Abstract
Norovirus gastroenteritis (NV-GE) is a highly transmittable disease that can lead to fatal outcomes in vulnerable populations including patients after hematopoietic stem cell transplantation (HSCT). Prompt detection of NV is therefore important for HSCT recipients. Immunochromatography (IC) can be used to easily and rapidly diagnose NV-GE by detecting NV antigens. In this study, we examined 642 stool specimens in patients who developed diarrhea after allogeneic HSCT between January 2007 and June 2011. NV was detected in 10 of 350 (2.9 %) HSCT recipients. The median onset of symptoms was 36 days (range 3–93) after HSCT. The median duration of symptoms was 42 days (3–135). A second or subsequent allogeneic HSCT was associated with a higher incidence of NV-GE (P = 0.034). Of four patients who underwent colonoscopy, two showed intestinal graft-versus-host disease (GVHD) histopathology, whereas the other two showed no evidence of GVHD, and thus no need for intensified immunosuppression. None of the patients died of NV-GE. In conclusion, IC may be useful in the differential diagnosis of diarrhea after allogeneic HSCT, and could enable the appropriate adjustment of immunosuppressive drugs and prompt preventive measures.
Similar content being viewed by others
Introduction
Norovirus (NV) is a major cause of gastroenteritis in both sporadic cases and outbreaks worldwide [1]. NV gastroenteritis (NV-GE) is highly infectious and transmittable. Outbreaks often occur among not only healthy people but also vulnerable individuals in hospitals and nursing homes, and thus NV-GE is considered to be a major public health problem worldwide [2]. Therefore, the early diagnosis of NV-GE is necessary to prevent outbreaks [3].
It has been reported that immunocompromised hosts such as patients who have undergone solid organ transplantation and hematopoietic stem cell transplantation (HSCT) can develop NV-GE, which tends to be long-lasting and can be fatal [4–10]. Severe and life-threatening cases of NV-GE have been increasingly reported in both pediatric and adult patients who have undergone HSCT [11–14]. Roddie et al. [15] reported that 12 adult patients after allogeneic HSCT developed NV-GE and diarrhea tended to persist. Schwartz et al. [16] reported an outbreak of NV-GE in a hematology and transplantation unit. Eleven patients including 5 recipients after HSCT developed NV-GE and had a significantly longer duration of symptoms than infected medical staff. In both of these reports, NV-GE after HSCT was associated with an increased risk of morbidity and mortality. Thus, NV is considered to be an important emerging pathogen that causes GE after HSCT. However, little is known about the detailed prevalence, etiology and appropriate clinical management of NV-GE.
In allogeneic HSCT, patients often develop diarrhea due to various causes including regimen-related toxicity, infection and intestinal graft-versus-host disease (GVHD). The differential diagnosis between intestinal GVHD and infectious GE is important because the treatment strategies are different. While intestinal GVHD requires the intensification of immunosuppression, infectious GE might be worsened by the intensification of immunosuppression [13].
Although a tissue culture system for NV has not yet been established for the diagnosis of NV-GE, several methods have been developed for detecting NV in stool specimens, such as electron microscopy, radioimmunoassay, enzyme immunoassay and quantitative reverse transcription polymerase chain reaction (RT-PCR) [17]. RT-PCR is mainly used for the detection of NV because of its superior sensitivity and specificity compared with conventional methods [1]. Although quantitative RT-PCR for the detection of viral RNA in stool specimens has been used to diagnose NV-GE after HSCT in recent studies [11, 12, 15, 16], this method is not yet established as a standardized technique for widespread clinical use due to drawbacks such as its high cost and complicated techniques required [18]. On the other hand, several studies in other settings have demonstrated that immunochromatography (IC), which is based on the antigen–antibody reaction using a monoclonal antibody specific for virus-like particles, can be used to easily and rapidly detect NV antigen in stool samples by an in-house laboratory with high specificity, albeit with slightly less sensitivity, and at lower cost than RT-PCR [19–27]. An IC kit has recently been marketed in Asia and Europe [1]. Thus, IC might be a promising diagnostic tool in patients with NV-GE after HSCT in clinical practice, especially if we consider the urgent need for appropriate diagnosis and intervention in allogeneic HSCT recipients [28].
