Abstract
Purpose of Review
As immersive learning outside of the operating room is increasingly recognized as a valuable method of surgical training, virtual reality (VR) and augmented reality (AR) are increasingly utilized in orthopedic surgical training. This article reviews the evolving nature of these training tools and provides examples of their use and efficacy. The practical and ethical implications of incorporating this technology and its impact on both orthopedic surgeons and their patients are also discussed.
Recent Findings
Head-mounted displays (HMDs) represent a possible adjunct to surgical accuracy and education. While the hardware is advanced, there is still much work to be done in developing software that allows for seamless, reliable, useful integration into clinical practice and training.
Summary
Surgical training is changing: AR and VR will become mainstays of future training efforts. More evidence is needed to determine which training technology translates to improved clinical performance. Volatility within the HMD industry will likely delay advances in surgical training.





Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bass BL. Fundamental changes in general surgery residency training. Am Surg. 2007;73:109–13.
Ziv A, Small SD, Wolpe PR. Patient safety and simulation-based medical education. Med Teach. 2000;22:489–95.
Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am [Internet]. 2010;92:2643–52 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21084575.
Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: A systematic literature review. Clin Orthop Relat Res. Lippincott Williams and Wilkins; 2007. p. 35–41.
Gates EA. New surgical procedures: can our patients benefit while we learn? Am J Obstet Gynecol [Internet]. 1997;176:1293–8 discussion 1298–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9215187.
Grogan BF, Blair JA, Blease RE, Cho MS, Hsu JR. Exposure of the distal humerus using a triceps hemi-peel approach. Orthopedics [Internet]. 2014 [cited 2017 May 25];37:e455–9. Available from: http://www.healio.com/doiresolver?doi=10.3928/01477447-20140430-56
Bedigrew KM, Blair JA, Possley DR, Kirk KL, Hsu JR. Comparison of calcaneal exposure through the extensile lateral and sinus tarsi approaches. Foot Ankle Spec. 2018;11:142–7.
Beltran MJ, Blair JA, Huh J, Kirby JM, Hsu JR. Articular exposure with the swashbuckler versus a “mini- swashbuckler” approach. Injury. 2013;44:189–93.
Blair JA, Stinner DJ, Kirby JM, Gerlinger TL, Hsu JR. Quantification of femoral neck exposure through a minimally invasive Smith-Petersen approach. J Orthop Trauma. 2010;24:355–8.
Larsen CR, Soerensen JL, Grantcharov TP, Dalsgaard T, Schouenborg L, Ottosen C, et al. Effect of virtual reality training on laparoscopic surgery: randomised controlled trial. BMJ [Internet]. BMJ Publishing Group; 2009 [cited 2017 Jul 12];338:b1802. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19443914
Atesok K, MacDonald P, Leiter J, Dubberley J, Satava R, VanHeest A, et al. Orthopaedic education in the era of surgical simulation: still at the crawling stage. World J Orthop [Internet]. Baishideng Publishing Group Inc; 2017 [cited 2017 Jul 14];8:290–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28473955
Baker DK, Fryberger CT, Ponce BA. The emergence of augmented reality in orthopaedic surgery and education. Orthop J Harvard Med School. 2015;23:8–16.
Barsom EZ, Graafland M, Schijven MP. Systematic review on the effectiveness of augmented reality applications in medical training. Surg Endosc [Internet]. Springer; 2016 [cited 2017 Aug 30];30:4174–83. Available from: https://link.springer.com/content/pdf/10.1007%252Fs00464-016-4800-6.pdf
Ruikar DD, Ravindra HS, Santosh KC. A systematic review on orthopedic simulators for psycho-motor skill and surgical procedure training. J Med Syst [Internet]. 2018 [cited 2019 Nov 15];42:168. Available from. https://doi.org/10.1007/s10916-018-1019-1.
Hodgins JL, Veillette C. Arthroscopic proficiency: methods in evaluating competency. BMC Med Educ [Internet]. 2013; [cited 2017 Jul 11];13:61. Available from: http://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-13-61.
