Abstract
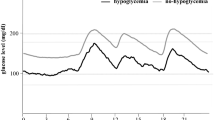
The aim of this study was to compare the difference of blood glucose (BG) fluctuation in the patients of type-2 diabetes mellitus (DM-2) with and without clinical diagnosed diabetic nephropathy (DN) by the continuous glucose monitoring system (CGMS). Thirty DM-2 patients with clinical diagnosed DN and fifteen DM-2 patients without complication underwent continuous glucose monitoring for 3 days (72 h) by CGMS. The difference of daily glucose fluctuation in both groups was compared by the parameter of CGMS. The 24-h mean blood glucose (MBG), minimal BG (MIN-BG), area under curve of BG over 7.8 (AUC7.8), percentage of time of BG over 7.8 (PT7.8), area under curve of BG over 11.1 (AUC11.1), percentage of time of BG over 11.1 (PT11.1), as well as mean of daily difference (MODD) were significantly increased in the group of DN, compared with those in the group of DM-2 without complication (all statistic probability P <0.05). No statistical significance of mean amplitude of glycaemic excursion (MAGE) was found. In the group of DN, MBG, standard deviation of blood glucose (SDBG), large amplitude of glycaemic excursion (LAGE), AUC7.8, PT7.8, AUC11.1, PT11.1, MAGE and MODD were (10.7±1.9)mmol/L, (2.5±1.3)mmol/L, (9.2±3.9)mmol/L, 3.2±1.7, (81±18)%, 1.2±1.0, (42±24)%, (5.8±2.5)mmol/L and (2.6±1.5)mmol/L, respectively. The study showed that the BG level of the patients with DN fluctuated throughout the day. MBG of the patients with DN was higher than that of the patients of DM-2 without complications, with the characteristics of long-lasting high BG period, dramatic instability during the day and especially high postprandial blood glucose. CGMS is a useful tool for physicians to know the details of the change of BG in the patients with DN.
Similar content being viewed by others
References
Song M, Alexander C M, Mavros P, et al. Use of the UKPDS outcomes model to predict all-cause mortality in U.S. adults with type-2 diabetes mellitus: Comparison of predicted versus observed mortality [J]. Diabetes Research and Clinical Practice, 2011, 91(1): 121–126.
Kaufman F R, Gibson L C, Havalvorson M, et al. A pilot study of the continuous glucose monitoring system: Clinical decisions and glycemic control after its use in pediatric type 1 diabetic subjects [J]. Diabetes Care, 2001, 24(12): 2034.
American Diabetes Association. Standards of medical care in diabetes [J]. Diabetes Care, 2004, 27(S1):15–35.
Bonakdaran S, Rajabian R. Prevalence and extent of glycemic excursions in well-controlled patients with type 2 diabetes mellitus using continuous glucosemonitoring system [J]. Indian Journal of Medical Science, 2009, 63(2): 66–71.
Rimondi F, Banin P, Gamberini M R, et al. The continuous glucose monitoring system (CGMS) in patients with beta-thalassemia major and impaired glucose homeostasis: Preliminary results [J]. Pediatric Endocrinology Reviews, 2008, 6(S1): 190–192.
Derosa G, Salvadeo S A, Mereu R, et al. Continuous glucose monitoring system in free-living healthy subjects: Results from a pilot study [J]. Diabetes Technology & Therapeutics, 2009, 11(3): 159–169.
Woredekal Y. Early detection and treatment of diabetic nephropathy [J]. Pediatric Endocrinology Reviews, 2008, 5(S4): 999–1004.
Zhou J, Li H, Ran X, et al. Reference values for continuous glucose monitoring in Chinese subjects [J]. Diabetes Care, 2009, 32(7): 1188–1193.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus [J]. Diabetes Care, 2003, 26(S1): 5–20.
Kidney Disease Outcome Quality Initiative. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification [J]. American Journal of Kidney Diseases, 2002, 39(S2): 1–266.
Mc Carter Rj, Hempe J M, Chalew S A. Mean blood glucose and biological variation have greater influence on HbAlc levels than glucose instability: An analysis of data from the diabetes control and complications trial [J]. Diabetes Care, 2006, 29(2): 352–355.
Del Prato S. In search of normoglycaemia in diabetes: controlling postprandial glucose [J]. International Journal of Obesity and Related Metabolic Disorders, 2002, 26(S3): 9–17.
Coutinho M, Gerstein H C, Wang Y, et al. The relationship between glucose and incident cardiovascular events: A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years [J]. Diabetes Care, 1999, 22(2): 233–240.
Weinzimer S A, DE Lucia M C, Boland E A, et al. Analysis of continuous glucose monitoring data from non-diabetic and diabetic children: A tale of two algorithms [J]. Diabetes Technology & Therapeutics, 2003, 5(3): 375–380.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Foundation item: the Shanghai United Developing Technology Project of Municipal Hospitals (No. SHDC12006101)
Rights and permissions
About this article
Cite this article
Wang, F., Cheng, Ds., Wang, Ns. et al. Continuous glucose monitoring in the patients with diabetic nephropathy. J. Shanghai Jiaotong Univ. (Sci.) 16, 508–512 (2011). https://doi.org/10.1007/s12204-011-1179-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12204-011-1179-3
Key words
- continuous glucose monitor
- diabetic nephropathy (DN)
- type-2 diabetes mellitus (DM-2)
- fluctuation of blood glucose