Here we report a single-center retrospective analysis of the detection of NV antigen using an IC kit with stool samples from patients with diarrhea after allogeneic HSCT in our institution to assess the prevalence, symptoms and clinical outcome of patients with NV-GE.
Patients and methods
Patients
We examined stool specimens to detect NV antigens in adult patients who developed diarrhea after allogeneic HSCT in both our HSCT unit and hematology ward between January 2007 and June 2011. Our HSCT unit has 26 beds with a high-efficiency particulate air filter system. The hematology ward is used for patients who have achieved neutrophil engraftment after HSCT. As prophylaxis against microorganisms such as bacteria, fungus and virus, levofloxacin, fluconazole and acyclovir were routinely used from the beginning of the conditioning regimen. This study was approved by the Institutional Review Board of National Cancer Center, Tokyo, Japan.
Stool collection and examination
Stool specimens were collected and examined to detect NV antigens in patients who developed diarrhea in our HSCT unit and hematology ward during the study period. Stool specimens that had been frozen at −40 °C between January 2007 and November 2008 were also retrospectively examined.
Laboratory method
A commercially available IC kit (QuickEx-Norovirus until 2009 and QuickNavi-Norovirus from 2010 to 2011, Denka Seiken, Tokyo, Japan) was used to detect NV antigens in stool specimens according to the manufacturer’s instructions. Briefly, a stool specimen was diluted in the provided buffer tube, and the suspension was filtered and applied to the sample well of the kit. If the stool specimen contained NV, NV would react with latex-coated mouse monoclonal antibodies specific for NV genogroups I and II. During 15 min of incubation, the antigen–antibody complex migrated along the membrane and was captured by NV-specific monoclonal antibodies immobilized in the test line, and a blue color appeared. The complex was also captured by rabbit anti-mouse immunoglobulin immobilized in the control line, and a blue line became visible. If the sample did not contain NV, only the blue control line was present. The IC kit can detect NV antigen in stool specimens within a total time of 30 min by an in-house laboratory. Stool specimens were also examined by a Clostridium difficile (CD) toxin test, which can be used to detect CD toxins A and B by enzyme immunoassay [29].
Prevention and control of NV infection
We promptly implemented both the isolation of infected patients and an enhanced hygiene strategy after a diagnosis of NV-GE. Environmental surfaces in the rooms of patients with NV-GE were also disinfected using sodium hypochlorite. Isolation was continued until symptoms were completely resolved.
Statistical analysis
We used Fisher’s exact test to compare categorical covariates and the Mann–Whitney U test to compare continuous covariates. NV-GE and NV-GE-free mortality were considered as competing risk events for each other. The incidences of NV-GE and NV-GE-free mortality were estimated by cumulative incidence functions, and differences between groups were evaluated by the Gray test. The incidence of NV-GE was estimated as the probability at 1 year from allogeneic HSCT. In univariate analyses, Eastern Cooperative Oncology Group performance status (ECOG PS) >1 before HSCT, primary disease of lymphoma, second or subsequent allogeneic HSCT, and non-complete remission (non-CR) at HSCT were included as categorical covariates. For multivariate analyses, we included covariates that had a P value of <0.1 in univariate analyses. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R Commander that was designed to add statistical functions that are frequently used in biostatistics [30].
Results
Patient characteristics
Between January 2007 and June 2011, a total of 374 allogeneic HSCT procedures were performed at our center (350 recipients), and we tested 642 stool specimens from 235 recipients (67 % of total recipients) who developed diarrhea after allogeneic HSCT, as shown in Table 1. There was no apparent time trend in the incidence of NV-GE over this period. The characteristics of all of the allogeneic HSCT recipients and patients with NV-GE are shown in Tables 2 and 3. NV was detected in 10 patients (2.9 % of total recipients and 4.3 % of recipients with diarrhea) after allogeneic HSCT. Frozen stool specimens from Patient Nos. 1–3 were examined retrospectively. The median age of these patients with NV-GE was 49.5 years (range 29–65). Patients with NV-GE were more likely to have undergone a second or subsequent allogeneic HSCT than those without NV-GE (P = 0.033). The median time from allogeneic HSCT to the onset of symptoms was 36 days (range 3–93) among recipients who were diagnosed as NV-GE. The median time from allogeneic HSCT to the diagnosis of NV-GE was 42.5 days (range 11–101).
