Abstract
Venous thromboembolism is associated with substantial morbidity and mortality. Furthermore, the subsequently indicated anticoagulation treatment puts the patient at risk of possible bleeding complications. Therefore, improving treatment strategies as well as diagnostic approaches can optimize patient care. During the 55th Annual Meeting 2013 of the American Society of Hematology the Choosing Wisely® campaign was presented. An expert committee recommends against the test for thrombophilia after venous thromboembolism occurring in the setting of major transient risk factors to avoid over treatment in these patients. Other presentations focused on the use of the direct oral anticoagulants in patients with cancer-associated thromboembolism. However, specific studies comparing direct oral anticoagulants with the state-of the art treatment with low molecular heparins in cancer-associated thromboembolism are still missing. Finally, age-adjusted cut-off levels can increase the specificity of D-Dimer in older patients. Consequently, using clinical probability assessment in the combination with age-adjusted D-dimer cut-off levels may be associated with a larger number of patients in whom pulmonary embolism can be ruled out.
Similar content being viewed by others
Abbreviations
- ASH:
-
American Society of Hematology
- DOAC:
-
Direct oral anticoagulant
- LMWH:
-
Low-molecular-weight heparin
- UFH:
-
Unfractionated heparin
- VKA:
-
Vitamin K antagonist
- VTE:
-
Venous thromboembolism
References
Hicks LK, Bering H, Carson KR, et al. The ASH Choosing Wisely(R) campaign: five hematologic tests and treatments to question. Blood. 2013;122:3879–83.
Crowther MA, Ageno W, Garcia D, et al. Oral vitamin K versus placebo to correct excessive anticoagulation in patients receiving warfarin: a randomized trial. Ann Intern Med. 2009;150:293–300.
Crowther MA, Garcia D, Ageno W, et al. Oral vitamin K effectively treats international normalised ratio (INR) values in excess of 10. Results of a prospective cohort study. Thromb Haemost. 2010;104:118–21.
Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523–6.
Kyrle PA, Minar E, Bialonczyk C, et al. The risk of recurrent venous thromboembolism in men and women. N Engl J Med. 2004;350:2558–63.
Kyrle PA, Eischer L. Predicting the risk of recurrent venous thromboembolism. The Austrian study on recurrent venous thromboembolism (AUREC). Hamostaseologie. 2013;33:201–9.
Kyrle PA, Rosendaal FR, Eichinger S. Risk assessment for recurrent venous thrombosis. Lancet. 2010;376:2032–9.
Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e419S–94S.
Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361:2342–52.
Schulman S, Kearon C, Kakkar AK, et al. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med. 2013;368:709–18.
Buller HR, Decousus H, Grosso MA, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369:1406–15.
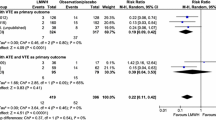
Schulman S, Kakkar AK, Goldhaber SZ, et al. Treatment of acute venous thromboembolism with dabigatran or warfarin and pooled analysis. Circulation. 2014;129:764–72.
Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349:146–53.
Blot E, Gutman F, Thannberger A. Dalteparin compared with an oral anticoagulant for thromboprophylaxis in patients with cancer. N Engl J Med. 2003;349:1385–7.
Rose AJ, Sharman JP, Ozonoff A, Henault LE, Hylek EM. Effectiveness of warfarin among patients with cancer. J Gen Intern Med. 2007;22:997–1002.
Short NJ, Connors JM. New oral anticoagulants and the cancer patient. Oncologist. 2014;19:82–93.
Farge D, Debourdeau P, Beckers M, et al. International clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. J Thromb Haemost. 2013;11:56–70.
Lyman GH, Khorana AA, Kuderer NM, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: american society of clinical oncology clinical practice guideline update. J Clin Oncol. 2013;31:2189–204.
Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001;135:98–107.
van Belle A, Buller, Huisman MV, et al. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006;295:172–9.
Klok FA, Mos IC, Nijkeuter M, et al. Simplification of the revised Geneva score for assessing clinical probability of pulmonary embolism. Arch Intern Med. 2008;168:2131–6.
Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the task force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008;29:2276–315.
Walston J, McBurnie MA, Newman A, et al. Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: results from the Cardiovascular Health Study. Arch Intern Med. 2002;162:2333–41.
Schouten HJ, Geersing GJ, Koek HL, et al. Diagnostic accuracy of conventional or age adjusted D-dimer cut-off values in older patients with suspected venous thromboembolism: systematic review and meta-analysis. BMJ. 2013;346:f2492.
Righini M, Van EJ, den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism: the ADJUST-PE study. JAMA. 2014;311:1117–24.
Take-home message
Thrombophilia screening should be used carefully to avoid overtreatment and, subsequently, possible harm in patients. Furthermore, the use of age-adjusted D-dimer cut-off levels in combination with clinical probability assessment may help to rule out PE.
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feistritzer, C., Wildner, S. Highlights of the American Society of Hematology Meeting 2013: hemostaseology. memo 7, 126–129 (2014). https://doi.org/10.1007/s12254-014-0157-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12254-014-0157-5