Abstract
Enteroviruses (EVs) species A are a major public health issue in the Asia–Pacific region and cause frequent epidemics of hand, foot and mouth disease (HFMD) in China. Mild infections are common in children; however, HFMD can also cause severe illness that affects the central nervous system. To molecularly characterize EVs, a prospective HFMD virological surveillance program was performed in China between 2013 and 2016. Throat swabs, rectal swabs and stool samples were collected from suspected HFMD patients at participating hospitals. EVs were detected using generic real-time and nested reverse transcription-polymerase chain reactions (RT-PCRs). Then, the complete VP1 regions of enterovirus A71 (EV-A71), coxsackievirus A16 (CVA16) and CVA6 were sequenced to analyze amino acid changes and construct a viral molecular phylogeny. Of the 2836 enrolled HFMD patients, 2,517 (89%) were EV positive. The most frequently detected EVs were CVA16 (32.5%, 819), CVA6 (31.2%, 785), and EV-A71 (20.4%, 514). The subgenogroups CVA16_B1b, CVA6_D3a and EV-A71_C4a were predominant in China and recombination was not observed in the VP1 region. Sequence analysis revealed amino acid variations at the 30, 29 and 44 positions in the VP1 region of EV-A71, CVA16 and CVA6 (compared to the respective prototype strains BrCr, G10 and Gdula), respectively. Furthermore, in 21 of 24 (87.5%) identified EV-A71 samples, a known amino acid substitution (D31N) that may enhance neurovirulence was detected. Our study provides insights about the genetic characteristics of common HFMD-associated EVs. However, the emergence and virulence of the described mutations require further investigation.
Similar content being viewed by others
Introduction
Non-polio Enteroviruses (EVs) are among the most prevalent viruses infecting humans. While most infections are asymptomatic, EVs can cause a broad spectrum of disease from mild to severe and even fatal illnesses. Hand, foot and mouth disease (HFMD) is mainly caused by EVs species A and represents an important public health problem in the Asia–Pacific region. China ranks first worldwide in terms of the case number and mortality of HFMD (Yu and Cowling 2019), and HFMD outbreaks have occurred annually in the past decade. Currently, no specific antiviral drugs are available for HFMD. Despite the availability and partial roll-out of an EV-A71 vaccine, approved for licensure in China in March 2016, the vaccine has no cross-protective effect with other EVs. Thus the burden of HFMD in China remains high (Li et al. 2018).
EVs are nonenveloped, single-stranded, positive-sense RNA viruses (https://www.viprbrc.org/brc/home.spg?decorator=picorna_entero) that encode four structural viral proteins (VPs): VP1, VP2, VP3, and VP4. Among these VPs, the VP1 region of EVs is most often used for genotyping (Harvala et al. 2018). EV-A71, the most common pathogen of severe HFMD, is divided into seven genogroups, A through G; eleven subgenogroups, B0 through B5 and C1 through C5; and two sublineages, C4a and C4b, based on the VP1 region (Iwai et al. 2009; Zhu et al. 2013; Le et al. 2019). The prototype strain for EV-A71 is BrCr. Coxsackievirus A16 (CVA16) is divided into two genogroups, A and B; two subgenogroups, B1 and B2; and three sublineages, B1a, B1b and B1c, also based on the VP1 region (Perera et al. 2007; Zhang et al. 2010; Ganorkar et al. 2017). The prototype strain for CVA16 is G10. Coxsackievirus A6 (CVA6) is divided into four genogroups, A through D; seven subgenogroups, B1 and B2, C1 and C2 and D1 through D3; and two sub-lineages, D3a and D3b (Song et al. 2017). The prototype strain for CVA6 is Gdula.
For both EV-A71 and CVA16, the important neutralizing/antigenic epitopes within the VP1 protein that are associated with viral infectivity have been established. These include the BC-, GH- and EF-loops and numerous residues (EV-A71: residues 31, 43, 98, 104, 106, 145, 164, 242 and 244; CVA16: residues 51-52, 98, 102-103, 218, 220, 241, 248, 251 and 295) (Huang et al. 2009; Cordey et al. 2012; Lu et al. 2012; Shi et al. 2013; Lyu et al. 2015; Arthur Huang et al. 2017; Song et al. 2017; Xu et al. 2018; Yao et al. 2018; Le et al. 2019). In contrast, because CVA6 is mostly associated with mild cases and difficult to culture, the corresponding sites and their properties have yet to be determined.
In China, previous HFMD outbreaks were mainly caused by EV-A71 and CVA16; however, CVA6 and CVA10 have emerged worldwide as important pathogens in recent years. Currently, CVA6 is the most commonly detected serotype in HFMD patients in China (Song et al. 2017). To provide a new perspective on viral diversity and identify new potential targets for drug and vaccine research, we conducted phylogenetic and variable site analyses of the VP1 protein of EV-A71, CVA16 and CVA6 viruses isolated from HFMD patients in China.
Materials and Methods
Virological Surveillance and Sampling
Before the introduction of the EV-A71 vaccine, a prospective virological surveillance program among children hospitalized with HFMD was established between October 2013 and September 2016. The program included three county-level hospitals and three township-level hospitals in Anhua County, Hunan Province, China (Gao et al. 2018). Details of the methods and results of the etiological investigations are described elsewhere (Gao et al. 2018).