Prevalence and risk factors
The 1-year cumulative incidence of NV-GE was 2.9 %. The 1-year incidence of NV-GE was 8.5 % in recipients with a second or subsequent allogeneic HSCT and 2.0 % in those with a first allogeneic HSCT, as shown in Fig. 1 (P = 0.013). The other covariates with a P value of <0.1 were lymphoma (P = 0.093), non-CR (P = 0.069), and ECOG PS >1 before HSCT (P = 0.068). A multivariate analysis showed that a second or subsequent allogeneic HSCT was associated with an increased risk of NV-GE (P = 0.034).
Clinical outcomes
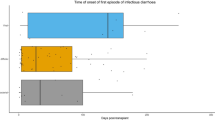
The clinical outcomes of patients who developed NV-GE are summarized in Table 3. The median duration of symptoms was 42 days (range 3–135). The symptoms of NV-GE included nausea (60 %), abdominal pain (50 %), vomiting (40 %), and fever (20 %), in addition to diarrhea. The volume of diarrhea was more than 500 ml per day in 4 patients (40 %). At the diagnosis of NV-GE, all patients received immunosuppressive agents, and 2 received systemic corticosteroid as treatment for GVHD. Figure 2 shows the timing of the diagnosis of NV-GE and intestinal GVHD, and Supplemental Fig. 1 shows the details of the relationship between NV-GE and intestinal GVHD. Among 4 patients who underwent colonoscopy, intestinal GVHD was diagnosed in 2 based on histopathological findings, whereas the other 2 had no evidence of intestinal GVHD, which resulted in no need for the intensification of immunosuppression. Of the 10 patients with NV-GE, 5 were alive with a median follow-up of 1721 days (range 890–2036) after the diagnosis of NV-GE. None of the patients died of NV-GE, and 5 died of other causes (disease progression, 3; GVHD-related, 2) at a median of 118 days (range, 92–233) after allogeneic HSCT. There was no outbreak of NV-GE during the study period.
Onset and duration of diarrhea and timing of diagnosis of NV-GE and intestinal GVHD after allogeneic HSCT. Five patients (Nos. 2, 6, 8, 9, and 10) became positive for NV at the second time of testing through an episode of diarrhea. Patient Nos. 2 and 6 developed NV-GE after steroid therapy for intestinal GVHD. Patient Nos. 8, 9 and 10 were diagnosed as NV-GE several days after the onset of diarrhea. Numbers indicate the days from the onset of symptoms to the diagnosis of NV-GE. Filled downward triangles indicates the diagnosis of intestinal GVHD by colonoscopy, open downward triangles no diagnosis of intestinal GVHD by colonoscopy, Filled circle positive for NV-Ag, open circle negative for NV-Ag, Filled diamond diagnosis of CMV disease, plus sign death
CD infection
Twenty-two patients with diarrhea after allogeneic HSCT were positive for CD toxin (6.3 % of total recipients and 9.4 % of recipients with diarrhea). The median time from allogeneic HSCT to the diagnosis of CD infection was 21 days (range 0–284). NV was also detected concomitantly in 1 of the 22 patients with CD infection (4.5 %).
Discussion
In the present study, 10 of 350 patients were diagnosed as NV-GE after allogeneic HSCT using IC. To our knowledge, this is the first report on the use of IC to detect NV antigen after allogeneic HSCT. This method was useful for the rapid detection of NV antigen and helpful in the differential diagnosis of diarrhea after allogeneic HSCT. Although NV-GE is a potentially fatal disease in immunocompromised patients, none of the patients in our study died of NV-GE. These findings suggest that IC might enable the appropriate adjustment of immunosuppressive drugs and could allow us to take prompt preventive measures.