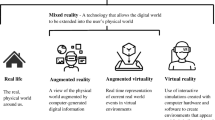
Milgram P, Takemura H, Utsumi A, Kishino F. Augmented reality: a class of displays on the reality-virtuality continuum [Internet]. 282 / SPIE. 1994. Available from: http://vered.rose.utoronto.ca
Hamacher A, Kim SJ, Cho ST, Pardeshi S, Lee SH, Eun S-J, et al. Application of virtual, augmented, and mixed reality to urology. Int Neurourol J [Internet]. Korean Continence Society; 2016 [cited 2018 Mar 24];20:172–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27706017
Khor WS, Baker B, Amin K, Chan A, Patel K, Wong J. Augmented and virtual reality in surgery-the digital surgical environment: applications, limitations and legal pitfalls. Ann Transl Med [Internet]. AME Publications; 2016 [cited 2017 Aug 29];4:454. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28090510
Wood L. Global Augmented Reality &; Virtual reality in healthcare industry worth USD 641 million by 2018 - analysis, technologies & Forecasts 2013–2018 - Key Vendors: Hologic Inc, Artificial Life Inc, Aruba Networks - Research and Markets | Business Wire [Internet]. Bus. Wire. 2016 [cited 2018 Apr 6]. Available from: https://www.businesswire.com/news/home/20160316005923/en/Global-Augmented-Reality-Virtual-Reality-Healthcare-Industry
Mixed Reality in Healthcare Market by Value, Revenue, Segments, Mega trends, Prominent Players and Outlook to 2024 - Reuters [Internet]. [cited 2019 Nov 15]. Available from: https://www.reuters.com/brandfeatures/venture-capital/article?id=144434
Bartlett JD, Lawrence JE, Stewart ME, Nakano N, Khanduja V. Does virtual reality simulation have a role in training trauma and orthopaedic surgeons? Bone Jt. J. Br Editorial Society of Bone and Joint Surgery; 2018. p. 559–65.
Tulipan J, Miller A, Park AG, Labrum JT, Ilyas AM. Touch surgery: analysis and assessment of validity of a hand surgery simulation “app.” Hand. SAGE Publications Inc.; 2018;
Sugand K, Mawkin M, Gupte C. Training effect of using Touch SurgeryTM for intramedullary femoral nailing. Injury Elsevier Ltd. 2016;47:448–52.
Moro C, Štromberga Z, Raikos A, Stirling A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ. John Wiley and Sons Inc. 2017;10:549–59.
Luciano CJ, Banerjee PP, Bellotte B, Lemole GM, Oh M, Charbel FT, et al. Learning retention of thoracic pedicle screw placement using a high-resolution augmented reality simulator with haptic feedback 1.
Leong JJH, Leff DR, Das A, Aggarwal R, Reilly P, Atkinson HDE, et al. Validation of orthopaedic bench models for trauma surgery. J Bone Jt Surg [Br] [Internet]. 2008 [cited 2017 Jul 11];90:958–65. Available from: http://bjj.boneandjoint.org.uk.libproxy.lib.unc.edu/content/jbjsbr/90-B/7/958.full.pdf
Pollard TCB, Khan T, Price AJ, Gill HS, Glyn-Jones S, Rees JL. Simulated hip arthroscopy skills: learning curves with the lateral and supine patient positions. J Bone Jt Surgery-American Vol [Internet]. 2012 [cited 2017 Jul 12];94:e68–1–10. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00004623-201205160-00023
Homma Y, Mogami A, Baba T, Naito K, Watari T, Osamu O, et al. Is actual surgical experience reflected in virtual reality simulation surgery for a femoral neck fracture? Eur J Orthop Surg Traumatol [Internet]. 2019 [cited 2019 Nov 13];29:1429–34. Available from. https://doi.org/10.1007/s00590-019-02465-9.
Cho HS, Park YK, Gupta S, Yoon C, Han I, Kim H-S, et al. Augmented reality in bone tumour resection: an experimental study. Bone Joint Res [Internet]. British Editorial Society of Bone and Joint Surgery; 2017 [cited 2018 Mar 19];6:137–43. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28258117
Kalun P, Wagner N, Yan J, Nousiainen M, Sonnadara R. Surgical simulation training in orthopedics: current insights. Adv Med Educ Pract. Dove Medical Press Ltd. 2018;9:125–31.
