Abstract
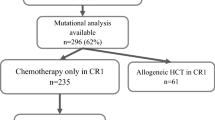
Mutation status of FLT3, NPM1, and CEBPA is used to classify the prognosis of acute myeloid leukemia, but its significance in patients with cytogenetically normal (CN) AML is unclear. We prospectively analyzed these genes in 295 patients with CN-AML and identified 76 (25.8%) FLT3-ITD, 113 (38.3%) NPM1 mutations, and 30 (10.2%) CEBPA biallelic mutations. We found that patients with FLT3-ITD had a poor prognosis at any age, while patients with CEBPA biallelic mutation were younger and had a better prognosis. FLT3-ITD and NPM1 mutations were correlated, and the favorable prognostic impact of being FLT3-ITD negative and NPM1 mutation positive was evident only in patients aged 65 years or more. For CEBPA, 86.7% of the patients with biallelic mutation and 9.1% of patients with the single allele mutation had in-frame mutations in the bZIP domain, which were strongly associated with a favorable prognosis. Multivariate analysis showed that age < 65 years, FLT3-ITD and CEBPA bZIP in-frame mutation were independent prognostic factors. The results suggest that analyzing these gene mutations at diagnosis can inform selection of the optimal intensity of therapy for patients with CN-AML.






Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
O’Donnell MR, Abboud CN, Altman J, Appelbaum FR, Arber DA, Attar E, et al. NCCN clinical practice guidelines acute myeloid leukemia. J Natl Compr Canc Netw. 2012;10(8):984–1021. https://doi.org/10.6004/jnccn.2012.0103.
O’Donnell MR, Tallman MS, Abboud CN, Altman JK, Appelbaum FR, Arber DA, et al. Acute Myeloid Leukemia, Version 3.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15(7):926–57. https://doi.org/10.6004/jnccn.2017.0116.
Tallman MS, Wang ES, Altman JK, Appelbaum FR, Bhatt VR, Bixby D, et al. Acute Myeloid Leukemia, Version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(6):721–49. https://doi.org/10.6004/jnccn.2019.0028.
Pollyea DA, Bixby D, Perl A, Bhatt VR, Altman JK, Appelbaum FR, et al. NCCN guidelines insights: acute myeloid leukemia, version 2.2021. J Natl Compr Canc Netw. 2021;19(1):16–27. https://doi.org/10.6004/jnccn.2021.0002.
Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115(3):453–74. https://doi.org/10.1182/blood-2009-07-235358.
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47. https://doi.org/10.1182/blood-2016-08-733196.
Dohner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, et al. Diagnosis and management of AML in adults: 2022 ELN recommendations from an international expert panel. Blood. 2022. https://doi.org/10.1182/blood.2022016867.
Wouters BJ, Lowenberg B, Erpelinck-Verschueren CA, van Putten WL, Valk PJ, Delwel R. Double CEBPA mutations, but not single CEBPA mutations, define a subgroup of acute myeloid leukemia with a distinctive gene expression profile that is uniquely associated with a favorable outcome. Blood. 2009;113(13):3088–91. https://doi.org/10.1182/blood-2008-09-179895.
Wakita S, Sakaguchi M, Oh I, Kako S, Toya T, Najima Y, et al. Prognostic impact of CEBPA bZIP domain mutation in acute myeloid leukemia. Blood Adv. 2022;6(1):238–47. https://doi.org/10.1182/bloodadvances.2021004292.
Taube F, Georgi JA, Kramer M, Stasik S, Middeke JM, Rollig C, et al. CEBPA mutations in 4708 patients with acute myeloid leukemia: differential impact of bZIP and TAD mutations on outcome. Blood. 2022;139(1):87–103. https://doi.org/10.1182/blood.2020009680.
Hou HA, Chou WC, Kuo YY, Liu CY, Lin LI, Tseng MH, et al. TP53 mutations in de novo acute myeloid leukemia patients: longitudinal follow-ups show the mutation is stable during disease evolution. Blood Cancer J. 2015;5: e331. https://doi.org/10.1038/bcj.2015.59.
Niparuck P, Police P, Noikongdee P, Siriputtanapong K, Limsuwanachot N, Rerkamnuaychoke B, et al. TP53 mutation in newly diagnosed acute myeloid leukemia and myelodysplastic syndrome. Diagn Pathol. 2021;16(1):100. https://doi.org/10.1186/s13000-021-01162-8.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transpl. 2013;48(3):452–8. https://doi.org/10.1038/bmt.2012.244.