The prevalence of NV-GE after allogeneic HSCT in this study was 2.9 %. There have been a few reports on NV-GE in adult and pediatric patients after HSCT (Table 4), and the estimated incidence of NV-GE has been stated to be 10–20 % [12, 15]. Despite the difference in the backgrounds among these studies, the lower incidence of NV-GE in our report than in other reports suggests that some patients who are diagnosed as NV-GE by RT-PCR might be overlooked by IC [18–20, 22, 24, 27] because the IC kit was reported to have a lower sensitivity in patients who were diagnosed by RT-PCR. However, IC might have adequate sensitivity comparable to those of other methods for detecting a high viral load in the early phase of the disease, since there was no apparent NV outbreak during our study period [23]. Moreover, it is still unclear whether patients who are positive by RT-PCR but negative by IC have infectious potential and are clinically significant [13, 31, 32]. The significance of false-negative cases according to the IC kit should be evaluated in a future study.
The etiology of NV infection was unclear. We did not have any episode that infected persons such as medical staff or visitors had contacted the patients. However, we cannot exclude the possibility of NV transmission to the patients from people with NV infections. On the other hand, the immunosuppression due to HSCT might have induced the development of NV-GE in patients with subclinical infection [33]. In fact, a second or subsequent allogeneic HSCT was associated with NV-GE in our analysis, which suggests that immunocompromised HSCT recipients with no previous diagnosis of NV-GE may tend to develop NV-GE after further immunosuppression. After a diagnosis of NV-GE, it has been reported that immunocompromised patients whose symptoms have resolved still exhibit the prolonged excretion of NV in stool specimens, which can be detected by RT-PCR [11, 12, 34]. Roddie et al. [15] reported the recurrence of NV-GE with the original strain in a patient who had low viral loads after the relief of symptoms and intensified immunosuppressive therapy for GVHD. Therefore, immunocompromised patients with a low viral load might be at risk for the development or relapse of NV-GE when immunosuppression is intensified.
The spectrum and severity of symptoms have varied among studies. One possible explanation for these differences is the difference in patient characteristics. For example, the median duration of symptoms was 3 months in the study by Roddie et al., 42 days in our study, and 7 days in the study by Schwartz et al., and this discrepancy might be due to the difference in the degree of immunosuppression among the studies [34, 35]. In the first study by Roddie et al., 8 of 12 recipients underwent allogeneic HSCT with in vivo T-cell depletion using alemtuzumab. In our study, all 10 recipients who underwent allogeneic HSCT received T-cell replete grafts, and in the study by Schwartz et al., most patients received conventional chemotherapy [15, 16].
Although NV-GE is a potentially fatal disease in immunocompromised patients, none of the patients in our study died of NV-GE [15, 16]. Among the 5 patients who died, 3 (Patient Nos. 1, 7, and 8) died due to disease progression without gastrointestinal symptoms, and 2 (Patient Nos. 2 and 6) died due to GVHD-related comorbidities such as severe infection other than NV-GE during steroid treatment for refractory GVHD. Patient No. 2 developed Bifidobacterium bacteremia and candidemia a few days before the diagnosis of NV-GE, and Patient No. 6 developed severe bilateral pneumonia of unknown etiology just after the diagnosis of NV-GE. These complications, rather than NV-GE, were clinically considered to be the main cause of death in these patients. We continued supportive care in patients with NV-GE who were not diagnosed as intestinal GVHD without intensifying immunosuppression, and their symptoms resolved gradually. We carefully intensified immunosuppression in patients with NV-GE who were previously or simultaneously diagnosed as intestinal GVHD.
This study has several limitations. First, although we routinely performed this test in patients who developed diarrhea after allogeneic HSCT, we did not check diarrhea according to a pre-defined protocol for sample collection. Thus, there may be the possibility that the cumulative incidence of NV infection is underestimated. Second, we examined frozen stool specimens that had been stored in a deep freezer (−40 °C) for the first cohort of this study. The freezing and thawing procedure might have influenced the results obtained by IC. Third, we did not compare the results obtained by IC to those by RT-PCR. According to the manufacturer, the IC kit that we used (QuickNavi-Noro) had 81.6 % sensitivity and 96.9 % specificity in patients with NV-GE diagnosed by RT-PCR, and the overall concordance rate between IC and RT-PCR was 89.3 %. However, some reports have described a lower sensitivity for IC, which was probably due to the differences in background of the studies, such as population, genotype of NV, viral load, specimen handling and antibodies used in the kits [18–20, 22, 24, 27]. RT-PCR and IC in the setting of HSCT should be compared in a prospective study.
