Abstract
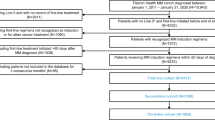
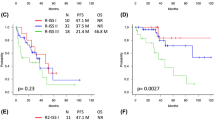
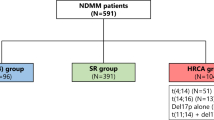
Optimal treatments for multiple myeloma (MM) patients with high-risk cytogenetics must be determined, but subgroup features are not well-defined. We used real-world data from the Korean Myeloma Registry (KMR) to analyze the characteristics and clinical outcomes of newly diagnosed MM patients with ≥ 1 high-risk cytogenetic abnormality: Group 1: t(4;14) or t(14;16); Group 2: del(17p); Group 3: t(4;14)/del(17p) or t(14;16)/del(17p). Overall, 347 high-risk patients were identified (males, 48.7%; median age, 63 years). Median progression-free survival (PFS) and overall survival (OS) were 19.0 months (95% CI 17.0–20.0) and 50.0 months (95% CI 37.0–61.0), respectively. PFS (p = 0.047) and OS (p = 0.020) differed significantly between groups. After stratification by transplant eligibility, PFS and OS were significantly poorer in Group 3 among transplant-eligible patients, and even poorer in those with gain(1q). Patients stratified by cytogenetic abnormality and revised International Staging System (R-ISS) had significantly different PFS (p < 0.001) and OS (p = 0.003), with the worst survival in R-ISS III/Group 3 (median OS 21.0 months). Higher number of high-risk cytogenetic abnormalities was a negative prognostic marker for PFS and OS (p < 0.001). Real-world KMR data showed that risk factors for poor prognosis of MM patients included del(17p), R-ISS stage, and number of cytogenetic abnormalities.





Similar content being viewed by others
Availability of data and material
All relevant data are within the manuscript and its Supporting Information files.
Code availability
Not applicable.
References
Anderson KC, Carrasco RD. Pathogenesis of myeloma. Annu Rev Pathol. 2011;6:249–74.
Kuehl WM, Bergsagel PL. Molecular pathogenesis of multiple myeloma and its premalignant precursor. J Clin Invest. 2012;122:3456–63.
Bloedjes TA, de Wilde G, Guikema JEJ. Metabolic effects of recurrent genetic aberrations in multiple myeloma. Cancers (Basel). 2021;13:396.
Kumar SK, Dispenzieri A, Lacy MQ, Gertz MA, Buadi FK, Pandey S, et al. Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Leukemia. 2014;28:1122–8.
Ziogas DC, Dimopoulos MA, Kastritis E. Prognostic factors for multiple myeloma in the era of novel therapies. Expert Rev Hematol. 2018;11:863–79.
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, et al. Revised international staging system for multiple myeloma: a report from international myeloma working group. J Clin Oncol. 2015;33:2863–9.
Binder M, Rajkumar SV, Ketterling RP, Greipp PT, Dispenzieri A, Lacy MQ, et al. Prognostic implications of abnormalities of chromosome 13 and the presence of multiple cytogenetic high-risk abnormalities in newly diagnosed multiple myeloma. Blood Cancer J. 2017;7:e600.
Shah V, Sherborne AL, Walker BA, Johnson DC, Boyle EM, Ellis S, et al. Prediction of outcome in newly diagnosed myeloma: a meta-analysis of the molecular profiles of 1905 trial patients. Leukemia. 2018;32:102–10.
Hong J, Lee JH. Recent advances in multiple myeloma: a Korean perspective. Korean J Intern Med. 2016;31:820–34.
Yoo SL, Kim DJ, Lee SM, Kang WG, Kim SY, Lee JH, et al. Improving patient access to new drugs in South Korea: evaluation of the national drug formulary system. Int J Environ Res Public Health. 2019;16:288.
Kim SJ, Kim K, Kim BS, Jo DY, Kang HJ, Kim JS, et al. Clinical features and survival outcomes in patients with multiple myeloma: analysis of web-based data from the Korean Myeloma Registry. Acta Haematol. 2009;122:200–10.
Lee JH, Lee DS, Lee JJ, Chang YH, Jin JY, Jo DY, et al. Multiple myeloma in Korea: past, present and future perspectives. Experience of the Korean Multiple Myeloma Working Party. Int J Hematol. 2010;92:52–7.
Song MK, Chung JS, Lee JJ, Lee JH, Song IC, Lee SM, et al. Risk stratification model in elderly patients with multiple myeloma: clinical role of magnetic resonance imaging combined with international staging system and cytogenetic abnormalities. Acta Haematol. 2015;134:7–16.
Oh S, Koo DH, Kwon MJ, Kim K, Suh C, Min CK, et al. Chromosome 13 deletion and hypodiploidy on conventional cytogenetics are robust prognostic factors in Korean multiple myeloma patients: web-based multicenter registry study. Ann Hematol. 2014;93:1353–61.
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15:e538–48.
Jung HA, Jang MA, Kim K, Kim SH. Clinical utility of a diagnostic approach to detect genetic abnormalities in multiple myeloma: a single institution experience. Ann Lab Med. 2018;38:196–203.
Byun JM, Shin DY, Hong J, Kim I, Kim HK, Lee DS, et al. Distinct predictive impact of FISH abnormality in proteasome inhibitors and immunomodulatory agents response: redefining high-risk multiple myeloma in Asian patients. Cancer Med. 2018;7:831–41.
Lancman G, et al. The effect of novel therapies in high-molecular-risk multiple myeloma. Clin Adv Hematol Oncol H&O. 2017;15:870.
Lonial S, Dimopoulos M, Palumbo A, et al. ELOQUENT-2 Investigators. Elotuzumab therapy for relapsed or refractory multiple myeloma. N Engl J Med. 2015;373(7):621–31.