Mayne IP, Brydges R, Moktar J, Murnaghan ML. Development and assessment of a distal radial fracture model as a clinical teaching tool. J BONE Jt Surg [Internet]. 2016 [cited 2017 Jul 14];98:410–6. Available from: http://insights.ovid.com/crossref?an=00004623-201603020-00010
Goff BA, Lentz GM, Lee D, Fenner D, Morris J, Mandel LS. Development of a bench station objective structured assessment of technical skills. Obstet Gynecol [Internet]. 2001 [cited 2017 Jul 12];98:412–6. Available from: http://ac.els-cdn.com/S0029784401014739/1-s2.0-S0029784401014739-main.pdf?_tid=0614599c-671d-11e7-87f7-00000aab0f6b&acdnat=1499876186_1231ab1b1c7ad1abed53d1909841acaa
Rose K, Pedowitz R. Fundamental arthroscopic skill differentiation with virtual reality simulation. Arthrosc J Arthrosc Relat Surg [Internet]. 2015 [cited 2018 Mar 19];31:299–305. Available from: https://ac-els-cdn-com.libproxy.lib.unc.edu/S0749806314007154/1-s2.0-S0749806314007154-main.pdf?_tid=0258fdc6-d6ae-4cce-b212-fb6e0a12f604&acdnat=1521482765_68d74cd652aad08786da5570b17dc582
Moktar J, Popkin CA, Howard A, Murnaghan ML. Development of a cast application simulator and evaluation of objective measures of performance. J Bone Jt Surg - Am Vol [Internet]. 2014 [cited 2017 Jul 11];96:e76.1-e76.6. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00004623-201405070-00017
Dunn JC, Belmont PJ, Lanzi J, Martin K, Bader J, Owens B, et al. Arthroscopic shoulder surgical simulation training curriculum: transfer reliability and maintenance of skill over time. J Surg Educ [Internet]. 2015;72:1118–23 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26298520.
Waterman BR, Martin KD, Cameron KL, Owens BD, Belmont PJ. Simulation training improves surgical proficiency and safety during diagnostic shoulder arthroscopy performed by residents. Orthopedics [Internet]. 2016;39:e479–85 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27135460.
Cannon WD, Garrett WE, Hunter RE, Sweeney HJ, Eckhoff DG, Nicandri GT, et al. Improving residency training in arthroscopic knee surgery with use of a virtual-reality simulator. A randomized blinded study. J Bone Joint Surg Am [Internet]. 2014;96:1798–806 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27135460.
Howells NR, Gill HS, Carr AJ, Price AJ, Rees JL. Transferring simulated arthroscopic skills to the operating theatre a randomised blinded study. J Bone Jt Surg [Br] [Internet]. 2008 [cited 2017 Jul 12];90:494–9. Available from: http://bjj.boneandjoint.org.uk.libproxy.lib.unc.edu/content/jbjsbr/90-B/4/494.full.pdf
Tillander B, Ledin T, Nordqvist P, Skarman E, Wahlström O. A virtual reality trauma simulator. Med Teach. 2004;26:189–91.
Blyth P, Stott NS, Anderson IA. Virtual reality assessment of technical skill using the Bonedoc DHS simulator. Injury. 2008;39:1127–33.
Vankipuram M, Kahol K, McLaren A, Panchanathan S. A virtual reality simulator for orthopedic basic skills: a design and validation study. J Biomed Inform [Internet]. Elsevier Inc.; 2010;43:661–8. Available from: https://doi.org/10.1016/j.jbi.2010.05.016
Froelich JM, Milbrandt JC, Novicoff WM, Saleh KJ, Allan DG. Surgical simulators and hip fractures: a role in residency training? J Surg Educ [Internet]. Elsevier Inc.; 2011;68:298–302. Available from: https://doi.org/10.1016/j.jsurg.2011.02.011
LeBlanc J, Hutchison C, Hu Y, Donnon T. Topics in training: a comparison of orthopaedic resident performance on surgical fixation of an ulnar fracture using virtual reality and synthetic models. J Bone Jt Surg - Ser A. 2013;95:1–6.