In conclusion, our data demonstrated that NV-GE can be rapidly diagnosed by IC in patients who have developed diarrhea after allogeneic HSCT. In a future study, the usefulness of IC should be validated in immunocompromised populations including patients after allogeneic HSCT.
References
Glass RI, Parashar UD, Estes MK. Norovirus gastroenteritis. N Engl J Med. 2009;361:1776–85.
Updated norovirus outbreak management and disease prevention guidelines. MMWR Recomm Rep. 2011;60:1–18.
Greig JD, Lee MB. A review of nosocomial norovirus outbreaks: infection control interventions found effective. Epidemiol Infect. 2012;140:1151–60.
Morotti RA, Kaufman SS, Fishbein TM, Chatterjee NK, Fuschino ME, Morse DL, et al. Calicivirus infection in pediatric small intestine transplant recipients: pathological considerations. Hum Pathol. 2004;35:1236–40.
Capizzi T, Makari-Judson G, Steingart R, Mertens WC. Chronic diarrhea associated with persistent norovirus excretion in patients with chronic lymphocytic leukemia: report of two cases. BMC Infect Dis. 2011;11:131.
Roos-Weil D, Ambert-Balay K, Lanternier F, Mamzer-Bruneel MF, Nochy D, Pothier P, et al. Impact of norovirus/sapovirus-related diarrhea in renal transplant recipients hospitalized for diarrhea. Transplantation. 2011;92:61–9.
Ebdrup L, Bottiger B, Molgaard H, Laursen AL. Devastating diarrhoea in a heart-transplanted patient. J Clin Virol. 2011;50:263–5.
Boillat Blanco N, Kuonen R, Bellini C, Manuel O, Estrade C, Mazza-Stalder J, et al. Chronic norovirus gastroenteritis in a double hematopoietic stem cell and lung transplant recipient. Transpl Infect Dis. 2011;13:213–5.
Kim MJ, Kim YJ, Lee JH, Lee JS, Kim JH, Cheon DS, et al. Norovirus: a possible cause of pneumatosis intestinalis. J Pediatr Gastroenterol Nutr. 2011;52:314–8.
Kaltsas A, Sepkowitz K. Community acquired respiratory and gastrointestinal viral infections: challenges in the immunocompromised host. Curr Opin Infect Dis. 2012;25:423–30.
Saif MA, Bonney DK, Bigger B, Forsythe L, Williams N, Page J, et al. Chronic norovirus infection in pediatric hematopoietic stem cell transplant recipients: a cause of prolonged intestinal failure requiring intensive nutritional support. Pediatr Transplant. 2011;15:505–9.
Robles JD, Cheuk DK, Ha SY, Chiang AK, Chan GC. Norovirus infection in pediatric hematopoietic stem cell transplantation recipients: incidence, risk factors, and outcome. Biol Blood Marrow Transplant. 2012;18:1883–9.
Bok K, Green KY. Norovirus gastroenteritis in immunocompromised patients. N Engl J Med. 2012;367:2126–32.
Doshi M, Woodwell S, Kelleher K, Mangan K, Axelrod P. An outbreak of norovirus infection in a bone marrow transplant unit. Am J Infect Control. 2013;41:820–3.
Roddie C, Paul JP, Benjamin R, Gallimore CI, Xerry J, Gray JJ, et al. Allogeneic hematopoietic stem cell transplantation and norovirus gastroenteritis: a previously unrecognized cause of morbidity. Clin Infect Dis. 2009;49:1061–8.
Schwartz S, Vergoulidou M, Schreier E, Loddenkemper C, Reinwald M, Schmidt-Hieber M, et al. Norovirus gastroenteritis causes severe and lethal complications after chemotherapy and hematopoietic stem cell transplantation. Blood. 2011;117:5850–6.
Atmar RL, Estes MK. Diagnosis of noncultivatable gastroenteritis viruses, the human caliciviruses. Clin Microbiol Rev. 2001;14:15–37.
Takanashi S, Okame M, Shiota T, Takagi M, Yagyu F, Tung PG, et al. Development of a rapid immunochromatographic test for noroviruses genogroups I and II. J Virol Methods. 2008;148:1–8.
Bruins MJ, Wolfhagen MJ, Schirm J, Ruijs GJ. Evaluation of a rapid immunochromatographic test for the detection of norovirus in stool samples. Eur J Clin Microbiol Infect Dis. 2010;29:741–3.
