Abstract
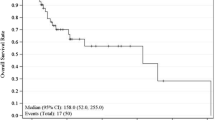
Cutaneous adnexal malignancies are biologically and pathologically diverse, and associated with a range of clinical outcomes. Given their rarity, the prognosis and optimal treatment of these neoplasms remains unclear. A single institution database from a tertiary care cancer center of patients treated for malignant cutaneous adnexal tumors was retrospectively analyzed. Clinicopathologic variables and outcome measures were analyzed in patients undergoing wide excision with or without sentinel node biopsy. 103 patients were analyzed; the majority of tumors were of eccrine sweat gland derivation (n = 69, 70%), and these exhibited a higher rate of nodal involvement and overall worse outcome. Sixteen patients (16%) demonstrated nodal metastasis, which included 10 (10%) with nodal disease at presentation and 6 who developed nodal metastasis during followup. 20 patients underwent sentinel node biopsy, and 2 (10%) had a positive sentinel node. 62% of nodal metastases occurred in patients with porocarcinoma. Seven patients died of disease (7%) with a median time from diagnosis to death of 48 months (range, 10–174). After a median follow up of 44.7 months, age > 70 years and larger tumor size were significantly associated with worse overall survival. Adnexal malignancies are rare tumors, and there is a paucity of information to guide the clinician in determining optimum surgical and medical treatment. Tumors of eccrine derivation, especially porocarcinomas, have a high risk of nodal involvement and may be considered for sentinel node biopsy.



Similar content being viewed by others
References
Edge SB (2010) American Joint Committee on Cancer. In: AJCC cancer staging manual, 7th edn. Springer, New York
Rogers HW, Weinstock MA, Harris AR et al (2010) Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol 146(3):283–287
Blake PW, Bradford PT, Devesa SS, Toro JR (2010) Cutaneous appendageal carcinoma incidence and survival patterns in the United States: a population-based study. Arch Dermatol 146(6):625–632
Martinez SR, Barr KL, Canter RJ (2011) Rare tumors through the looking glass: an examination of malignant cutaneous adnexal tumors. Arch Dermatol 147(9):1058–1062
Mallone S, De Vries E, Guzzo M et al (2012) Descriptive epidemiology of malignant mucosal and uveal melanomas and adnexal skin carcinomas in Europe. Eu J Ca 48(8):1167–1175
Stam H, Lohuis PJ, Zupan-Kajcovski B, Wouters MW, van der Hage JA, Visser O (2013) Increasing incidence and survival of a rare skin cancer in the Netherlands. A population-based study of 2,220 cases of skin adnexal carcinoma. J Surg Oncol 107(8):822–827
Ambe CMSV (2014) Sentinel lymph node biopsy in melanoma and other cutaneous malignancies. Am J Hematol Oncol 10(3):3–9
Bogner PN, Fullen DR, Lowe L et al (2003) Lymphatic mapping and sentinel lymph node biopsy in the detection of early metastasis from sweat gland carcinoma. Cancer 97(9):2285–2289
Delgado R, Kraus D, Coit DG, Busam KJ (2003) Sentinel lymph node analysis in patients with sweat gland carcinoma. Cancer 97(9):2279–2284
Breslow A (1970) Thickness, cross-sectional areas and depth of invasion in the prognosis of cutaneous melanoma. Ann Surg 172(5):902–908
Wright JR, Jr. Albert C. (2012) Broders' paradigm shifts involving the prognostication and definition of cancer. Arch Pathol Lab Med 136(11):1437–1446
Morton DL, Wen DR, Wong JH et al (1992) Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg (Chicago, Ill: 1960) 127(4):392–399
Ross MI, Reintgen D, Balch CM (1993) Selective lymphadenectomy: emerging role for lymphatic mapping and sentinel node biopsy in the management of early stage melanoma. Semin Surg Oncol 9(3):219–223
Ponti G, Losi L, Di Gregorio C et al (2005) Identification of Muir-Torre syndrome among patients with sebaceous tumors and keratoacanthomas: role of clinical features, microsatellite instability, and immunohistochemistry. Cancer 103(5):1018–1025
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no relevant conflict of interest.
Additional information
Synopsis
Cutaneous adnexal malignancies, which include eccrine and apocrine carcinomas, are rare skin neoplasms. Their clinical behavior as well as the role of sentinel lymph node biopsy in their staging and management remain poorly understood. This retrospective outcome addresses clinical behavior and prognosis in a large, retrospective well-curated single institution series.
Rights and permissions
About this article
Cite this article
Prieto-Granada, C., Castner, N., Chen, A. et al. Behavior of Cutaneous Adnexal Malignancies: a Single Institution Experience. Pathol. Oncol. Res. 26, 239–244 (2020). https://doi.org/10.1007/s12253-018-0427-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-018-0427-3