Akhtar K, Sugand K, Sperrin M, Cobb J, Standfield N, Gupte C. Training safer orthopedic surgeons. Acta Orthop. 2015;86:616–21.
Ruder JA, Turvey B, Hsu JR, Scannell BP. Effectiveness of a low-cost drilling module in orthopaedic surgical simulation. [cited 2017 Aug 2]; Available from: https://www-clinicalkey-com.libproxy.lib.unc.edu/service/content/pdf/watermarked/1-s2.0-S193172041630229X.pdf?locale=en_US
• Buck JS, Wally MK, Patt JC, Scannell B, Seymour RB, Hsu JR. Teaching cortical-screw tightening: a simple, affordable, torque-directed training protocol improves resident performance. J Bone Joint Surg Am. NLM (Medline). 2019:101, e51. The authors developed a low-fidelity training protocol to teach residents how to insert cortical screws without stripping the screw-bone interface. Immediately following training, all residents demonstrated improved ability to insert screws without stripping, but at 3-month follow-up, only senior residents retained the benefits of the training protocol.
Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, et al. Assessment of technical skills transfer from the bench training model to the human model. [cited 2017 Jul 13]; Available from: http://ac.els-cdn.com/S0002961098003274/1-s2.0-S0002961098003274-main.pdf?_tid=30e2008c-6800-11e7-b10d-00000aacb361&acdnat=1499973749_2439c3aa32a8900be2a507214ef3a8e6
Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, et al. The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg [Internet]. 2004;240:374–81 Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1356416&tool=pmcentrez&rendertype=abstract.
Blackwell M, Morgan F, Di Gioia AM. Augmented reality and its future in orthopaedics. Clin Orthop Relat Res. Lippincott Williams and Wilkins; 1998. p. 111–22.
Ponce BA, Jennings JK, Clay TB, May MB, Huisingh C, Sheppard ED, et al. J Bone Jt Surg - Am Vol. Journal of Bone and Joint Surgery Inc. 2014;96:e84(1).
Davis MC, Can DD, Pindrik J, Rocque BG, Johnston JM. Virtual interactive presence in global surgical education: international collaboration through augmented reality. World Neurosurg [Internet]. NIH Public Access; 2016 [cited 2018 Mar 19];86:103–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26342783
Shenai MB, Dillavou M, Shum C, Ross D, Tubbs RS, Shih A, et al. Virtual interactive presence and augmented reality (VIPAR) for remote surgical assistance. Neurosurgery [Internet]. 2011 [cited 2017 Aug 31];68:ons200–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21304333
Rahman R, Wood M. Head-mounted display use in surgery: a systematic review. 2019 [cited 2019 Nov 12]; Available from: https://doi.org/10.1177/1553350619871787
Ewurum CH, Guo Y, Pagnha S, Feng Z, Luo X. Surgical navigation in orthopedics: workflow and system review. Adv Exp Med Biol. Springer New York LLC; 2018. p. 47–63.
Tepper OM, Rudy HL, Lefkowitz A, Weimer KA, Marks SM, Stern CS, et al. Mixed reality with HoloLens. Plast Reconstr Surg [Internet]. 2017 [cited 2018 Mar 16];140:1066–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29068946
•• Yong M, Pauwels J, Kozak FK, Chadha NK. Application of augmented reality to surgical practice: a pilot study using the ODG R-7 Smartglasses. Clin Otolaryngol [Internet]. 2019 [cited 2019 Nov 12]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/31610087. Remote attending surgeons ODG R7 HMD to guide trainees through simulated temporal bone dissection. Uploaded imaging and annotations to trainees field of view. Found issues with connectivity, lack of eye protection, no built-in headlight, angle of camera didn't align with user.