Briefly, 2836 patients were enrolled, from whom 2827 throat swabs, 2583 rectal swabs and 778 stool samples were collected. Generic real-time reverse transcription-polymerase chain reaction (RT-PCR) was used to detect all EVs, and specific real-time RT-PCR was used to specifically detect EV-A71, CVA16 and CVA6. If a sample tested positive in the generic real-time RT-PCR but negative in the specific real-time RT-PCR, an additional nested RT-PCR was used to amplify a portion of the VP1 or VP4-VP2 regions for viral identification.
Selection of PCR-Positive Samples for Complete VP1 Sequencing
To select samples for VP1 sequencing, we first calculated the numbers of patients infected with each of the three serotypes (EV-A71, CVA16 and CVA6) by clinical sample type (stool sample, throat swab or rectal swab). These samples were further grouped by year and month of collection to identify specific time points for genotype switches (Ooi et al. 2007; Dolan et al. 2018). Finally, we applied a set of selection criteria to these categorized clinical samples to generate a final subsample for VP1 sequencing. The selection criteria were as follows: (1) For throat swabs, when ≥ 10 samples were available in a month, 10 clinical specimens were randomly selected, and when < 10 samples were available in a month all positive specimens were included; (2) For rectal swabs and stool samples, when > 2 samples were available in a month, 2 clinical specimens were randomly selected, and when ≤ 2 samples were available in a month, all positive specimens were included; (3) When both fecal and rectal swab samples were available, fecal samples were prioritized, and when fecal samples were not available, rectal swabs were included; and (4) Only one positive specimen was included per patient.
VP1 Sequencing of EV-A71, CVA16 and CVA6
Viral RNA was extracted using a QIAamp Viral RNA Mini Kit (QIAGEN, Hilden, Germany) and recovered in elution buffer, according to the manufacturer’s instructions. Nested RT-PCR amplification and sequencing of VP1 from the selected clinical samples were conducted using previously described PCR primers (Supplementary Table S1) (Perera et al. 2007; Zhang et al. 2009; Gaunt et al. 2015). In short, the first round amplification was performed in a 50 μL reaction volume using a SuperScript III One-Step RT-PCR Kit (Invitrogen, Carlsbad, CA, USA), with annealing temperatures of 50 °C for EV-A71, 45 °C for CVA16 and 55 °C for CVA6 over 40 cycles. CVA16 and CVA6 were amplified in a second round using DreamTaq Green PCR Master Mix (Invitrogen) under the same PCR conditions as the first-round in a 25 μL volume. The expected size of the PCR products was approximately 900 bp.
The obtained PCR products were sequenced bidirectionally using a Big Dye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems Inc., Foster City, CA, USA), using corresponding forward and reverse PCR primers in a 96-capillary 3730xl DNA Analyzer (Applied Biosystems). Sequences were confirmed by BLAST search (https://blast.ncbi.nlm.nih.gov/Blast.cgi).
Phylogenetic Analysis
For clarity, we first removed all sequences that were < 1% divergent from each other at the nucleotide level using the CD-HIT program (http://weizhong-lab.ucsd.edu/cdhit_suite/cgi-bin/) (Huang et al. 2010). Recombination was detected using a combination of methods (RDP, GENECONV, MaxChi, Chimaera, 3Seq, Bootscan and Siscan) within Recombination Detection Program version 4 (RDP4) with the default settings (Martin et al. 2015). Recombination was considered present when more than three of the above methods showed significant values (P < 0.05), and was reconfirmed by phylogenetic analysis. Sequence alignment was carried out using Geneious alignment in Geneious v7.1.3 (https://www.geneious.com). The maximum likelihood (ML) method available in IQ-TREE v1.4.3 was employed to reconstruct phylogenetic trees of the corresponding EVs serotypes (Nguyen et al. 2015). A bootstrap procedure with 10,000 replicates was used to assess the reliability of the obtained phylogenetic trees. Tree files were visualized using FigTree v1.4.3.
Detection of Amino Acid Substitutions
VP1 amino acid sequence analysis was conducted using PredictProtein (https://predictprotein.org/) (Yachdav et al. 2014). Selection pressure was measured by identifing instances of episodic positive selection, at the level of an individual site, using a mixed effects model of evolution (MEME) as previously described (http://www.datamonkey.org) (Murrell et al. 2012). To identify VP1-region amino acid changes in EV-A71, CVA16 and CVA6, sequences were compared to their respective reference strains (genotype A). All VP1 amino acid sequences obtained in this study were aligned.
Sequence Accession Numbers
The sequences obtained in this study were submitted to the NCBI under accession numbers MK306732 through MK307505.
Results
Overview of EVs Serotype Compositions
In total, 2836 HFMD patients were enrolled in our previous study. Using PCR methodologies, EVs that were eligible for genetic characterization in this study were detected in 2517 (89%) patients (Gao et al. 2018).
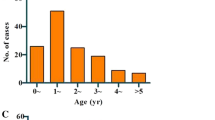
Among the 18 EVs serotypes identified, CVA16, CVA6 and EV-A71 were the most frequently detected, accounting for 32.5% (n = 819/2517), 31.2% (n = 785/2517) and 20.4% (n = 514/2517), respectively (Fig. 1A). Additionally, the serotypes were identified as follows: 5.9% (n = 149/2517) CVA10, 3.0% (n = 55/2517) CVA4, 1.6% (n = 40/2517) CVA8, 1.2% (n = 31/2517) CVA2, 0.5% (n = 12/2517) E18, 0.3% (n = 8/2517) CVA5, 0.3% (n = 8/2517) CVB5, 0.2% (n = 6/2517) CVB2, and 0.2% (5/2517) E9. Other EVs serotypes were detected in 2 or fewer patients.