Sonneveld P, Avet-Loiseau H, Lonial S, Usmani S, Siegel D, Anderson KC, et al. Treatment of multiple myeloma with high-risk cytogenetics: a consensus of the International Myeloma Working Group. Blood. 2016;127:2955–62.
Schmidt TM, Barwick BG, Joseph N, Heffner LT, Hofmeister CC, Bernal L, et al. Gain of Chromosome 1q is associated with early progression in multiple myeloma patients treated with lenalidomide, bortezomib, and dexamethasone. Blood Cancer J. 2019;9:94.
Hanamura I, Stewart JP, Huang Y, Zhan F, Santra M, Sawyer JR, et al. Frequent gain of chromosome band 1q21 in plasma-cell dyscrasias detected by fluorescence in situ hybridization: incidence increases from MGUS to relapsed myeloma and is related to prognosis and disease progression following tandem stem-cell transplantation. Blood. 2006;108:1724–32.
Jian Y, Chen X, Zhou H, Zhu W, Liu N, Geng C, et al. Prognostic impact of cytogenetic abnormalities in multiple myeloma: a retrospective analysis of 229 patients. Medicine (Baltimore). 2016;95:e3521.
Castaneda O, Baz R. Multiple myeloma genomics—a concise review. Acta Med Acad. 2019;48:57–67.
Fakhri B, Vij R. Clonal evolution in multiple myeloma. Clin Lymphoma Myeloma Leuk. 2016;16(Suppl):S130–4.
Lakshman A, Painuly U, Rajkumar SV, Ketterling RP, Kapoor P, Greipp PT, et al. Natural history of multiple myeloma with de novo del(17p). Blood Cancer J. 2019;9:32.
Radocha J, Maisnar V, Pour L, Špička I, Minařík J, Szeligová L, et al. Validation of multiple myeloma risk stratification indices in routine clinical practice: analysis of data from the Czech Myeloma Group Registry of Monoclonal Gammopathies. Cancer Med. 2018;7:4132–45.
Cavo M, Tacchetti P, Patriarca F, Petrucci MT, Pantani L, Galli M, et al. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet. 2010;376:2075–85.
Cavo M, Pantani L, Pezzi A, Petrucci MT, Patriarca F, Di Raimondo F, et al. Bortezomib-thalidomide-dexamethasone (VTD) is superior to bortezomib-cyclophosphamide-dexamethasone (VCD) as induction therapy prior to autologous stem cell transplantation in multiple myeloma. Leukemia. 2015;29:2429–31.
Abdallah N, Rajkumar SV, Greipp P, Kapoor P, Gertz MA, Dispenzieri A, et al. Cytogenetic abnormalities in multiple myeloma: association with disease characteristics and treatment response. Blood Cancer J. 2020;10:82.
Larocca A, Mina R, Offidani M, Liberati AM, Ledda A, Patriarca F, Evangelista A, Spada S, Benevolo G, Oddolo D, Innao V, Cangiolosi C, Bernardini A, Musto P, Amico V, Fraticelli V, Paris L, Giuliani N, Falcone AP, Zambello R, De Paoli L, Romano A, Palumbo A, Montefusco V, Hájek R, Boccadoro M, Bringhen S. First-line therapy with either bortezomib-melphalan-prednisone or lenalidomide-dexamethasone followed by lenalidomide for transplant-ineligible multiple myeloma patients: a pooled analysis of two randomized trials. Haematologica. 2020;105(4):1074–80.
Sonneveld P, Avet-Loiseau H, Lonial S. Treatment of multiple myeloma with high-risk cytogenetics: a consensus of the International Myeloma Working Group. Blood. 2016;127(24):2955–62.
Yuan YY, Zhu HY, Wu JZ, Xia Y, Liang JH, Wu W, et al. The percentage of cells with 17p deletion and the size of 17p deletion subclones show prognostic significance in chronic lymphocytic leukemia. Genes Chromosomes Cancer. 2019;58:43–51.
Acknowledgements
Under the direction of the authors, medical writing assistance was provided by Robert A. Furlong PhD and David P. Figgitt PhD, ISMPP CMPP™, Content Ed Net, with funding from Amgen Korea.
Funding
This study was funded by Amgen Korea.
Author information
Authors and Affiliations
Consortia
Contributions
KK conceived and designed the analysis, contributed to data collection, and wrote the paper. JSK, S-SY, DHY, H-SE, J-JL and C-KM contributed to data collection and reviewing the manuscript. HWY and MP contributed to analyzing the data, writing the statistical analysis, and reviewing the manuscript. HL performed the statistical analysis and wrote the paper. Patient information was provided by various investigators at KMMWP. All authors were involved in the preparation of the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Kihyun Kim, Jin Seok Kim, Sung-Soo Yoon, Dok Hyun Yoon, Hyeon-Seok Eom, Je-Jung Lee, Hyeon Woo Yim, Misun Park and Chang-Ki Min report consultancy and research funding from Amgen Korea. Hojoon Lee reports employment by Amgen Korea.
Ethical approval
This study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (IRB no. SMC2018-08-058-001), the Catholic University of Korea (IRB no. KC18RODI0556), Severance Hospital (IRB no. 4-2018-0633), Seoul National University Hospital (IRB no. H-1810-111-982), Asan Medical Center (IRB no. 2019-0788), National Cancer Center of Korea (IRB no. NCC2019-0105), and Chonnam National University Hwasun Hospital (IRB no. CNUHH-2019-092).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kim, K., Kim, J.S., Yoon, SS. et al. Characteristics and clinical outcome of high-risk multiple myeloma patients in Korea (KMM 1805). Int J Hematol 116, 110–121 (2022). https://doi.org/10.1007/s12185-022-03332-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03332-w