Abstract
Introduction
Skeletal muscle tissue development and regeneration relies on the proliferation, maturation and fusion of muscle progenitor cells (myoblasts), which arise transiently from muscle stem cells (satellite cells). Following muscle damage, myoblasts proliferate and differentiate in response to temporally-varying inflammatory cytokines, growth factors, and extracellular matrix cues, which stimulate a shared network of intracellular signaling pathways. Here we present an integrated data-modeling approach to elucidate synergies and antagonisms among proliferation and differentiation signaling axes in myoblasts stimulated by regeneration-associated ligands.
Methods
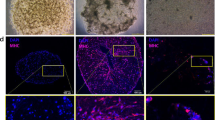
We treated mouse primary myoblasts in culture with combinations of eight regeneration-associated growth factors and cytokines in mixtures that induced additive, synergistic, and antagonistic effects on myoblast proliferation and differentiation responses. For these combinatorial stimuli, we measured the activation dynamics of seven signal transduction pathways using multiplexed phosphoprotein assays and scored proliferation and differentiation responses based on expression of myogenic commitment factors to assemble a cue-signaling-response data compendium. We interrogated the relationship between these signals and responses by partial least-squares (PLS) regression modeling.
Results
Partial least-squares data-modeling accurately predicted response outcomes in cross-validation on the training compendium (cumulative R 2 = 0.96). The PLS model highlighted signaling axes that distinctly govern myoblast proliferation (MEK–ERK, Stat3) and differentiation (JNK) in response to these combinatorial cues, and we confirmed these signal-response associations with small molecule perturbations. Unexpectedly, we observed that a negative feedback circuit involving the phosphatase DUSP6/MKP-3 auto-regulates MEK–ERK signaling in myoblasts.
Conclusion
This data-modeling approach identified conflicting signaling axes that underlie muscle progenitor cell proliferation and differentiation.






Similar content being viewed by others
Abbreviations
- AUC:
-
Area-under-the-curve
- CSR:
-
Cue-signal-response
- DUSP:
-
Dual specificity phosphatase
- EGF:
-
Epidermal growth factor
- FGF2:
-
Fibroblast growth factor 2
- IGF1:
-
Insulin-like growth factor 1
- IL-1α:
-
Interleukin-1α
- IL-6:
-
Interleukin-6
- LIF:
-
Leukemia inhibitor factor
- MHC:
-
Myosin heavy chain
- OSM:
-
Oncostatin-M
- PC:
-
Principal component
- PLS:
-
Partial-least squares
- TNF-α:
-
Tumor necrosis factor-α
References
Albeck, J. G., G. MacBeath, F. M. White, P. K. Sorger, D. A. Lauffenburger, and S. Gaudet. Collecting and organizing systematic sets of protein data. Nat. Rev. Mol. Cell Biol. 7(11):803–812, 2006.
Belizario, J. E., C. C. Fontes-Oliveira, J. P. Borges, J. A. Kashiabara, and E. Vannier. Skeletal muscle wasting and renewal: a pivotal role of myokine il-6. Springerplus 5:619, 2016.
Bennett, A. M., and N. K. Tonks. Regulation of distinct stages of skeletal muscle differentiation by mitogen-activated protein kinases. Science 278(5341):1288–1291, 1997.
Bernet, J. D., J. D. Doles, J. K. Hall, K. Kelly Tanaka, T. A. Carter, and B. B. Olwin. P38 mapk signaling underlies a cell-autonomous loss of stem cell self-renewal in skeletal muscle of aged mice. Nat. Med. 20(3):265–271, 2014.
Bliss, C. I. The toxicity of poisins applied jointly. Ann. Appl. Biol. 26(3):585–615, 1939.
Broholm, C., M. J. Laye, C. Brandt, R. Vadalasetty, H. Pilegaard, B. K. Pedersen, and C. Scheele. LIF is a contraction-induced myokine stimulating human myocyte proliferation. J. Appl. Physiol. (1985) 111(1):251–259, 2011.
Cheung, T. H., and T. A. Rando. Molecular regulation of stem cell quiescence. Nat. Rev. Mol. Cell Biol. 14(6):329–340, 2013.
