Abstract
Purpose of Review
The purpose of this paper is to illustrate how telemedicine can be beneficial in many areas of orthopedic clinical practice through a literature narrative review. In addition, we discuss advantages, barriers, and enablers of such technology.
Recent Findings
Telemedicine in orthopedics was initially described to discuss simple cases among non-specialist doctors through videoconferencing. Recently, it evolved to postoperative follow-up on selected cases, physical examination, and even teleconsultations direct to patients. Studies have reported that consultation can be offered safely to selected patients. Although this topic is already being addressed for a long time, recent studies have reported that there is still resistance among many orthopedic surgeons.
Summary
Telemedicine for orthopedics has safely expanded its operations. It can be used in postoperative follow-up of selected cases, fracture follow-up, and even in pediatric cases. Remote diagnosis of fractures is done successfully on an outpatient basis in many countries. Protocols and methods to standardize the virtual orthopedic examination for common musculoskeletal conditions have been developed. Satisfaction with teleconsultations as well as cost-effectiveness of remote care orthopedics were already well reported by some studies. We believe that remote care will be expanded in several hospitals around the world due to its huge potential. This fact is explained by natural technological development and by change and obliteration of habits accelerated exponentially after COVID-19 crisis.
Similar content being viewed by others
Introduction
Telemedicine is a broad term and can be simplistically defined as provision of medical services through distance. This definition encompasses many applications, such as diagnostic asynchronous evaluation, continuous monitoring using biosensors, and synchronous video consultations, as well as multiple variations on each theme [1]. Currently it can be considered a hot topic, and the adoption is skyrocketing, virtually in any medical specialty and service.
Although the boom was brought up by widely available broadband internet, the history of telemedicine began more than 50 years ago. Advances in telecommunication technologies over the last decades changed the way healthcare services can be provided. Since the 1940’s, x-ray images have been transmitted by telephone and radio from underserved areas to reference centers with reasonable quality, and there are many programs, from more than 40 years ago, using two-way communication and ancient closed-circuit TV systems to provide medical consultations to distant locations [2].
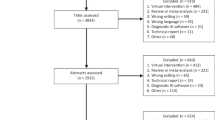
After development and vast adoption of smart and connected devices, along with cheaper and accessible internet, telemedicine growth and maturing escalated in an exponential fashion. The same occurred with science and publications in the field. Using the MESH term “telemedicine,” which also looks for similar terms like “Mobile Health,” “mHealth,” “telehealth,” and “e-health,” the number of search results in PubMed has grown from a few dozen per year in the beginning of the 1990s to more than three thousand articles published only in 2019. The terms also indicate a strong relationship between health and digital interfaces—artifacts whose efficiency is linked on user-centered interaction design projects. Using the same taxonomy of telemedicine, the application of communications technologies to provide healthcare at a distance in the field of orthopedics is being called “tele-orthopedics” [3]. Published data regarding specifically tele-orthopedics is still in its infancy, with the pioneering attempts dating to 1996 [4]. Since then, however, many more services have been developed, and too much data is being published.
Orthopedics is a specialty that can benefit greatly from telemedicine. In addition to being cost-effective, it presents good patient-reported outcomes and is considered an opportunity with potential to be explored [5•]. Since COVID-19 pandemic is tipping point in telemedicine adoption curve, which now shows exponential growth in most countries, there are multiple appropriate telemedicine applications suggested for orthopedic practice, such as teleconsultation for diagnosis, treatment, and patient follow-up; virtual rehabilitation; or even offering specialized advice in a teleconsultation for non-specialist doctors [1, 6]. This narrative review will focus on telemedicine applied to orthopedics: its limits, potential usages, results of published data, best practices, and the experience of mature tele-orthopedic services. As a result, we intend to encourage orthopedic surgeons and clinics to design and implement their own telemedicine service.