Dufour A, Schneider F, Metzeler KH, Hoster E, Schneider S, Zellmeier E, et al. Acute myeloid leukemia with biallelic CEBPA gene mutations and normal karyotype represents a distinct genetic entity associated with a favorable clinical outcome. J Clin Oncol. 2010;28(4):570–7. https://doi.org/10.1200/JCO.2008.21.6010.
Arthur DC, Berger R, Golomb HM, Swansbury GJ, Reeves BR, Alimena G, et al. The clinical significance of karyotype in acute myelogenous leukemia. Cancer Genet Cytogenet. 1989;40(2):203–16. https://doi.org/10.1016/0165-4608(89)90025-3.
Machnicki JL, Bloomfield CD. Chromosomal abnormalities in myelodysplastic syndromes and acute myeloid leukemia. Clin Lab Med. 1990;10(4):755–67.
Mrozek K, Heinonen K, de la Chapelle A, Bloomfield CD. Clinical significance of cytogenetics in acute myeloid leukemia. Semin Oncol. 1997;24(1):17–31.
Nimer SD. Is it important to decipher the heterogeneity of “normal karyotype AML”? Best Pract Res Clin Haematol. 2008;21(1):43–52. https://doi.org/10.1016/j.beha.2007.11.010.
Schlenk RF, Dohner K, Krauter J, Frohling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358(18):1909–18. https://doi.org/10.1056/NEJMoa074306.
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML 10 trial. The medical research council adult and children’s leukaemia working parties. Blood. 1998;92(7):2322–33.
Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia group B (CALGB 8461). Blood. 2002;100(13):4325–36. https://doi.org/10.1182/blood-2002-03-0772.
Harada Y, Nagata Y, Kihara R, Ishikawa Y, Asou N, Ohtake S, et al. Prognostic analysis according to the 2017 ELN risk stratification by genetics in adult acute myeloid leukemia patients treated in the Japan adult leukemia study group (JALSG) AML201 study. Leuk Res. 2018;66:20–7. https://doi.org/10.1016/j.leukres.2018.01.008.
Sakaguchi M, Yamaguchi H, Najima Y, Usuki K, Ueki T, Oh I, et al. Prognostic impact of low allelic ratio FLT3-ITD and NPM1 mutation in acute myeloid leukemia. Blood Adv. 2018;2(20):2744–54. https://doi.org/10.1182/bloodadvances.2018020305.
Tong WG, Sandhu VK, Wood BL, Hendrie PC, Becker PS, Pagel JM, et al. Correlation between peripheral blood and bone marrow regarding FLT3-ITD and NPM1 mutational status in patients with acute myeloid leukemia. Haematologica. 2015;100(3):e97–8. https://doi.org/10.3324/haematol.2014.118422.
Boonthimat C, Thongnoppakhun W, Auewarakul CU. Nucleophosmin mutation in Southeast Asian acute myeloid leukemia: eight novel variants, FLT3 coexistence and prognostic impact of NPM1/FLT3 mutations. Haematologica. 2008;93(10):1565–9. https://doi.org/10.3324/haematol.12937.
Hollink IH, Zwaan CM, Zimmermann M, Arentsen-Peters TC, Pieters R, Cloos J, et al. Favorable prognostic impact of NPM1 gene mutations in childhood acute myeloid leukemia, with emphasis on cytogenetically normal AML. Leukemia. 2009;23(2):262–70. https://doi.org/10.1038/leu.2008.313.
Becker H, Marcucci G, Maharry K, Radmacher MD, Mrozek K, Margeson D, et al. Favorable prognostic impact of NPM1 mutations in older patients with cytogenetically normal de novo acute myeloid leukemia and associated gene- and microRNA-expression signatures: a cancer and leukemia group B study. J Clin Oncol. 2010;28(4):596–604. https://doi.org/10.1200/JCO.2009.25.1496.
Heath EM, Chan SM, Minden MD, Murphy T, Shlush LI, Schimmer AD. Biological and clinical consequences of NPM1 mutations in AML. Leukemia. 2017;31(4):798–807. https://doi.org/10.1038/leu.2017.30.
Shamaa S, Laimon N, Aladle DA, Azmy E, Elghannam DM, Salem DA, et al. Prognostic implications of NPM1 mutations and FLT3 internal tandem duplications in Egyptian patients with cytogenetically normal acute myeloid leukemia. Hematology. 2014;19(1):22–30. https://doi.org/10.1179/1607845413Y.0000000085.
Dohner K, Schlenk RF, Habdank M, Scholl C, Rucker FG, Corbacioglu A, et al. Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood. 2005;106(12):3740–6. https://doi.org/10.1182/blood-2005-05-2164.
