Abstract
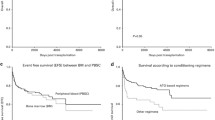
Although bone marrow transplantation is the recommended form of allogeneic hematopoietic stem cell transplantation for aplastic anemia, some patients undergo peripheral blood stem cell transplantation (PBSCT). Therefore, there is critical demand to identify factors affecting transplantation outcomes. Using the Japanese registry database, we retrospectively analyzed outcomes of 94 adult patients with aplastic anemia who underwent PBSCT from HLA-identical sibling donors. The cumulative incidence of neutrophil engraftment was 94% (95% confidence interval [CI] 86–97%), and was significantly higher in patients who received anti-thymocyte globulin (ATG) in conditioning. The cumulative incidence rate was 26% (95% CI 17–35%) in grades II–IV acute graft-versus-host disease (GVHD) and 20% (95% CI 13–29%) in extensive chronic GVHD, and tended to be lower in patients with chronic GVHD who received ATG-based conditioning. The 5-year overall survival (OS) rate was 70% (95% CI 59–78%). In multivariate analysis, patient age < 40 years, shorter period from diagnosis to transplantation, better performance status, and ATG-based conditioning were significantly correlated with favorable OS. In conclusion, PBSCT from HLA-identical sibling donors for aplastic anemia would result in acceptable outcomes. Several risk factors identified in our study should be considered when selecting a stem cell source.



Similar content being viewed by others
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Killick SB, Bown N, Cavenagh J, Dokal I, Foukaneli T, Hill A, et al. Guidelines for the diagnosis and management of adult aplastic anaemia. Br J Haematol. 2016;172:187–207.
de Latour RP. Transplantation for bone marrow failure: current issues. Hematol Am Soc Hematol Educ Program. 2016;2016:90–8.
Bacigalupo A. How I treat acquired aplastic anemia. Blood. 2017;129:1428–36.
Iftikhar R, Chaudhry QUN, Anwer F, Neupane K, Rafae A, Mahmood SK, et al. Allogeneic hematopoietic stem cell transplantation in aplastic anemia: current indications and transplant strategies. Blood Rev. 2021;47: 100772.
Yoshimi A, Baldomero H, Horowitz M, Szer J, Niederwieser D, Gratwohl A, et al. Global use of peripheral blood vs bone marrow as source of stem cells for allogeneic transplantation in patients with bone marrow failure. JAMA. 2016;315:198–200.
Schrezenmeier H, Passweg JR, Marsh JC, Bacigalupo A, Bredeson CN, Bullorsky E, et al. Worse outcome and more chronic GVHD with peripheral blood progenitor cells than bone marrow in HLA-matched sibling donor transplants for young patients with severe acquired aplastic anemia. Blood. 2007;110:1397–400.
Chu R, Brazauskas R, Kan F, Bashey A, Bredeson C, Camitta B, et al. Comparison of outcomes after transplantation of G-CSF-stimulated bone marrow grafts versus bone marrow or peripheral blood grafts from HLA-matched sibling donors for patients with severe aplastic anemia. Biol Blood Marrow Transplant. 2011;17:1018–24.
Bacigalupo A, Socié G, Schrezenmeier H, Tichelli A, Locasciulli A, Fuehrer M, et al. Bone marrow versus peripheral blood as the stem cell source for sibling transplants in acquired aplastic anemia: survival advantage for bone marrow in all age groups. Haematologica. 2012;97:1142–8.
Kumar R, Kimura F, Ahn KW, Hu ZH, Kuwatsuka Y, Klein JP, et al. Comparing outcomes with bone marrow or peripheral blood stem cells as graft source for matched sibling transplants in severe aplastic anemia across different economic regions. Biol Blood Marrow Transplant. 2016;22:932–40.
Gupta V, Eapen M, Brazauskas R, Carreras J, Aljurf M, Gale RP, et al. Impact of age on outcomes after bone marrow transplantation for acquired aplastic anemia using HLA-matched sibling donors. Haematologica. 2010;95:2119–25.
Deeg HJ, Self S, Storb R, Doney K, Appelbaum FR, Witherspoon RP, et al. Decreased incidence of marrow graft rejection in patients with severe aplastic anemia: changing impact of risk factors. Blood. 1986;68:1363–8.
Atsuta Y. Introduction of transplant registry unified management program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15:825–8.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204–17.
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Onishi Y, Mori T, Yamazaki H, Takenaka K, Yamaguchi H, Shingai N, et al. Cyclosporine/methotrexate versus tacrolimus/methotrexate with or without anti-thymocyte globulin as GVHD prophylaxis in adult patients with aplastic anemia. Ann Hematol. 2021;100:217–28.