History and Potential Usage for Telemedicine in Orthopedics
Potential uses of communication technologies in healthcare are huge, but what is attracting most attention of those interested in this phenomenon is its use for performing teleconsultations in daily clinical practice. The majority of studies about this topic reports the experience of independent services. Lamminen et al. [4] published one of the first articles about orthopedic telehealth in 1996. In this study conducted in Finland, authors reported their experience with a service of videoconferencing for consultation and communication among doctors. Physical exam was also transmitted by video. Interestingly, at that time, the authors already discussed an important issue that still remain current: “who takes responsibility for the whole system when it breaks down?”. In addition, they describe some simple tasks before the videoconferencing, such as correctly positioning the camera, in order to save time.
Lambrecht et al. [7] reported in 1997 an analysis of 410 orthopedic teleconsultations done during a 2-year period by three orthopedic surgeons. The reason for teleconsultation was evaluation and treatment of fractures in 43% of the patients, ligamentous injury, joint swelling or infection in 35%, postoperative evaluation in 18%, and evaluation and treatment of dislocations in 4%. Mean duration for teleconsultations was 12.8 min. No adverse outcomes were observed, and final suggestion of authors was that telemedicine can be an option where orthopedic physicians are not available.
In 1999, Aarnio et al. [8] published a prospective study analyzing teleconsultation in orthopedics. Teleconsultations took place by videoconference between two 150 miles distant cities in Finland. The reasons for consultations were to establish diagnosis in 10 cases and to discuss clinical management in 14 cases and for follow-up in other five. The majority of consultations lasted between 11 and 15 min. At that time, quality of video was judged to be good by doctors. This is an important point because video and sound quality was a concern in the past, but with the advancement of technology, this problem is losing importance. However, each location has its characteristics, and video and sound quality can represent an important barrier for the implementation of telemedicine for this purpose. Also, this was one of the first studies that reported data about patient satisfaction, 87% percent of patients thought that it was a good or very good method and the rest felt that it was satisfactory.
Remote diagnosis of fractures is done successfully on an outpatient basis in many countries. McGill et al. [9] remotely followed non-surgical fractures successfully from a technical point of view, in a rural area. They reported that undisplaced fractures and postoperative wound reviews were commonly seen and considered well managed in such situations. Another study has shown similar results [3]. Caffery et al. [3] explored Australian-based tele-orthopedic services and also reported technology use mainly for fractures and peri-operative consultations. Authors of both studies highlight importance of such service in rural and remote areas. Prada et al. [10] also had conducted a study which demonstrated efficiency in handling cases with family doctors. Rural populations are greatly benefited by this strategy, highlighting benefit arising from convenience of avoiding long-distance transportation by orthopedic patients, often with mobility difficulties due to their own diagnosis [10].
It is interesting to note that despite rapid advancement of technology and although this subject is already being addressed for a long time, recent studies have reported that there is still resistance by the health team [3]. However, it is possible that the same resistant staff become an enabler as it uses tele-orthopedic service and realizes benefits for the patient [3]. Another reason for concern by orthopedists is physical examination, since many think that it is unfeasible to accomplish by video. In this way, regarding orthopedic clinical examination through video consultations, Tanaka et al. [11••] designed protocols and methods to standardize the virtual orthopedic examination for common musculoskeletal conditions. Other authors also have reported and validated the use of virtual tools, like internet-based goniometer, to help doctors during a virtual examination [12]. Obviously, there are inherent limitations of the virtual examination, and the orthopedist should evaluate when a face-to-face visit is necessary. Despite all these concerns, Buvik et al. [13], in a randomized controlled trial, suggested that virtual consultation can be offered safely to selected patients. The authors did not observe any difference in patient satisfaction and patient-reported health between video-assisted and in-person consultations.
When looking at medical literature, cost-effectiveness of remote care orthopedics is well established. Buvik et al. [14•] performed a randomized clinical trial to examine cost-effectiveness of telemedicine in remote orthopedic consultations. They have shown annual savings of $18,161 euros per 300 consultants by transportation costs and absenteeism from work, among others. This cost discrepancy was observed due to patient travel expenses. Another study that performed such economic evaluation was published by Atanda Jr. et al. [15]. Interestingly, in this case, they calculated and showed that there were cost savings to both the health system and patient. Despite these favorable results, it is important to understand that these data can be different in other scenarios.
