Abstract
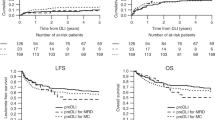
To explore the efficacy and safety of G-SCF-mobilized donor lymphocyte infusion (DLI) for treatment of relapse of hematologic malignancies after allogeneic peripheral blood stem cell transplantation, we performed a retrospective analysis in a cohort of patients with morphologic (n = 36) or molecular (n = 22) relapse post transplantation. The 3-year post-DLI survival rates for therapeutic and preemptive DLI recipients were 16.7% and 33.3%, respectively. The occurrence of DLI-associated acute graft-versus-host disease predicted longer survival, whereas diagnosis of T cell acute lymphoblastic leukemia/lymphoma or myelodysplastic syndromes or early relapse after transplant (< 6 months) predicted shorter survival after therapeutic DLI. Cumulative incidence of progression to hematologic relapse and non-relapse mortality after preemptive DLI were 46.8% and 29.1%, respectively. Active disease prior to transplant and early molecular relapse after transplant (< 4 months) were the strongest predictors of non-relapse mortality after preemptive DLI. In conclusion, although therapeutic DLI had limited efficacy against T cell acute lymphoblastic leukemia/lymphoma or myelodysplastic syndromes or early post-transplant relapse, patients who developed DLI-associated acute graft-versus-host disease would benefit from this procedure in the setting of G-SCF-mobilized DLI. Furthermore, preemptive DLI could protect half of patients from hematologic relapse after transplantation with acceptable toxicity.


Similar content being viewed by others
References
Horowitz M, Schreiber H, Elder A, Heidenreich O, Vormoor J, Toffalori C, et al. Epidemiology and biology of relapse after stem cell transplantation. Bone Marrow Transplant. 2018;53(11):1379–89.
Yanada M, Konuma T, Yamasaki S, Kondo T, Fukuda T, Shingai N, et al. Relapse of acute myeloid leukemia after allogeneic hematopoietic cell transplantation: clinical features and outcomes. Bone Marrow Transplant. 2021;56(5):1126–33.
Pavletic SZ, Kumar S, Mohty M, de Lima M, Foran JM, Pasquini M, et al. NCI first international workshop on the biology, prevention, and treatment of relapse after allogeneic hematopoietic stem cell transplantation: report from the committee on the epidemiology and natural history of relapse following allogeneic cell transplantation. Biol Blood Marrow Transplant. 2020;16(7):871–90.
Yan CH, Liu DH, Liu KY, Xu LP, Liu YR, Chen H, et al. Risk stratification-directed donor lymphocyte infusion could reduce relapse of standard-risk acute leukemia patients after allogeneic hematopoietic stem cell transplantation. Blood. 2012;119(14):3256–62.
Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W. Donor lymphocyte infusion for the treatment of leukemia relapse after HLA-mismatched/haploidentical T-cell-replete hematopoietic stem cell transplantation. Haematologica. 2007;92(3):414–7.
Zeidan AM, Forde PM, Symons H, Chen A, Smith BD, Pratz K, et al. HLA-haploidentical donor lymphocyte infusions for patients with relapsed hematologic malignancies after related HLA-haploidentical bone marrow transplantation. Biol Blood Marrow Transplant. 2014;20(3):314–8.
Kharfan-Dabaja MA, Labopin M, Polge E, Nishihori T, Bazarbachi A, Finke J, et al. Association of second allogeneic hematopoietic cell transplant vs donor lymphocyte infusion with overall survival in patients with acute myeloid leukemia relapse. JAMA Oncol. 2018;4(9):1245–53.
Chen Y, Cheng Y, Suo P, Yan C, Wang Y, Chen Y, et al. Donor-derived CD19-targeted T cell infusion induces minimal residual disease-negative remission in relapsed B-cell acute lymphoblastic leukaemia with no response to donor lymphocyte infusions after haploidentical haematopoietic stem cell transplantation. Br J Haematol. 2017;79(4):598–605.
Gao XN, Lin J, Wang SH, Huang WR, Li F, Li HH, et al. Donor lymphocyte infusion for prevention of relapse after unmanipulated haploidentical PBSCT for very high-risk hematologic malignancies. Ann Hematol. 2019;98(1):185–93.
Gao XN, Lin J, Wang LJ, Li F, Li HH, Wang SH, et al. Comparison of the safety and efficacy of prophylactic donor lymphocyte infusion after haploidentical versus matched-sibling PBSCT in very high-risk acute myeloid leukemia. Ann Hematol. 2019;98(5):1267–77.
Rowlings PA, Przepiorka D, Klein JP, Gale RP, Passweg JR, Henslee-Downey PJ, et al. IBMTR severity index for grading acute graft-versus-host disease: retrospective comparison with Glucksberg grade. Br J Haematol. 1997;97(4):855–64.
