarcionoma. In all, 88.7 % of LCP received systemic medical treatment while 11.3 %—palliative care. Only 2.5 % received adjuvant and 2.0 % neoadjuvant chemotherapy, while 84.2 % received medical therapy for advanced disease. In the last group, prognostic value for survival according to Cox-regression model reached ECOG performance status (PS) (HR 0.4; CI 0.23–0.63; p < 0.0001); weight loss (WL) prior to diagnosis (HR 2.03; CI 1.22–3.37; p < 0.01); number of treatment lines (HR 1.65; CI 1.2–2.67; p < 0.05); and platelet to lymphocyte ratio (PLR) (HR 0.48;CI 0.24–0.95; p < 0.001).
Conclusions
Lung cancer diagnosis and treatment in Bulgaria are managed according to the European guidelines. ECOG PS and WL are known prognostic factors in advanced LCP. Our results support prognostic impact of PLR on survival. However, the confirmation of this finding needs further prospective validation. The fact that the number of treatment lines impacts survival point out the importance of “continuum of care” concept in advanced LCP, treated with medical therapy.





Similar content being viewed by others
References
Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Malvezzi M, Bertuccio P, Levi F, et al. European cancer mortality predictions for the year 2012. Ann Oncol. 2012;23:1044–52.
Cancer Incidence in Bulgaria 2010- National Cancer Registry, 2012: Vol.XX1;pp 18-20: Publisher Avia-24,Ltd.
M. Reck, S. Popat, N. Reinmuth, et al., on behalf of the ESMO Guidelines Working Group. Metastatic non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;00:1–13.
Hotta K, Fujiwara Y, Kiura K, et al. Relationship between response and survival in more than 50,000 patients with advanced non-small cell lung cancer treated with systemic chemotherapy in 143 phase III trials. J Thoracic Oncol. 2007;2:402–7.
Brundage MD, Davies D, Mackillop WJ Prognostic factors in non-small cell lung cancer: adecade of progress. Chest 2002;122:1037–57.
Kulesza P, Ramchandran K, Patel JD Emerging concepts in the pathology and molecular biology of advanced non-small cell lung cancer. Am J Clin Pathol. 2011;136: 228–38.
Ulas A, Turkoz FP, Silay K, et al. A laboratory prognostic index for patients with advanced non-small cell lung cancer. Plos One. 2014;9(12):e114471. doi:10.1371/journal.pone.0114471.
Kasymjanova G, MacDonald N, Agulnik JS, et al. The predictive value of pre-treatment inflammatory markers in advanced non-small-cell lung cancer. Curr Oncol. 2010;17(4):52–58.
Trape J, Montesinos J, Catot S, Buxo J, Franquesa J, et al. A prognostic score based on clinical factors and biomarkers for advanced non-small cell lung cancer. Int J Biol Markers. 2012;27(3):257–62.
Jafri SH, Shi R, Mills G. Advance lung cancer inflammation index (ALI) at diagnosis is a prognostic marker in patients with metastatic non-small cell lung cancer (NSCLC): a retrospective review. BMC Cancer. 2013;13:158–67.
Edge SB, Byrd DR, Compton CC, editor. AJCC Cancer Staging Handbook. 7th ed. New York: Springer, 2010
Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol. 2007;2:706–14.
Zhang Y, Kang S, Fang W, et al. Impact of smoking status on EGFR-TKI efficacy for advanced non-small-cell lung cancer in EGFR mutants: a meta-analysis. Clin Lung Cancer. 2014. doi:10.1016/j.cllc.2014.09.008. (pii: S1525–7304(14)00196–X)
O’Malley M, King AN, Conte M, et al. Effects of cigarette smoking on metabolism and effectiveness of systemic therapy for lung cancer. J Thorac Oncol. 2014;9(7):917–26. doi:10.1097/JTO.0000000000000191.
Bulgarian National Statistical Institute. http://www.nsi.bg. Accessed Jan 2015.
Biswas M, Ades AE, Hamilton W. Symptom lead times in lung and colorectal cancers: what are the benefits of symptom-based approaches to early diagnosis? Br J Cancer. 2015;112(2):271–7. doi:10.1038/bjc.2014.597.
National Comprehensive Cancer Network Guidelines V 2. 2013. http://www.nccn.org. Accessed May 11, 2013.
Goldberg RM, Rothenberg ML, Van Cutsem E, et al. The continuum of care: a paradigm for the management of metastatic colorectal cancer. Oncologist. 2007;12(1):38–50.
McMilan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care. 2009:12(3):223–6
Teramukai S, Kitano T, Kishida Y, Kawahara M, Kubota K, et al. Pretreatment neutrophil count as an independent prognostic factor in advanced non-small-cell lung cancer: an analysis of Japan Multinational Trial Organisation LC00–03. Eur J Cancer. 2009;5:1950–8.
Qiu M, Zhou Y, Jin Y, et al. Prognostic effect of high pretreatment neutrophil to lymphocyte ratio on survival of patients with gastric adenocarcinoma in China. Int J Bio Markers. 2014;30:e96–103. doi:10.5301/jbm.5000123.
Supoken A, Kleebkaow P, Chumworathayi B, et al. Elevated preoperative platelet to lymphocyte ratio associated with decreased survival of women with ovarian clear cell carcinoma. Asian Pac J Cancer Prev. 2014;15(24):10831–6.
Kusumanto Y, Dam W, Hospers G, et al. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 2003;6:283–7
Zhou X, Du Y, Huang Z, et al. Prognostic value of PRL in various cancers: a meta-analysis. PLoS One. 2014;9(6):e101119.
Author information
Authors and Affiliations
Corresponding author
Additional information
To my mentor Prof. Maurizio Tonato
Rights and permissions
About this article
Cite this article
Mihaylova, Z., Megdanova, V., Petrova, V. et al. Lung cancer in Bulgaria ‒ diagnosis, treatment, and factors affecting survival. memo 8, 136–143 (2015). https://doi.org/10.1007/s12254-015-0214-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12254-015-0214-8