Telemedicine for Postoperative Follow-Up
Telemedicine seems an important ally in improving care for patients undergoing orthopedic surgery. Several authors have used telemedicine for monitoring arthroplasty patients. Marsh et al. [16] compare in-person consultations and postoperative follow-up by telemedicine. By analyzing 229 patients (118 telemedicine and 111 usual-care group), authors found lower costs with web-based patients, less time spent traveling, and less time to complete consultations. All patients had at least 1 year of postoperative in this study. As it is a routine precaution among arthroplasty surgeons, wound observation in the immediate postoperative period and range of motion in person is mandatory. But in the near future, remote monitoring will probably improve even more. Postoperative follow-up has great advantages being made by video and with good acceptance [17].
In addition, Thomas et al. [18] previously demonstrated the importance of telemedicine as a tool for preoperative education in arthroplasty patients. In specific cases, rehabilitation of orthopedic surgery is already being carried out with telerehabilitation in selected cases. Especially in cases of arthroplasty, there are striking results in literature. It is reported that the home environment is safe and patients can engage more in rehabilitation in this situation. Eichler et al. [19], in a randomized controlled study, demonstrated equivalent results between two types of in-person and virtual rehabilitation by comparing functional outcomes, pain, and quality of life. However, patients with in-person rehabilitation had a higher rate of return to work.
Telemedicine for Pediatric Population
Regarding pediatric teleconsultation, Abel et al. [20••] conducted a comparative study for determining if patients between the ages 10 and 20 years that underwent knee arthroscopy surgery could have a reliable teleconsultation as first postoperative visit. According to the authors, home telemedicine visits have similar results when range of motion, incision color, and effusion size are evaluated. In this study, 96% of patients reported satisfaction with telemedicine visit. The main reason for that was time saved and convenience. Another study carried out among general practitioners in an African country with a specialized surgeon in pediatric orthopedics in France evaluated the feasibility of teleconsultation in 48 pediatric cases. Authors reported that 77% of the 48 teleconsultations had the clinical management decision changed after advice from the expert in France. Authors also highlighted that physical isolation and limited socioeconomic resources in many countries would benefit from international cooperation [21].
Atanda et al. [15] retrospectively analyzed 120 teleconsultations from patients under 18 years of age. As a result, a high level of satisfaction (more than 90%) was observed. Telemedicine visits were performed for follow-up, postoperative, and preoperative counseling. In addition to labor costs, visit and wait times were shorter in telemedicine visits. Telemedicine for pediatric population, which initially may seem challenging, actually seems to be resolutive. The fact that young patients are early adopters of technology is the main advantage. Moreover, in many cases, parents or caregivers are just looking for information and guidance.
COVID-19 Experience
COVID-19 pandemic strongly intensified the entire process described so far in telemedicine for orthopedic areas. Patients undergoing urgent outpatient follow-up, the orthopedist’s own presence in the health system has been reinvented as a result of this situation. The importance of telemedicine appears even more necessary as a tool for orthopedic reality. Tanaka et al. [11••] make important systematizations for proper functioning of virtual orthopedic physical examination. At scheduling time, the patient needs to be prepared for teleconsultation. A checklist is filled, under which proper patient positioning is assured and audio and video devices are tested. In addition, all guidelines for proper orthopedic physical examination are described to increase efficiency. We agree that systematization is necessary for proper functioning of remote consultation. In addition, inspection and calculation of range of motion is essential for diagnosis of orthopedic pathologies. Now, with the growth of telemedicine adoption during the COVID-19 pandemic, these guidelines must be revised and expanded. Modifying orthopedic physical examination is a necessary challenge for orthopedists, which we saw as a fundamental adaptation to new times. Loeb et al. [22] also reported experience introducing telemedicine service during COVID-19 crisis. In rapid deployment for 5 days, authors describe how to carry out a project with a new dynamic and selection criteria consultation. Acute injuries and brace complications, for example, are mentioned as indications for face-to-face consultation. The need to educate patients for these new practices is also described. Interestingly, a major concern of the pandemic is a substantial decrease in orthopedic care due to coronavirus, but authors estimated that 50% of clinical volume was maintained with telemedicine implanted in their hospital.