Albrecht U-V, von Jan U, Kuebler J, Zoeller C, Lacher M, Muensterer OJ, et al. Google Glass for documentation of medical findings: evaluation in forensic medicine. J Med Internet Res [Internet]. 2014 [cited 2017 Aug 29];16:e53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24521935
Armstrong DG, Rankin TM, Giovinco NA, Mills JL, Matsuoka Y. A heads-up display for diabetic limb salvage surgery: a view through the Google looking glass. J Diabetes Sci Technol [Internet]. Diabetes Technology Society; 2014 [cited 2017 Aug 29];8:951–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24876445
Knight HM, Gajendragadkar PR, Bokhari A. Wearable technology: using Google Glass as a teaching tool. BMJ Case Rep [Internet]. BMJ Publishing Group; 2015 [cited 2017 Aug 31];2015. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25969411
Wei NJ, Dougherty B, Myers A, Badawy SM. Using Google glass in surgical settings: systematic review. JMIR mHealth uHealth [Internet]. JMIR Publications Inc.; 2018 [cited 2018 Mar 30];6:e54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29510969
Qian L, Barthel A, Johnson A, Osgood G, Kazanzides P, Navab N, et al. Comparison of optical see-through head-mounted displays for surgical interventions with object-anchored 2D-display. Int J Comput Assist Radiol Surg [Internet]. 2017 [cited 2017 Aug 31];12:901–10. Available from: https://link-springer-com.libproxy.lib.unc.edu/content/pdf/10.1007%2Fs11548-017-1564-y.pdf
Peden RG, Mercer R, Tatham AJ. The use of head-mounted display eyeglasses for teaching surgical skills: a prospective randomised study. 2016 [cited 2017 Aug 31]; Available from: https://www-clinicalkey-com.libproxy.lib.unc.edu/service/content/pdf/watermarked/1-s2.0-S1743919116308500.pdf?locale=en_US
An AR glasses pioneer collapses | TechCrunch [Internet]. [cited 2019 Nov 17]. Available from: https://techcrunch.com/2019/01/10/an-ar-glasses-pioneer-collapses/
Mahmood F, Mahmood E, Dorfman RG, Mitchell J, Mahmood FU, Jones SB, et al. Augmented reality and ultrasound education: initial experience. J Cardiothorac Vasc Anesth [Internet]. Elsevier Inc.; 2018;1–5. Available from: https://doi.org/10.1053/j.jvca.2017.12.006
Input Methods Overview | Magic Leap [Internet]. [cited 2019 Nov 17]. Available from: https://creator.magicleap.com/learn/guides/design-input-methods-overview
Magic Leap sees a bright future in AR healthcare [Internet]. [cited 2019 Nov 17]. Available from: https://www.fastcompany.com/90398573/magic-leap-sees-a-bright-future-in-ar-health-care
Pelargos PE, Nagasawa DT, Lagman C, Tenn S, Demos J V, Lee SJ, et al. Utilizing virtual and augmented reality for educational and clinical enhancements in neurosurgery. J Clin Neurosci [Internet]. 2017 [cited 2018 Mar 16];35:1–4. Available from: https://www-clinicalkey-com.libproxy.lib.unc.edu/service/content/pdf/watermarked/1-s2.0-S0967586816303162.pdf?locale=en_US
•• Elmi-Terander A, Burström G, Nachabe R, Skulason H, Pedersen K, Fagerlund M et al. Pedicle screw placement using augmented reality surgical navigation with intraoperative 3D imaging: a first in-human prospective cohort study. Spine (Phila Pa 1976). NLM (Medline); 2019;44:517–25. AR assisted in vivo pedicle screw placement. Found 6% of screws breeched 2-4mm. Used display screen monitor system and noninvasive patient monitoring including C-arm mounted 3D cone-beam CT. Found low intraoperative screw revision rate (1.2%).
• Gibby JT, Swenson SA, Cvetko S, Rao Raj, Javan R, Rao R. Head-mounted display augmented reality to guide pedicle screw placement utilizing computed tomography. Int J Comput Assist Radiol Surg [Internet]. 2019 [cited 2019 Nov 12];14:525–35. Available from: https://doi.org/10.1007/s11548-018-1814-7. Bench model using Hololens to give superimposed CT-based image guidance during pedicle screw placement. Found 97% accuracy.