Ghavamzadeh A, Alimoghaddam K, Jalili M, Mousavi SA, Bahar B, Kasaeian A, et al. Peripheral blood versus bone marrow transplant in patients with aplastic anemia, an unresolved issue. Bone Marrow Transplant. 2016;51:1628–30.
Eapen M, Le Rademacher J, Antin JH, Champlin RE, Carreras J, Fay J, et al. Effect of stem cell source on outcomes after unrelated donor transplantation in severe aplastic anemia. Blood. 2011;118:2618–21.
Bacigalupo A, Socié G, Hamladji RM, Aljurf M, Maschan A, Kyrcz-Krzemien S, et al. Current outcome of HLA identical sibling versus unrelated donor transplants in severe aplastic anemia: an EBMT analysis. Haematologica. 2015;100:696–702.
Champlin RE, Perez WS, Passweg JR, Klein JP, Camitta BM, Gluckman E, et al. Bone marrow transplantation for severe aplastic anemia: a randomized controlled study of conditioning regimens. Blood. 2007;109:4582–5.
Kako S, Yamazaki H, Ohashi K, Ozawa Y, Ota S, Kanda Y, et al. Mixed chimerism and secondary graft failure in allogeneic hematopoietic stem cell transplantation for aplastic anemia. Biol Blood Marrow Transplant. 2020;26:445–50.
Clé DV, Atta EH, Dias DS, Lima CB, Bonduel M, Sciuccati G, et al. Repeat course of rabbit antithymocyte globulin as salvage following initial therapy with rabbit antithymocyte globulin in acquired aplastic anemia. Haematologica. 2015;100:e345–7.
Devillier R, Crocchiolo R, Castagna L, Fürst S, El Cheikh J, Faucher C, et al. The increase from 2.5 to 5 mg/kg of rabbit anti-thymocyte-globulin dose in reduced intensity conditioning reduces acute and chronic GVHD for patients with myeloid malignancies undergoing allo-SCT. Bone Marrow Transplant. 2012;47:639–45.
Butera S, Cerrano M, Brunello L, Dellacasa CM, Faraci DG, Vassallo S, et al. Impact of anti-thymocyte globulin dose for graft-versus-host disease prophylaxis in allogeneic hematopoietic cell transplantation from matched unrelated donors: a multicenter experience. Ann Hematol. 2021;100:1837–47.
Zelikson V, Simmons G, Raman N, Krieger E, Rebiero A, Hawks K, et al. Dynamical systems modeling of early-term immune reconstitution with different antithymocyte globulin administration schedules in allogeneic stem cell transplantation. Transplant Cell Ther. 2022;28:85.e1-85.e9.
Acknowledgements
The authors would like to thank all the physicians and data managers at each transplantation center and the staff members at the Japanese Data Center for Hematopoietic Cell Transplantation.
Funding
Takehiko Mori received research funding from Mochida Pharmaceutical; MSD K.K.; Novartis Pharma K.K.; Eisai Pharmaceuticals; Medical & Biological Laboratories; Otsuka Pharmaceutical; Kyowa Kirin Co. Ltd.; Shionogi & Co.; Chugai Pharmaceutical; Takeda Pharmaceutical; Asahi Kasei Corporation; Bristol Myers Squibb; AbbVie GK; CSL Behring; Teijin Pharma; and KM Biologics, outside the submitted work. The remaining authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
YN, TM, SK, HY and YO: designed the study. YN: analyzed the data and wrote the manuscript. All the authors have discussed the results and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Takehiko Mori has received personal fees from Pfizer Inc.; MSD K.K.; Janssen Pharma; Sumitomo Pharma; Novartis Pharma K.K.; Kyowa Kirin Co. Ltd.; Chugai Pharmaceutical; Asahi Kasei Corporation; Japan Blood Products Organization; Takeda Pharmaceutical; Ono Pharmaceutical; Eisai Pharmaceuticals; Astellas Pharma; AbbVie GK; Meiji Seika Pharma; CSL Behring; SymBio Pharmaceuticals; AstraZeneca; Daiichi Sankyo; Mochida Pharmaceutical; Sanofi, Otsuka Pharmaceutical; and Mitsubishi Tanabe Pharma, outside the submitted work. Hirohito Yamazaki has received personal fees from Novartis Pharma K.K. and Kyowa Kirin Co. Ltd., outside the submitted work. The remaining authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakamura, Y., Mori, T., Kako, S. et al. Outcome of peripheral blood stem cell transplantation from HLA-identical sibling donors for adult patients with aplastic anemia. Int J Hematol 117, 356–365 (2023). https://doi.org/10.1007/s12185-022-03487-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03487-6