Organization of telemedicine services is mandatory in post-pandemic time, and clinical pathways must be adapted for orthopedic care. Many orthopedic patients are at high risk for severe illness from COVID-19, and their care must be adapted.
Telemedicine and Design
Telemedicine can benefit from its intersections with various areas of design, as design for health [23] and design thinking methodologies [24]. There is a need for user-friendly graphic interfaces, which can be coupled with methodologies of interaction design [25] and UX (user experience) [26], going through stages of research, information architecture, prototyping, and user tests.
Interdisciplinary collaboration designing journey maps and generating artifacts to communicate telemedicine pathways to patients and users are opportunities to be developed [27].
Fatehi et al. [28] described that the development of telemedicine interventions can be done using design methods and a patient-centered approach. The authors mention 5 research stages—concept development, service design, pre-implementation, implementation, and post-implementation—where typical aspects of design are observed, such as accessibility, efficacy, usability, scalability, satisfaction, cost effectiveness, utilization, sustainability, and social impact.
Future Directions
Since telemedicine in orthopedics is already a reality and technology advances quickly, there are two points of concern: regulatory considerations and payment model. Regulatory considerations involve legal responsibilities and liability distributions, licensing, and information security protocols overseeing. Such discussion can only be solved by continuing debate by the medical community. Medical societies need to establish norms for each situation as well as define which payment models will be applied. The majority of healthcare financing around the world is still based on a fee-for-service model. There are several attempts to improve these models with value-based healthcare, bundle payment, and accountable care organization. However, there must be collaboration and extensive debate among all stakeholders involved in this process, such as paying sources, healthcare providers, politicians, software development teams, technology providers, and, last but not least, patients themselves. These adjustments are imperative to expand the use of telemedicine, with the necessary capillarity for healthcare systems, whether public or private.
Conclusion
Telemedicine for orthopedics has safely expanded its operations with high satisfaction and cost-effectiveness. It can be used in several scenarios as postoperative follow-up of selected cases, fracture follow-up, and even in pediatric cases. Remote diagnosis of fractures is done successfully in many countries. Standardization of virtual orthopedic examination for some musculoskeletal conditions have been developed, but there is a need of further expansion and validation. Remote care had dramatically increase in 2020 and will continue to expand due to the natural technological development and by change and obliteration of habits that were accelerated exponentially after COVID-19 crisis.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
David Novillo-Ortiz (2016) Framework for the implementation of a telemedicine service. Washington, DC.
Strehle EM, Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics? Arch Dis Child. 2006;91:956–9.
Caffery LJ, Taylor M, North JB, Smith AC. Tele-orthopaedics: a snapshot of services in Australia. J Telemed Telecare. 2017;23:835–41.
Lamminen H, Nevalainen J, Alho A, Lindholm TS, Tallroth K, Lepistö J. Experimental telemedicine in orthopaedics. J Telemed Telecare. 1996;2:170–3.
• Wongworawat MD, Capistrant G, Stephenson JM. The opportunity awaits to lead orthopaedic telehealth innovation. J Bone Jt Surg - Am. 2017;99:1–6 Summary on telehealth in orthopaedics. Considers new trends in patients and health services. It highlights need for paying sources to be included in the process.
Marcolino MS, Alkmim MB, Assis TGP, de Sousa LAP, Ribeiro ALP. Teleconsultorias no apoio à atenção primária à saúde em municípios remotos no Estado de Minas Gerais, Brasil. Rev Panam Salud Pública. 2014;35:345–52.
Lambrecht C, Canham W, Gattey P, Mckenzie G. Telemedicine and orthopaedic care: a review of 2 years of experience. Clin Orthop Relat Res Mar. 1997:228–32.
Aarnio P, Lamminen H, Lepistö J, Alho A. A prospective study of teleconferencing for orthopaedic consultations. J Telemed Telecare. 1999;5:62–6.