Schmid C, Labopin M, Nagler A, Bornhäuser M, Finke J, Fassas A, et al. Donor lymphocyte infusion in the treatment of first hematological relapse after allogeneic stem-cell transplantation in adults with acute myeloid leukemia: a retrospective risk factors analysis and comparison with other strategies by the EBMT acute leukemia working party. J Clin Oncol. 2007;25(31):4938–45.
Döhner H, Estey EH, Amadori S, Appelbaum FR, Büchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115(3):453–74.
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD, et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006;108(2):419–25.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. International harmonization project on lymphoma. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25(5):579–86.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47.
Schroeder T, Rachlis E, Bug G, Stelljes M, Klein S, Steckel NK, et al. Treatment of acute myeloid leukemia or myelodysplastic syndrome relapse after allogeneic stem cell transplantation with azacitidine and donor lymphocyte infusions–a retrospective multicenter analysis from the German cooperative transplant study group. Biol Blood Marrow Transplant. 2015;21(4):653–60.
Cheson BD, Bennett JM, Kopecky KJ, Büchner T, Willman CL, Estey EH, et al. Revised recommendations of the international working group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol. 2003;21(24):4642–9.
Scrucca L, Santucci A, Aversa F. Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transplant. 2007;40(4):381–7.
Scrucca L, Santucci A, Aversa F. Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transplant. 2010;45(9):1388–95.
Chang YJ, Zhao XY, Huang XJ. Granulocyte colony-stimulating factor-primed unmanipulated haploidentical blood and marrow transplantation. Front Immunol. 2019;10:2516.
Takami A, Yano S, Yokoyama H, Kuwatsuka Y, Yamaguchi T, Kanda Y, et al. Donor lymphocyte infusion for the treatment of relapsed acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation: a retrospective analysis by the adult acute myeloid leukemia working group of the Japan society for hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2014;20(11):1785–90.
Schmid C, Labopin M, Nagler A, Niederwieser D, Castagna L, Tabrizi R, et al. Treatment, risk factors, and outcome of adults with relapsed AML after reduced intensity conditioning for allogeneic stem cell transplantation. Blood. 2012;119(6):1599–606.
Bejanyan N, Weisdorf DJ, Logan BR, Wang HL, Devine SM, de Lima M, et al. Survival of patients with acute myeloid leukemia relapsing after allogeneic hematopoietic cell transplantation: a center for international blood and marrow transplant research study. Biol Blood Marrow Transplant. 2015;21(3):454–9.
Yan CH, Xu LP, Liu DH, Chen H, Wang Y, Wang JZ, et al. Low-dose methotrexate may preserve a stronger antileukemic effect than that of cyclosporine after modified donor lymphocyte infusion in unmanipulated haploidentical HSCT. Clin Transplant. 2015;29(7):594–605.
Yan CH, Liu DH, Xu LP, Liu KY, Zhao T, Wang Y, et al. Modified donor lymphocyte infusion-associated acute graft-versus-host disease after haploidentical T-cell-replete hematopoietic stem cell transplantation: incidence and risk factors. Clin Transplant. 2012;26(6):868–76.
Xuan L, Wang Y, Chen J, Jiang E, Gao L, Wu B, et al. Sorafenib therapy is associated with Improved outcomes for FMS-like tyrosine kinase 3 internal tandem duplication acute myeloid leukemia relapsing after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2019;25(8):1674–81.
Zucenka A, Vaitekenaite V, Maneikis K, Davainis L, Pileckyte R, Trociukas I, et al. Venetoclax-based salvage therapy followed by Venetoclax and DLI maintenance vs. FLAG-Ida for relapsed or refractory acute myeloid leukemia after allogeneic stem cell transplantation. Bone Marrow Transplant. 2021;56(11):2804–12.
Schmidt S, Liu Y, Hu ZH, Williams KM, Lazarus HM, Vij R, et al. The role of donor lymphocyte infusion (DLI) in post-hematopoietic cell transplant (HCT) relapse for chronic myeloid leukemia (CML) in the tyrosine kinase inhibitor (TKI) era. Biol Blood Marrow Transplant. 2020;26(6):1137–43.
Mathew NR, Baumgartner F, Braun L, O’Sullivan D, Thomas S, Waterhouse M, et al. Sorafenib promotes graft-versus-leukemia activity in mice and humans through IL-15 production in FLT3-ITD-mutant leukemia cells. Nat Med. 2018;24(3):282–91.
Acknowledgements
This work was partially supported by grants from the National Natural Science Foundation of China (81870109 and 82070149 to X-N G) and Natural Science Foundation of Beijing Municipality (7202191 to X-N G).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Lu, N., Lin, J., Wang, LL. et al. A retrospective single-center analysis of G-CSF-mobilized donor lymphocyte infusion in hematologic malignancies after unmanipulated allogenic PBSCT. Int J Hematol 115, 713–727 (2022). https://doi.org/10.1007/s12185-022-03298-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03298-9