Distribution of EV serotypes found in Anhua County, China, October 2013–September 2016. A Distribution of EV-A71, CVA16 and CVA6 HFMD in Anhua County, China, October 2013–September 2016. Total monthly numbers, samples planned for VP1 sequencing and successfully sequenced of B EV-A71, C CVA16, and D CVA6.
Phylogeny of VP1 Sequences of EV-A71, CVA16 and CVA6
According to the selection criteria, we selected 17% of the CVA16 isolates (n = 136/819), 23% of the CVA6 isolates (n = 181/785) and 28% of the EV-A71 isolates (n = 144/514) for complete VP1 sequencing. Then, we successfully obtained complete VP1 sequences from 76% of the CVA16 isolates (n = 103/136), 97% of the CVA6 isolates (n = 176/181) and 50% of the EV-A71 isolates (n = 72/144).
After the removal of identical sequences (where variation was < 1%), 24 EV-A71, 43 CVA16 and 65 CVA6 VP1 sequences remained for analysis (Fig. 1B–D, Table 1). All sequences fell within 3 subgenogroups: C4a for EV-A71, B1b for CVA16 and D3a for CVA6 (Figs. 2, 3 and 4).
Phylogenetic analyses of the entire VP1 sequences (891 bp) of EV-A71 from Anhua County based on ML methods. The tree was rooted on genotype A of the EV-A71 strain. The branches of sequences are color-coded according to the EV-A71 lineage. The names of the study sequences are colored in green; the reference strains are uncolored. Bootstrap values > 70% are shown on the branches. The phylogenetic tree indicates that evolutionary branch C4a was responsible for infections in Anhua County during 2013–2016.
Phylogenetic analyses of the entire VP1 sequences (891 bp) of CVA16 from Anhua County based on ML methods. The tree was rooted on genotype A of CVA16 strain. The branches of sequences are color-coded according to the CVA16 lineage. The names of the study sequences are colored in green; the reference strains are uncolored. Bootstrap values > 70% were shown on the branches. The phylogenetic tree indicates that evolutionary branch B1b was responsible for infections in Anhua County during 2013–2016.
Phylogenetic analyses of the entire VP1 sequences (891 bp) of CVA6 from Anhua County based on ML methods. The tree was rooted on genotype A of CVA6 strain. The branches of sequences are color-coded according to the CVA6 lineage. The names of the study sequences are colored in green; the reference strains are uncolored. Bootstrap values > 70% were shown on the branches. The phylogenetic tree indicates that evolutionary branch D3a was responsible for infections in Anhua County during 2013–2016.
Phylogeny of Other EVs
Partial VP1 region sequences of CVA10 (n = 119/149), CVA4 (n = 55/75), CVA8 (n = 38/40), CVA2 (n = 16/31), E18 (n = 10/12), CVB5 (n = 8/8), CVA5 (n = 7/8) and CVB2 (n = 6/6) were obtained (Table 1). After removing sequences with < 1% variation, partial VP1 sequences of CVA10 (n = 66/119), CVA4 (n = 29/55), CVA8 (n = 28/38), CVA2 (n = 11/16), E18 (n = 8/10), CVB5 (n = 8/8), CVA5 (n = 6/7) and CVB2 (n = 5/6) were included for analysis (Table 1). Following the calculation of similarity in terms of both nucleotides and amino acids, the results showed little variation (Supplementary Table S2). Thus, based on the phylogenetic tree and similarity analysis, these isolates clustered within their 8 subgenogroups: D, I-A, II, D, C, D2, E and 5.3 (Supplementary Figure S1-S8).
VP1 Deduced Amino Acid Sequence Analysis of EV-A71, CVA16 and CVA6
The remaining sequences were compared to reference prototype strains to identify variations at the amino acid level.
For the EV-A71 sequences, when compared to the prototype strain BrCr, 30 polymorphic amino acid sites were found. For the CVA16 sequences, when compared to the prototype strain G10, 29 polymorphic amino acid sites were found. For the CVA6, when compared to the prototype strain Gdula, 44 polymorphic amino acid sites were found (Figs. 5, 6 and 7, Supplementary Table S3).
Variations were found in EV-A71 (C4a) of our study. “-” indicates matching to the U22521/US/1970 (EV-A71 prototype strain, genotype A, BrCr type-strain). Variations potentially associated with major neutralizing/antigenicity epitopes are indicated in red. BC loop regions are indicated in green, EF loop regions are indicated in orange.
Variations were found in CVA6 (D3a) of our study. “-” indicates matching to the AY421764/US/1949 (CVA6 prototype strain, genotype A, Gdula type-strain). Variations potentially associated with major neutralizing/antigenicity epitopes are indicated in red. BC loop regions are indicated in green, EF loop regions are indicated in orange and GH loop regions are indicated in blue.