McGill A, North J. An analysis of an ongoing trial of rural videoconference fracture clinics. J Telemed Telecare. 2012;18:470–2.
Prada C, Izquierdo N, Traipe R, Figueroa C. Results of a new telemedicine strategy in traumatology and orthopedics. Telemed e-Health. 2019;00:1–6.
•• Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19. J Bone Jt Surg Publish Ah. 2020:1–7 Demonstrates trends in tele-orthopaedics after COVID-19 pandemic. Makes an important description of virtual orthopedic examination.
Russell T, Jull G, Wootton R. Can the internet be used as a medium to evaluate knee angle? Man Ther. 2003;8:242–6.
Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25:451–9.
• Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21:1–15 Randomized controlled study evaluated 559 consultations, divided between intervention and control. It demonstrated teleconsultation is cost-effective from health sector perspective.
Atanda A, Pelton M, Fabricant PD, Tucker A, Shah SA, Slamon N. Telemedicine utilisation in a paediatric sports medicine practice: decreased cost and wait times with increased satisfaction. J ISAKOS Jt Disord Orthop Sport Med. 2018;3:94–7.
Marsh J, Hoch JS, Bryant D, MacDonald SJ, Naudie D, McCalden R, et al. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Jt Surgery-American. 2014;96:1910–6.
Gilbert AW, Jaggi A, May CR. What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? A systematic review. Physiother (United Kingdom). 2018;104:178–86.
Thomas K, Burton D, Withrow L, Adkisson B. Impact of a preoperative education program via interactive telehealth network for rural patients having total joint replacement. Orthop Nurs. 2004;23:39–44.
Eichler S, Salzwedel A, Rabe S, Mueller S, Mayer F, Wochatz M, et al. The effectiveness of telerehabilitation as a supplement to rehabilitation in patients after total knee or hip replacement: randomized controlled trial. J Med Internet Res. 2019;21:1–12.
•• Abel KC, Baldwin K, Chuo J, Ganley T, Kim A, Wells L, et al. Can telemedicine be used for adolescent postoperative knee arthroscopy follow-up? JBJS J Orthop Physician Assist. 2017;5:1 350 patients aged 10-20 years , who underwent knee arthroscopy, were evaluated by teleconsultation. Authors describe how to assess range of motion, incision color and effusion size.
Bertani A, Launay F, Candoni P, Mathieu L, Rongieras F, Chauvin F. Teleconsultation in paediatric orthopaedics in Djibouti: evaluation of response performance. Orthop Traumatol Surg Res. 2012;98:803–7.
Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:469–76.
Groeneveld B, Dekkers T, Boon B, D’Olivo P. Challenges for design researchers in healthcare. Des Heal. 2018;2:305–26.
Roberts JP, Fisher TR, Trowbridge MJ, Bent C. A design thinking framework for healthcare management and innovation. Healthcare. 2016;4:11–4.
Preece J, Sharp H, Rogers Y (2019) Interaction design: beyond human-computer interaction, 5th ed. New York, NY.
Garrett JJ (2010) The elements of user experience: user-centered design for the web and beyond, 2nd ed. Berkeley, CA.
Reay SD, Collier G, Douglas R, Hayes N, Nakarada-Kordic I, Nair A, et al. Prototyping collaborative relationships between design and healthcare experts: mapping the patient journey. Des Heal. 2017;1:65–79.
Fatehi F, Smith AC, Maeder A, Wade V, Gray LC. How to formulate research questions and design studies for telehealth assessment and evaluation. J Telemed Telecare. 2017;23:759–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Noel Foni, Lauro Costa, Leandro Velloso, and Carlos Pedrotti declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Emerging Trends in Design for Musculoskeletal Medicine
Rights and permissions
About this article
Cite this article
Foni, N.O., Costa, L.A.V., Velloso, L.M.R. et al. Telemedicine: Is It a Tool for Orthopedics?. Curr Rev Musculoskelet Med 13, 797–801 (2020). https://doi.org/10.1007/s12178-020-09680-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-020-09680-6