Cosgrove, B. D., L. G. Alexopoulos, T. C. Hang, B. S. Hendriks, P. K. Sorger, L. G. Griffith, and D. A. Lauffenburger. Cytokine-associated drug toxicity in human hepatocytes is associated with signaling network dysregulation. Mol. BioSyst. 6(7):1195–1206, 2010.
Cosgrove, B. D., L. G. Alexopoulos, J. Saez-Rodriguez, L. G. Griffith, and D. A. Lauffenburger. A multipathway phosphoproteomic signaling network model of idiosyncratic drug- and inflammatory cytokine-induced toxicity in human hepatocytes. In: Conf Proc IEEE EMBS, 2009, pp. 5452–5455.
Cosgrove, B. D., P. M. Gilbert, E. Porpiglia, F. Mourkioti, S. P. Lee, S. Y. Corbel, M. E. Llewellyn, S. L. Delp, and H. M. Blau. Rejuvenation of the muscle stem cell population restores strength to injured aged muscles. Nat. Med. 20(3):255–264, 2014.
Cosgrove, B. D., L. G. Griffith, and D. A. Lauffenburger. Fusing tissue engineering and systems biology toward fulfilling their promise. Cell. Mol. Bioeng. 1(1):33–41, 2008.
Davies, S. P., H. Reddy, M. Caivano, and P. Cohen. Specificity and mechanism of action of some commonly used protein kinase inhibitors. Biochem. J. 351(Pt 1):95–105, 2000.
Deshpande, R. S., and A. A. Spector. Modeling stem cell myogenic differentiation. Sci. Rep. 7:40639, 2017.
Dumont, N. A., C. F. Bentzinger, M. C. Sincennes, and M. A. Rudnicki. Satellite cells and skeletal muscle regeneration. Compr. Physiol. 5(3):1027–1059, 2015.
Fedorov, Y. V., R. S. Rosenthal, and B. B. Olwin. Oncogenic ras-induced proliferation requires autocrine fibroblast growth factor 2 signaling in skeletal muscle cells. J. Cell Biol. 152(6):1301–1305, 2001.
Fu, X., J. Xiao, Y. Wei, S. Li, Y. Liu, J. Yin, K. Sun, H. Sun, H. Wang, Z. Zhang, B. T. Zhang, C. Sheng, H. Wang, and P. Hu. Combination of inflammation-related cytokines promotes long-term muscle stem cell expansion. Cell Res. 25(9):1082–1083, 2015.
Gaudet, S., K. A. Janes, J. G. Albeck, E. A. Pace, D. A. Lauffenburger, and P. K. Sorger. A compendium of signals and responses triggered by prodeath and prosurvival cytokines. Mol. Cell. Proteom. 4(10):1569–1590, 2005.
Heinemann, T., and A. Raue. Model calibration and uncertainty analysis in signaling networks. Curr. Opin. Biotechnol. 39:143–149, 2016.
Janes, K. A. An analysis of critical factors for quantitative immunoblotting. Sci. Signal. 8(371):rs2, 2015.
Janes, K. A., J. G. Albeck, S. Gaudet, P. K. Sorger, D. A. Lauffenburger, and M. B. Yaffe. A systems model of signaling identifies a molecular basis set for cytokine-induced apoptosis. Science 310(5754):1646–1653, 2005.
Janes, K. A., and M. B. Yaffe. Data-driven modelling of signal-transduction networks. Nat. Rev. Mol. Cell Biol. 7(11):820–828, 2006.
Joanisse, S., and G. Parise. Cytokine mediated control of muscle stem cell function. Adv. Exp. Med. Biol. 900:27–44, 2016.
Jones, N. C., Y. V. Fedorov, R. S. Rosenthal, and B. B. Olwin. Erk1/2 is required for myoblast proliferation but is dispensable for muscle gene expression and cell fusion. J. Cell. Physiol. 186(1):104–115, 2001.
Kellogg, R. A., and S. Tay. Noise facilitates transcriptional control under dynamic inputs. Cell 160(3):381–392, 2015.
Kemp, M. L., L. Wille, C. L. Lewis, L. B. Nicholson, and D. A. Lauffenburger. Quantitative network signal combinations downstream of tcr activation can predict il-2 production response. J. Immunol. 178(8):4984–4992, 2007.
Kreeger, P. K. Using partial least squares regression to analyze cellular response data. Sci. Signal. 6(271):tr7, 2013.