Additionally, we identified amino acid residue variations associated with major neutralization/antigenic epitopes. For the EV-A71 sequences, 87.5% (n = 21/24) of samples exhibited a substitution of aspartic acid (D) to asparagine (N) at residue 31 (D31N). Other substitutions were also found in the EV-A71 sequences: N104D/H (n = 2/24, 8%), R145E (n = 24/24, 100%), G239E (1/24, 4%), E244K (n = 24/24, 100%), S283T (15/24, 62.5%) and A293S/G (16/24, 66.7%) (Table 2).
For the CVA16 sequences, the substitutions L23I/M/V and I235V were found in 88.4% (n = 38) and 9.3% (n = 4) of the investigated samples (n = 43), respectively. Other substitutions were found in only one CVA16 sequence: P27S, L146X, V147S and T289A (Table 3).
For the CVA6 sequences, for which fewer major epitopes have been described in the literature, only small numbers of samples demonstrated amino acid substitutions; T96A (n = 2/65, 3%), S97N (n = 4/65, 6%), N137S/G/D (n = 16/65, 24.6%), T141A (1/65, 1.5%), V151I (1/65, 1.5%), G160N/S (n = 65/65, 100%), T205I (n = 1/65, 1.5%) and Q216H (n = 1/65, 1.5%) (Table 4).
Despite the variations described above, an analysis of selection pressure using MEME revealed that none of the protein-coding sequences showed adaptive evolution for EV-A71, CVA16 or CVA6.
Discussion
The present study describes the genetic characteristics of EVs serotypes associated with HFMD in Anhua County, Hunan Province, China, between 2013 and 2016. The VP1 protein plays a major role in the infectivity, replication and virulence of EVs and is the primary target for neutralizing antibodies. As such, monitoring surveillance of changes within the VP1 region of EVs may allow for the early identification of epidemiological and clinical changes, as well as the identification of potential novel vaccine targets.
All genogroups (or subgenogroups) of the EVs investigated in this study were consistent with the circulating strains reported in mainland China in recent years (Zhang et al. 2010; Baek et al. 2011; Hu et al. 2011; He et al. 2013; Zhang et al. 2013; Chen et al. 2016; Yang et al. 2016; Song et al. 2017; Zhang et al. 2017; Chen et al. 2018). We found that despite the complex epidemic patterns of HFMD recorded in Anhua County (Gao et al. 2018), each serotype investigated demonstrated long-term, population-level, persistent circulation of specific subgenogroups.
Since its first detection in 1998, EV-A71 subgenogroup C4 has persistently circulated in mainland China, while EV-A71 subgenogroup B5 has been reported only sporadically (Zhang et al. 2013). Notably, the C4a subgenogroup is now endemic to China and has been responsible for the ongoing nationwide HFMD outbreak since 2008. Further, our study indicates that C4a remains the single circulating EV-A71 subgenogroup. This finding is in contrast to the EVs circulation patterns reportrd in other areas, such as Taiwan (China), Japan, Singapore, Thailand and Vietnam, in which EV-A71 subgenogroup replacement has been frequently reported (Zhu et al. 2013; Linsuwanon et al. 2014; Le et al. 2019).
Similarly, the cocirculation of multiple lineages (e.g. B1a, B1b and/or B1c) of CVA16 has been observed in Taiwan (China), Malaysia, Thailand, Australia, Vietnam, and Japan (Zhang et al. 2010; Zhao et al. 2016; Sun et al. 2017), while subgenogroups have remained stable in mainland China. A previous analysis of CVA16 epidemic strains found that subgenotype B1 has been the dominant lineage in China since 2000 (Sun et al. 2017). Here, our phylogenetic analysis indicated that, the main circulating CVA16 subgenogroup between 2013 and 2016 was B1b.
In contrast to that of EV-A71 and CVA16, the molecular epidemiology of CVA6 detected in this study was similar to that in the broader Asian region. The emergence of CVA6 as a major cause of atypical HFMD worldwide has been associated specifically with genotype D (Song et al. 2017). HFMD-associated CVA6 subgenogroup D3 was first described following an outbreak in Finland in 2008, followed by other countries across Europe (Bian et al. 2015; Song et al. 2017). Subsequently, the D3 subgenogroup emerged in Asia, and was described from samples taken during outbreaks in Japan, Vietnam and other countries (Anh et al. 2018). In this study, we found that the D3a lineage was the predominant virus in China between 2013 and 2016, and no indication of other emerging subgenotypes was observed.
Although the identified EV-A71, CVA16 and CVA6 sequences belonged to a single subgenogroup across our study period, novel amino acid changes were also detected when compared to the sequences reported in previous molecular epidemiological studies. To our knowledge, amino acid substitutions in the EV-A71 VP1 region at sites Q48R, A54T/V, N104D/H, G239E, T295I/V/S and T296N have been described only in this study. Furthermore, we also found that the detected frequencies of polymorphic sites at positions S283T and A293S/G of the VP1 region were much higher than those in previous reports (van der Sanden et al. 2010; Le et al. 2019).