Juliusson G, Jadersten M, Deneberg S, Lehmann S, Mollgard L, Wennstrom L, et al. The prognostic impact of FLT3-ITD and NPM1 mutation in adult AML is age-dependent in the population-based setting. Blood Adv. 2020;4(6):1094–101. https://doi.org/10.1182/bloodadvances.2019001335.
Park DJ, Kwon A, Cho BS, Kim HJ, Hwang KA, Kim M, et al. Characteristics of DNMT3A mutations in acute myeloid leukemia. Blood Res. 2020;55(1):17–26. https://doi.org/10.5045/br.2020.55.1.17.
Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36(7):1703–19. https://doi.org/10.1038/s41375-022-01613-1.
Akabari R, Qin D, Hussaini M. Technological advances: CEBPA and FLT3 internal tandem duplication mutations can be reliably detected by next generation sequencing. Genes (Basel). 2022;13(4):630. https://doi.org/10.3390/genes13040630.
Kato N, Kitaura J, Doki N, Komeno Y, Watanabe-Okochi N, Togami K, et al. Two types of C/EBPalpha mutations play distinct but collaborative roles in leukemogenesis: lessons from clinical data and BMT models. Blood. 2011;117(1):221–33. https://doi.org/10.1182/blood-2010-02-270181.
Schmidt L, Heyes E, Grebien F. Gain-of-function effects of N-terminal CEBPA mutations in acute myeloid leukemia. BioEssays. 2020;42(2): e1900178. https://doi.org/10.1002/bies.201900178.
Pabst T, Mueller BU, Zhang P, Radomska HS, Narravula S, Schnittger S, et al. Dominant-negative mutations of CEBPA, encoding CCAAT/enhancer binding protein-alpha (C/EBPalpha), in acute myeloid leukemia. Nat Genet. 2001;27(3):263–70. https://doi.org/10.1038/85820.
Gombart AF, Hofmann WK, Kawano S, Takeuchi S, Krug U, Kwok SH, et al. Mutations in the gene encoding the transcription factor CCAAT/enhancer binding protein alpha in myelodysplastic syndromes and acute myeloid leukemias. Blood. 2002;99(4):1332–40. https://doi.org/10.1182/blood.v99.4.1332.
Mannelli F, Ponziani V, Bencini S, Bonetti MI, Benelli M, Cutini I, et al. CEBPA-double-mutated acute myeloid leukemia displays a unique phenotypic profile: a reliable screening method and insight into biological features. Haematologica. 2017;102(3):529–40. https://doi.org/10.3324/haematol.2016.151910.
Green CL, Koo KK, Hills RK, Burnett AK, Linch DC, Gale RE. Prognostic significance of CEBPA mutations in a large cohort of younger adult patients with acute myeloid leukemia: impact of double CEBPA mutations and the interaction with FLT3 and NPM1 mutations. J Clin Oncol. 2010;28(16):2739–47. https://doi.org/10.1200/JCO.2009.26.2501.
Pabst T, Eyholzer M, Haefliger S, Schardt J, Mueller BU. Somatic CEBPA mutations are a frequent second event in families with germline CEBPA mutations and familial acute myeloid leukemia. J Clin Oncol. 2008;26(31):5088–93. https://doi.org/10.1200/JCO.2008.16.5563.
Acknowledgements
We thank all physicians for their contributions to this study and their dedicated care of the patients. We thank Satoshi Oguri and Kaori Sato for FLT3-ITD analysis. We thank Chiaki Yokoyama and Fumina Kusaka for management of patients’ samples and data integrity.
Funding
This work was supported by North Japan Hematology Study Group (NJHSG) and partly by Japan Society for the Promotion of Science KAKENHI, Grant-in-Aid for scientific research (20K08745 [M.O.]).
Author information
Authors and Affiliations
Contributions
N.M. and M.O. designed the study, analyzed the data and wrote the manuscript; N.M., S.Yoshida, H.K., S.T., S.Yokoyama, and S.F. performed the molecular analysis; T.M., S.H., M.A., S.O., Y.K., Y.T., S.Y., T.M., T.N., M.I., H.K., Y.H., K.F., T.I., H.S., T.K. contributed to the data collection and provided critique to the manuscript; T.T. revised and approved the manuscript; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Miyashita, N., Onozawa, M., Yoshida, S. et al. Prognostic impact of FLT3-ITD, NPM1 mutation and CEBPA bZIP domain mutation in cytogenetically normal acute myeloid leukemia: a Hokkaido Leukemia Net study. Int J Hematol 118, 36–46 (2023). https://doi.org/10.1007/s12185-023-03567-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-023-03567-1