Kumar, N., A. Wolf-Yadlin, F. M. White, and D. A. Lauffenburger. Modeling her2 effects on cell behavior from mass spectrometry phosphotyrosine data. PLoS Comput. Biol. 3(1):e4, 2007.
Lagha, M., T. Sato, L. Bajard, P. Daubas, M. Esner, D. Montarras, F. Relaix, and M. Buckingham. Regulation of skeletal muscle stem cell behavior by pax3 and pax7. Cold Spring Harb. Symp. Quant. Biol. 73:307–315, 2008.
Lawlor, M. A., X. Feng, D. R. Everding, K. Sieger, C. E. Stewart, and P. Rotwein. Dual control of muscle cell survival by distinct growth factor-regulated signaling pathways. Mol. Cell. Biol. 20(9):3256–3265, 2000.
Miller-Jensen, K., K. A. Janes, J. S. Brugge, and D. A. Lauffenburger. Common effector processing mediates cell-specific responses to stimuli. Nature 448(7153):604–608, 2007.
Mueck, T., F. Berger, I. Buechsler, R. S. Valchanova, L. Landuzzi, P. L. Lollini, K. Klingel, and B. Munz. Traf6 regulates proliferation and differentiation of skeletal myoblasts. Differentiation 81(2):99–106, 2011.
Munoz-Canoves, P., C. Scheele, B. K. Pedersen, and A. L. Serrano. Interleukin-6 myokine signaling in skeletal muscle: a double-edged sword? FEBS J. 280:4131–4148, 2013.
Nagata, Y., K. Ohashi, E. Wada, Y. Yuasa, M. Shiozuka, Y. Nonomura, and R. Matsuda. Sphingosine-1-phosphate mediates epidermal growth factor-induced muscle satellite cell activation. Exp. Cell Res. 326(1):112–124, 2014.
Ogura, Y., S. M. Hindi, S. Sato, G. Xiong, S. Akira, and A. Kumar. TAK1 modulates satellite stem cell homeostasis and skeletal muscle repair. Nat. Commun. 6:10123, 2015.
Palacios, D., C. Mozzetta, S. Consalvi, G. Caretti, V. Saccone, V. Proserpio, V. E. Marquez, S. Valente, A. Mai, S. V. Forcales, V. Sartorelli, and P. L. Puri. TNF/p38alpha/polycomb signaling to pax7 locus in satellite cells links inflammation to the epigenetic control of muscle regeneration. Cell Stem Cell 7(4):455–469, 2010.
Patterson, K. I., T. Brummer, P. M. O’Brien, and R. J. Daly. Dual-specificity phosphatases: critical regulators with diverse cellular targets. Biochem. J. 418(3):475–489, 2009.
Pawlikowski, B., T. Orion Vogler, K. Gadek, and B. Olwin. Regulation of skeletal muscle stem cells by fibroblast growth factors. Dev. Dyn. 2017. doi:10.1002/dvdy.24495.
Price, F. D., J. von Maltzahn, C. F. Bentzinger, N. A. Dumont, H. Yin, N. C. Chang, D. H. Wilson, J. Frenette, and M. A. Rudnicki. Inhibition of JAK-STAT signaling stimulates adult satellite cell function. Nat. Med. 20(10):1174–1181, 2014.
Puri, P. L., and V. Sartorelli. Regulation of muscle regulatory factors by DNA-binding, interacting proteins, and post-transcriptional modifications. J. Cell. Physiol. 185(2):155–173, 2000.
Rando, T. A., and H. M. Blau. Primary mouse myoblast purification, characterization, and transplantation for cell-mediated gene therapy. J. Cell Biol. 125(6):1275–1287, 1994.
Rudnicki, M. A., F. Le Grand, I. McKinnell, and S. Kuang. The molecular regulation of muscle stem cell function. CSH Symp. Quant. Biol. 73:323–331, 2008.
Serra, C., D. Palacios, C. Mozzetta, S. V. Forcales, I. Morantte, M. Ripani, D. R. Jones, K. Du, U. S. Jhala, C. Simone, and P. L. Puri. Functional interdependence at the chromatin level between the MKK6/p38 and IGF1/PI3K/AKT pathways during muscle differentiation. Mol. Cell 28(2):200–213, 2007.