Interestingly, the amino acid variation D31N in the VP1 region of EV-A71 was previously reported to be associated with higher virulence and neurotropism (Zhang et al. 2014; Le et al. 2019). However, while the D31N mutation was present in most EV-A71 samples (21/24, 87.5%) in our study, all patients with EV-A71 were clinically mild cases, which indicates that D31N may not be the only factor or even a major factor determining the virulence of EV-A71. However, it is worth noting that although all enrolled patients in this study were hospitalized, only one enrolled patient had severe HFMD. This is due to the healthcare system structure in China, where rural healthcare insurance provides a larger proportional reimbursement for costs for inpatient care compared to outpatient care. As such, parents of sick children request hospital admission regardless of disease severity and physicians support these requests due to concern over the development of severe HFMD illness in seemingly mild cases. Unfortunately, this process restricted our ability to compare genetic variation between different groups of disease severity in this study.
Among CVA16 samples, we also detected novel variations at sites P27S, L146X and V147S of the VP1 region. Further, the previously reported variation at site L23I/M/V was detected at higher frequencies in our samples than in previous reports (Sun et al. 2017; Xu et al. 2018), which may be associated with local circulation and environmental factors. However, despite these findings, we did not detect a large degree of genetic diversity in CVA16 viruses, which is consistent with previous findings (Zhao et al. 2016).
CVA6 is a newly emerging virus that is often associated with milder cases and outbreaks of HFMD. Due to the emerging status of this virus, the variation analysisof CVA6 was based on known amino acid sequences and studies of EV-A71 and CVA16. Here, we detected ten variations in the VP1 region of CVA6 (sites 96-98, 102, 106, 151, 160, 165, 174 and 216), that are potentially associated with major neutralization/antigenic epitopes. Additionally, CVA6 samples from our study demonstrated higher rates of the amino acid variation G160N/S in the VP1 region than previously reported. Based on the same analysis method employed in this study, Kanbayashi et al. (2017) showed that only 68% (n = 17) of samples contained the G160N/S variation in the VP1 region. In contrast, 100% (n = 65) of our CVA6-positive samples contained this amino acid change. Furthermore, we detected previously unreported variations at sites 96-97, 141, 151, 165, 205 and 216, which were the main drivers of diversity within the VP1 regions of the CVA6 viruses found in our study.
The above variations in the VP1-region amino acids of EV-A71, CVA16 and CVA6 may contribute to future changes in virulence, antigenic properties or genotype switches in circulating EVs in China. However, because only mild clinical cases of HFMD were enrolled in our study, we could not compare genotype variations between HFMD severity groups. Furthermore, this study only investigated recombination in the VP1 region, while other groups of investigators studied the entire viral genome and found indicators of recombination more frequently occurring within nonstructural proteins (e.g., P2 and P3) (Oberste et al. 2004; McWilliam Leitch et al. 2012). Nevertheless, the data presented here may still contribute to drug target research and multivalent vaccine development.
In conclusion, this study has enriched the data on the genetic characteristics of multiple HFMD-associated EVs. EV-A71 subgenogroup C4a, CVA16 subgenogroup B1b and CVA6 subgenogroup D3a were the predominant EVs lineages in Anhua County, Hunan Province, China. This phylogenetic analysis of the main serotypes of EVs causing HFMD adds to our knowledge about enteroviral evolution and circulation. However, further research regarding amino acid variations and their effects on virulence, antigenic shifts and genotype switches of EVs is required.
References
Anh NT, Nhu LNT, Van HMT, Hong NTT, Thanh TT, Hang VTT, Ny NTH, Nguyet LA, Phuong TTL, Nhan LNT, Hung NT, Khanh TH, Tuan HM, Viet HL, Nam NT, Viet DC, Qui PT, Wills B, Sabanathan S, Chau NVV, Thwaites L, Rogier van Doorn H, Thwaites G, Rabaa MA, Van Tan L (2018) Emerging coxsackievirus a6 causing hand, foot and mouth disease, vietnam. Emerg Infect Dis 24:654–662
Arthur Huang KY, Chen MF, Huang YC, Shih SR, Chiu CH, Lin JJ, Wang JR, Tsao KC, Lin TY (2017) Epitope-associated and specificity-focused features of ev71-neutralizing antibody repertoires from plasmablasts of infected children. Nat Commun 8:762