Kirby A, Gurgel RQ, Dove W, Vieira SC, Cunliffe NA, Cuevas LE. An evaluation of the RIDASCREEN and IDEIA enzyme immunoassays and the RIDAQUICK immunochromatographic test for the detection of norovirus in faecal specimens. J Clin Virol. 2010;49:254–7.
Bruggink LD, Witlox KJ, Sameer R, Catton MG, Marshall JA. Evaluation of the RIDA((R))QUICK immunochromatographic norovirus detection assay using specimens from Australian gastroenteritis incidents. J Virol Methods. 2011;173:121–6.
Battaglioli G, Nazarian EJ, Lamson D, Musser KA, St George K. Evaluation of the RIDAQuick norovirus immunochromatographic test kit. J Clin Virol. 2012;53:262–4.
Geginat G, Kaiser D, Schrempf S. Evaluation of third-generation ELISA and a rapid immunochromatographic assay for the detection of norovirus infection in fecal samples from inpatients of a German tertiary care hospital. Eur J Clin Microbiol Infect Dis. 2012;31:733–7.
Park KS, Baek KA, Kim DU, Kwon KS, Bing SH, Park JS, et al. Evaluation of a new immunochromatographic assay kit for the rapid detection of norovirus in fecal specimens. Ann Lab Med. 2012;32:79–81.
Kim HS, Hyun J, Kim JS, Song W, Kang HJ, Lee KM. Evaluation of the SD Bioline Norovirus rapid immunochromatography test using fecal specimens from Korean gastroenteritis patients. J Virol Methods. 2012;186:94–8.
Pombubpa K, Kittigul L. Assessment of a rapid immunochromatographic test for the diagnosis of norovirus gastroenteritis. Eur J Clin Microbiol Infect Dis. 2012;31:2379–83.
Ambert-Balay K, Pothier P. Evaluation of 4 immunochromatographic tests for rapid detection of norovirus in faecal samples. J Clin Virol. 2013;56:194–8.
Ljungman P. Molecular monitoring of viral infections after hematopoietic stem cell transplantation. Int J Hematol. 2010;91:596–601.
Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection. Clin Infect Dis. 2008;46(Suppl 1):S12–8.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Sukhrie FH, Siebenga JJ, Beersma MF, Koopmans M. Chronic shedders as reservoir for nosocomial transmission of norovirus. J Clin Microbiol. 2010;48:4303–5.
Sukhrie FH, Teunis P, Vennema H, Copra C, Thijs Beersma MF, Bogerman J, et al. Nosocomial transmission of norovirus is mainly caused by symptomatic cases. Clin Infect Dis. 2012;54:931–7.
Gallimore CI, Cubitt D, du Plessis N, Gray JJ. Asymptomatic and symptomatic excretion of noroviruses during a hospital outbreak of gastroenteritis. J Clin Microbiol. 2004;42:2271–4.
Furuya D, Kuribayashi K, Hosono Y, Tsuji N, Furuya M, Miyazaki K, et al. Age, viral copy number, and immunosuppressive therapy affect the duration of norovirus RNA excretion in inpatients diagnosed with norovirus infection. Jpn J Infect Dis. 2011;64:104–8.
Tomov VT, Osborne LC, Dolfi DV, Sonnenberg GF, Monticelli LA, Mansfield K, et al. Persistent enteric murine norovirus infection is associated with functionally suboptimal virus-specific CD8 T cell responses. J Virol. 2013;87:7015–31.
Acknowledgments
The authors thank Ms. Mariko Ohnishi for immunochromatographic analysis and clinical research assistance. This work was supported by grants from the Japanese Ministry of Health, Labour and Welfare and the Advanced Clinical Research Organization. Some of these results were presented at the 38th Annual Meeting of the European Group for Blood and Marrow Transplantation in Geneva, Switzerland, April 2, 2012.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Ueda, R., Fuji, S., Mori, Si. et al. Characteristics and outcomes of patients diagnosed with norovirus gastroenteritis after allogeneic hematopoietic stem cell transplantation based on immunochromatography. Int J Hematol 102, 121–128 (2015). https://doi.org/10.1007/s12185-015-1804-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-015-1804-2