Tidball, J. G. Regulation of muscle growth and regeneration by the immune system. Nat. Rev. Immunol. 17(3):165–178, 2017.
Tierney, M. T., T. Aydogdu, D. Sala, B. Malecova, S. Gatto, P. L. Puri, L. Latella, and A. Sacco. Stat3 signaling controls satellite cell expansion and skeletal muscle repair. Nat. Med. 20(10):1182–1186, 2014.
Wales, S., S. Hashemi, A. Blais, and J. C. McDermott. Global MEF2 target gene analysis in cardiac and skeletal muscle reveals novel regulation of DUSP6 by p38MAPK-MEF2 signaling. Nucleic Acids Res. 42(18):11349–11362, 2014.
Xiao, F., H. Wang, X. Fu, Y. Li, K. Ma, L. Sun, X. Gao, and Z. Wu. Oncostatin m inhibits myoblast differentiation and regulates muscle regeneration. Cell Res. 21(2):350–364, 2011.
Yin, H., F. Price, and M. A. Rudnicki. Satellite cells and the muscle stem cell niche. Physiol. Rev. 93(1):23–67, 2013.
Acknowledgments
This work was financially supported by the National Institute on Aging of the National Institutes of Health under Award R00AG042491 (to B.D.C), a US Department of Education Graduate Assistantship in Areas of National Need under Award P200A150273 (to A.M.L), a Roberta G. and John B. DeVries Graduate Fellowship (to A.M.L.), and Hunter R. Rawlings III Cornell Presidential Research Scholarship (to R.F.K. and J.K.). This work made use of the Nanobiotechnology Center (NBTC) shared research facilities at Cornell University. The authors acknowledge technical assistance from Teresa Porri, Penny Burke, Andrea De Micheli, Hilarie Sit, Muhammad Safwan Jalal, Nancy Mejia, Isabella Mercado, Ryan Ausmus, and Paula Fraczek. The authors thank the anonymous reviewers for their constructive reviews.
Animal Studies
All institutional and national guidelines for the care and use of laboratory animals were followed in a protocol approved by Cornell University’s Institutional Animal Care and Use Committee (IACUC).
Conflicts of interest
A. M. Loiben, S. Soueld-Baumgarten, D. Bhattacharya, R. F. Kopyto, J. C. Kim and B. D. Cosgrove declare that they have no conflicts of interest.
Human Studies
No human studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Richard Waugh oversaw the review of this article.
Benjamin D. Cosgrove
is an Assistant Professor in the Meinig School of Biomedical Engineering at Cornell University in Ithaca, NY, where he directs the Laboratory of Regenerative Systems Biology. His research group, which is currently supported by a NIH R00 Pathway-to-Independence Award, develops and implements systems biology and biomaterials engineering approaches to study how cell–cell communication and intracellular signaling networks regulate stem and progenitor cell function in skeletal muscle homeostasis and regeneration, and how these processes become dysfunctional in aging and muscular dystrophies. Dr. Cosgrove earned a Bachelor’s in Biomedical Engineering at the University of Minnesota and a Ph.D. in Bioengineering at the Massachusetts Institute of Technology. His Ph.D. thesis research, under the joint supervision of Dr. Douglas Lauffenburger and Dr. Linda Griffith, which established on experimental and computational systems biology tools to elucidate signaling network mechanisms regulating liver hepatocyte cell-fate decisions, was supported by a Whitaker Foundation Graduate Research Fellowship and a Biomedical Engineering Society Graduate Research Award. His postdoctoral research with Dr. Helen Blau at Stanford University was supported by a Stanford Molecular Imaging Scholars Fellowship and NIH K99 Pathway-to-Independence Award and was recognized by the Cellular and Molecular Bioengineering Special Interest Group of the Biomedical Engineering Society with a Rising Star award in 2015.

This article is part of the 2017 CMBE Young Innovators special issue.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Loiben, A.M., Soueid-Baumgarten, S., Kopyto, R.F. et al. Data-Modeling Identifies Conflicting Signaling Axes Governing Myoblast Proliferation and Differentiation Responses to Diverse Ligand Stimuli. Cel. Mol. Bioeng. 10, 433–450 (2017). https://doi.org/10.1007/s12195-017-0508-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12195-017-0508-5