Baek K, Yeo S, Lee B, Park K, Song J, Yu J, Rheem I, Kim J, Hwang S, Choi Y, Cheon D, Park J (2011) Epidemics of enterovirus infection in Chungnam Korea, 2008 and 2009. Virol J 8:297
Bian L, Wang Y, Yao X, Mao Q, Xu M, Liang Z (2015) Coxsackievirus A6: a new emerging pathogen causing hand, foot and mouth disease outbreaks worldwide. Expert Rev Anti Infect Ther 13:1061–1071
Chan YF, Wee KL, Chiam CW, Khor CS, Chan SY, Amalina WM, Sam IC (2012) Comparative genetic analysis of VP4, VP1 and 3D gene regions of enterovirus 71 and coxsackievirus A16 circulating in malaysia between 1997–2008. Trop Biomed 29:451–466
Chen L, Yang H, Wang C, Yao XJ, Zhang HL, Zhang RL, He YQ (2016) Genomic characteristics of coxsackievirus A8 strains associated with hand, foot, and mouth disease and herpangina. Arch Virol 161:213–217
Chen P, Wang H, Tao Z, Xu A, Lin X, Zhou N, Wang P, Wang Q (2018) Multiple transmission chains of coxsackievirus A4 co-circulating in china and neighboring countries in recent years: phylogenetic and spatiotemporal analyses based on virological surveillance. Mol Phylogenet Evol 118:23–31
Chia MY, Chung WY, Chiang PS, Chien YS, Ho MS, Lee MS (2014) Monitoring antigenic variations of enterovirus 71: implications for virus surveillance and vaccine development. PLoS Negl Trop Dis 8:e3044
Cordey S, Petty TJ, Schibler M, Martinez Y, Gerlach D, van Belle S, Turin L, Zdobnov E, Kaiser L, Tapparel C (2012) Identification of site-specific adaptations conferring increased neural cell tropism during human enterovirus 71 infection. PLoS Pathog 8:e1002826
Dolan PT, Whitfield ZJ, Andino R (2018) Mechanisms and concepts in RNA virus population dynamics and evolution. Ann Rev Virol 5:69–92
Ganorkar NN, Patil PR, Tikute SS, Gopalkrishna V (2017) Genetic characterization of enterovirus strains identified in hand, foot and mouth disease (HFMD): emergence of B1c, C1 subgenotypes, E2 sublineage of CVA16, EV71 and CVA6 strains in india. Infect Genet Evol 54:192–199
Gao L, Zou G, Liao Q, Zhou Y, Liu F, Dai B, Liu J, Chen Z, Xing W, Yang L, Liang H, Zhang Y, Chen Z, Luo L, Li Q, Luo K, Wu P, Mo X, Wang L, Lan K, Horby PW, Cowling BJ, Simmonds P, Altmeyer R, van Doorn HR, Yu H (2018) Spectrum of enterovirus serotypes causing uncomplicated hand, foot, and mouth disease and enteroviral diagnostic yield of different clinical samples. Clin Infect Dis 67:1729–1735
Gaunt E, Harvala H, Osterback R, Sreenu VB, Thomson E, Waris M, Simmonds P (2015) Genetic characterization of human coxsackievirus A6 variants associated with atypical hand, foot and mouth disease: a potential role of recombination in emergence and pathogenicity. J Gen Virol 96:1067–1079
Harvala H, Broberg E, Benschop K, Berginc N, Ladhani S, Susi P, Christiansen C, McKenna J, Allen D, Makiello P, McAllister G, Carmen M, Zakikhany K, Dyrdak R, Nielsen X, Madsen T, Paul J, Moore C, von Eije K, Piralla A, Carlier M, Vanoverschelde L, Poelman R, Anton A, Lopez-Labrador FX, Pellegrinelli L, Keeren K, Maier M, Cassidy H, Derdas S, Savolainen-Kopra C, Diedrich S, Nordbo S, Buesa J, Bailly JL, Baldanti F, MacAdam A, Mirand A, Dudman S, Schuffenecker I, Kadambari S, Neyts J, Griffiths MJ, Richter J, Margaretto C, Govind S, Morley U, Adams O, Krokstad S, Dean J, Pons-Salort M, Prochazka B, Cabrerizo M, Majumdar M, Nebbia G, Wiewel M, Cottrell S, Coyle P, Martin J, Moore C, Midgley S, Horby P, Wolthers K, Simmonds P, Niesters H, Fischer TK (2018) Recommendations for enterovirus diagnostics and characterisation within and beyond europe. J Clin Virol 101:11–17
He YQ, Chen L, Xu WB, Yang H, Wang HZ, Zong WP, Xian HX, Chen HL, Yao XJ, Hu ZL, Luo M, Zhang HL, Ma HW, Cheng JQ, Feng QJ, Zhao DJ (2013) Emergence, circulation, and spatiotemporal phylogenetic analysis of coxsackievirus A6- and coxsackievirus A10-associated hand, foot, and mouth disease infections from 2008 to 2012 in Shenzhen, China. J Clin Microbiol 51:3560–3566
Hu YF, Yang F, Du J, Dong J, Zhang T, Wu ZQ, Xue Y, Jin Q (2011) Complete genome analysis of coxsackievirus A2, A4, A5, and A10 strains isolated from hand, foot, and mouth disease patients in china revealing frequent recombination of human enterovirus a. J Clin Microbiol 49:2426–2434
Huang SW, Hsu YW, Smith DJ, Kiang D, Tsai HP, Lin KH, Wang SM, Liu CC, Su IJ, Wang JR (2009) Reemergence of enterovirus 71 in 2008 in Taiwan: dynamics of genetic and antigenic evolution from 1998 to 2008. J Clin Microbiol 47:3653–3662
Huang Y, Niu B, Gao Y, Fu L, Li W (2010) CD-HIT suite: a web server for clustering and comparing biological sequences. Bioinformatics 26:680–682
Iwai M, Masaki A, Hasegawa S, Obara M, Horimoto E, Nakamura K, Tanaka Y, Endo K, Tanaka K, Ueda J, Shiraki K, Kurata T, Takizawa T (2009) Genetic changes of coxsackievirus a16 and enterovirus 71 isolated from hand, foot, and mouth disease patients in Toyama, Japan between 1981 and 2007. Jpn J Infect Dis 62:254–259
Kanbayashi D, Kaida A, Yamamoto SP, Hirai Y, Kubo H, Fujimori R, Hakui N, Hirokawa H, Iritani N (2017) Impact of coxsackievirus a6 emergence on hand, foot, and mouth disease epidemic in osaka city, Japan. J Med Virol 89:2116–2121
Le TV, Nguyen VTT, Nguyen QH, Pham DT (2019) Molecular epidemiology analysis of enterovirus 71 strains isolated in dak lak, Vietnam, 2011–2016. J Med Virol 91:56–64
Li Y, Chang Z, Wu P, Liao Q, Liu F, Zheng Y, Luo L, Zhou Y, Chen Q, Yu S, Guo C, Chen Z, Long L, Zhao S, Yang B, Yu H, Cowling BJ (2018) Emerging enteroviruses causing hand, foot and mouth disease, China, 2010–2016. Emerg Infect Dis 24:1902–1906
Linsuwanon P, Puenpa J, Huang SW, Wang YF, Mauleekoonphairoj J, Wang JR, Poovorawan Y (2014) Epidemiology and seroepidemiology of human enterovirus 71 among Thai populations. J Biomed Sci 21:16
Liu N, Xie J, Qiu X, Jia L, Wu Z, Ma Y, Wang Z, Li P, Ren X, Hao R, Wang L, Wang Y, Qiu S, Song H (2014) An atypical winter outbreak of hand, foot, and mouth disease associated with human enterovirus 71, 2010. BMC Infect Dis 14:123
Lu J, Yi L, Zhao J, Yu J, Chen Y, Lin MC, Kung HF, He ML (2012) Enterovirus 71 disrupts interferon signaling by reducing the level of interferon receptor 1. J Virol 86:3767–3776
Lyu K, He YL, Li HY, Chen R (2015) Crystal structures of yeast-produced enterovirus 71 and enterovirus 71/coxsackievirus a16 chimeric virus-like particles provide the structural basis for novel vaccine design against hand-foot-and-mouth disease. J Virol 89:6196–6208
Martin DP, Murrell B, Golden M, Khoosal A, Muhire B (2015) RDP4: detection and analysis of recombination patterns in virus genomes. Virus Evol 1:vev003
McWilliam Leitch EC, Cabrerizo M, Cardosa J, Harvala H, Ivanova OE, Koike S, Kroes AC, Lukashev A, Perera D, Roivainen M, Susi P, Trallero G, Evans DJ, Simmonds P (2012) The association of recombination events in the founding and emergence of subgenogroup evolutionary lineages of human enterovirus 71. J Virol 86:2676–2685
Murrell B, Wertheim JO, Moola S, Weighill T, Scheffler K, Kosakovsky Pond SL (2012) Detecting individual sites subject to episodic diversifying selection. PLoS Genet 8:e1002764
Nguyen LT, Schmidt HA, von Haeseler A, Minh BQ (2015) IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol Biol Evol 32:268–274
Oberste MS, Maher K, Pallansch MA (2004) Evidence for frequent recombination within species human enterovirus b based on complete genomic sequences of all thirty-seven serotypes. J Virol 78:855–867
Ooi MH, Solomon T, Podin Y, Mohan A, Akin W, Yusuf MA, del Sel S, Kontol KM, Lai BF, Clear D, Chieng CH, Blake E, Perera D, Wong SC, Cardosa J (2007) Evaluation of different clinical sample types in diagnosis of human enterovirus 71-associated hand-foot-and-mouth disease. J Clin Microbiol 45:1858–1866
Perera D, Yusof MA, Podin Y, Ooi MH, Thao NT, Wong KK, Zaki A, Chua KB, Malik YA, Tu PV, Tien NT, Puthavathana P, McMinn PC, Cardosa MJ (2007) Molecular phylogeny of modern coxsackievirus A16. Arch Virol 152:1201–1208
Shi J, Huang X, Liu Q, Huang Z (2013) Identification of conserved neutralizing linear epitopes within the VP1 protein of coxsackievirus A16. Vaccine 31:2130–2136
Song Y, Zhang Y, Ji T, Gu X, Yang Q, Zhu S, Xu W, Xu Y, Shi Y, Huang X, Li Q, Deng H, Wang X, Yan D, Yu W, Wang S, Yu D, Xu W (2017) Persistent circulation of coxsackievirus A6 of genotype D3 in mainland of china between 2008 and 2015. Sci Rep 7:5491
Sun Z, Zhang G, Guo P, Liu J, Gao Q, Xu X, Gong L (2017) Epidemiological characterizations, pathogen spectrum and molecular characteristics of coxsackievirus A16 from patients with HFMD in Yantai, Shandong, China between 2011 and 2015. Hum Vaccin Immunother 13:1831–1838
van der Sanden S, van der Avoort H, Lemey P, Uslu G, Koopmans M (2010) Evolutionary trajectory of the VP1 gene of human enterovirus 71 genogroup b and c viruses. J Gen Virol 91:1949–1958
Xu L, Cui D, Wang L, Cheng J, Sun C, Li L, Cao H (2018) Genetic characteristics of the P1 coding region of coxsackievirus A16 associated with hand, foot, and mouth disease in China. Mol Biol Rep 45:1947
Yachdav G, Kloppmann E, Kajan L, Hecht M, Goldberg T, Hamp T, Honigschmid P, Schafferhans A, Roos M, Bernhofer M, Richter L, Ashkenazy H, Punta M, Schlessinger A, Bromberg Y, Schneider R, Vriend G, Sander C, Ben-Tal N, Rost B (2014) Predictprotein–an open resource for online prediction of protein structural and functional features. Nucleic Acids Res 42:W337–343
Yang Q, Zhang Y, Yan D, Zhu S, Wang D, Ji T, Li X, Song Y, Gu X, Xu W (2016) Two genotypes of coxsackievirus A2 associated with hand, foot, and mouth disease circulating in china since 2008. PLoS ONE 11:e0169021
Yao X, Mao Q, Li Y, Hao C, Bian L, Chen P, Gao F, Wu X, Lu W, Gao Q, Li X, Liang Z (2018) Poorly neutralizing polyclonal antibody in vitro against coxsackievirus a16 circulating strains can prevent a lethal challenge in vivo. Hum Vaccin Immunother 14:1275–1282
Yu H, Cowling BJ (2019) Remaining challenges for prevention and control of hand, foot, and mouth disease. Lancet Child Adolesc Health 3:373–374
Zhang Y, Tan XJ, Wang HY, Yan DM, Zhu SL, Wang DY, Ji F, Wang XJ, Gao YJ, Chen L, An HQ, Li DX, Wang SW, Xu AQ, Wang ZJ, Xu WB (2009) An outbreak of hand, foot, and mouth disease associated with subgenotype c4 of human enterovirus 71 in shandong, china. J Clin Virol 44:262–267
Zhang Y, Wang D, Yan D, Zhu S, Liu J, Wang H, Zhao S, Yu D, Nan L, An J, Chen L, An H, Xu A, Xu W (2010) Molecular evidence of persistent epidemic and evolution of subgenotype B1 coxsackievirus A16-associated hand, foot, and mouth disease in china. J Clin Microbiol 48:619–622
Zhang Y, Tan X, Cui A, Mao N, Xu S, Zhu Z, Zhou J, Shi J, Zhao Y, Wang X, Huang X, Zhu S, Zhang Y, Tang W, Ling H, Xu W (2013) Complete genome analysis of the C4 subgenotype strains of enterovirus 71: predominant recombination C4 viruses persistently circulating in china for 14 years. PLoS ONE 8:e56341
Zhang B, Wu XB, Huang KY, Li L, Zheng L, Wan CS, He ML, Zhao W (2014) The variations of VP1 protein might be associated with nervous system symptoms caused by enterovirus 71 infection. BMC Infect Dis 14:243
Zhang J, Zhang H, Zhao Y, Guo C, Yang Z, Ma S (2017) Molecular characterization of a new human coxsackievirus B2 associated with severe hand-foot-mouth disease in yunnan province of china in 2012. Arch Virol 162:307–311
Zhao G, Zhang X, Wang C, Wang G, Li F (2016) Characterization of VP1 sequence of coxsackievirus A16 isolates by bayesian evolutionary method. Virol J 13:130
Zhu J, Luo Z, Wang J, Xu Z, Chen H, Fan D, Gao N, Ping G, Zhou Z, Zhang Y, An J (2013) Phylogenetic analysis of enterovirus 71 circulating in beijing, china from 2007 to 2009. PLoS ONE 8:e56318
Acknowledgements
We thank staff members of the Anhua County-, Yiyang Prefecture-, and Hunan Provincial-level departments of health for providing assistance with administration and data collection; staff members at the Anhua County-, Yiyang Prefecture-, and Hunan Provincial-level CDCs and six study hospitals (Anhua People’s Hospital, Anhua Second People’s Hospital, Anhua Hospital of TCM, Tianzhuang Township Hospital, Jiangnan Township Hospital, and Qingtang Township Hospital) for providing assistance with field investigation, administration and data collection. This work was supported by the National Science and Technology Major Project of China (No. 2018ZX10201001-010, No. 2017ZX10103009-005, No. 2018ZX10713001-007), the National Natural Science Fund for Distinguished Young Scholars of China (No. 81525023), the National Natural Science Foundation of China (No. 81473031), the Program of Shanghai Academic/Technology Research Leader (No. 18XD1400300), the Li Ka Shing Oxford Global Health Programme (No. B9RST00-B900.57), the Chinese Preventive Medicine Association (No: 20101801). JC is supported by CAS Pioneer Hundred Talents Program.
Author information
Authors and Affiliations
Contributions
HJY conceptualized, designed and supervised the study. KWL, QHL, PL, MH and SBY coordinated and participated in data collection. YHZ, LLW and QQ performed the experiments. GZ, NTA, NTTH, XW, TTL and JC provided laboratory technical support. YHZ and LVT wrote the first draft of the manuscript. HJY, HRD and LVT revised the manuscript. All authors contributed to review and revision and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
HJY has received investigator-initiated research funding from Sanofi Pasteur, GlaxoSmithKline, and Yichang HEC Changjiang Pharmaceutical Company, none of which is related to HFMD and enteroviruses.
Animal and Human Rights Statement
This study was approved by the ethical review committees at the Chinese Center for Disease Control and Prevention, World Health Organization Regional Office for the Western Pacific, and the School of Public Health, Fudan University (Gao et al. 2018). Informed verbal consent was obtained from all individual patients’ parents/guardians included in the study (Gao et al. 2018).
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, Y., Van Tan, L., Luo, K. et al. Genetic Variation of Multiple Serotypes of Enteroviruses Associated with Hand, Foot and Mouth Disease in Southern China. Virol. Sin. 36, 61–74 (2021). https://doi.org/10.1007/s12250-020-00266-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12250-020-00266-7