Müller F, Roner S, Liebmann F, Spirig JM, Furnstahl P, Farshad M. Augmented reality navigation for spinal pedicle screw instrumentation using intraoperative 3D imaging. Spine J [Internet]. 2019 [cited 2019 Nov 12]; Available from. https://doi.org/10.1016/j.spinee.2019.10.012.
Edström E, Burström G, Omar A, Nachabe R, Söderman M, Persson O, et al. Augmented reality surgical navigation in spine surgery to minimize staff radiation exposure. Spine (Phila Pa 1976). Ovid Technologies (Wolters Kluwer Health); 2019;1.
Kosterhon M, Gutenberg A, Kantelhardt SR, Archavlis E, Giese A. Navigation and image injection for control of bone removal and osteotomy planes in spine surgery. Oper Neurosurg (Hagerstown, Md) [Internet]. 2017;13:297–304 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28927210.
Cho HS, Oh JH, Han I, Kim HS. The outcomes of navigation-assisted bone tumour surgery: minimum three-year follow-up. J Bone Jt Surg - Ser B. 2012;94(B):1414–20.
Choi H, Park Y, Lee S, Ha H, Kim S, Cho HS, et al. A portable surgical navigation device to display resection planes for bone tumor surgery. Minim Invasive Ther Allied Technol. Taylor and Francis Ltd. 2017;26:144–50.
Cho HS, Park MS, Gupta S, Han I, Kim HS, Choi H, et al. Can augmented reality be helpful in pelvic bone cancer surgery? An in vitro study. Clin Orthop Relat Res. Lippincott Williams and Wilkins. 2018;476:1719–25.
Laitinen MK, Parry MC, Albergo JI, Grimer RJ, Jeys LM. Is computer navigation when used in the surgery of iliosacral pelvic bone tumours safer for the patient? Bone Jt J. 2017;99-B:261–6.
Gerrand C. CORR Insights®. Clin Orthop Relat Res. Ovid Technologies (Wolters Kluwer Health). 2018;476:1726–7.
• van Duren BH, Sugand K, Wescott R, Carrington R, Hart A. Augmented reality fluoroscopy simulation of the guide-wire insertion in DHS surgery: a proof of concept study. Med Eng Phys. Elsevier Ltd; 2018;55:52–9. Augmented and VR combo trainer for inserting guidewires with optical tracking and fake fluoroscopic image overlay using sawbones model. Found accuracy to within 2mm.
Hiranaka T, Fujishiro T, Hida Y, Shibata Y, Tsubosaka M, Nakanishi Y, et al. Augmented reality: the use of the picolinker smart glasses improves wire insertion under fluoroscopy. World J Orthop. Baishideng Publishing Group Co. 2017;8:891–894.pdf.
Diotte B, Fallavollita P, Wang L, Weidert S, Euler E, Thaller P, et al. Multi-modal intra-operative navigation during distal locking of intramedullary nails. IEEE Trans Med Imaging. Institute of Electrical and Electronics Engineers Inc. 2015;34:487–95.
Ma L, Zhao Z, Zhang B, Jiang W, Fu L, Zhang X, et al. Three-dimensional augmented reality surgical navigation with hybrid optical and electromagnetic tracking for distal intramedullary nail interlocking. Int J Med Robot Comput Assist Surgvery. John Wiley and Sons Ltd; 2018;14.
Richter PH, Gebhard F, Dehner C, Scola A. Accuracy of computer-assisted iliosacral screw placement using a hybrid operating room. 2016 [cited 2018 Apr 5]; Available from: https://ac-els-cdn-com.libproxy.lib.unc.edu/S0020138315007457/1-s2.0-S0020138315007457-main.pdf?_tid=a69b6021-571c-4240-9dee-b21f037899e0&acdnat=1522947591_d38225497a120d41d0a0e43892726b48
Wang H, Wang F, Leong APY, Xu L, Chen X, Wang Q. Precision insertion of percutaneous sacroiliac screws using a novel augmented reality-based navigation system: a pilot study. Int Orthop Springer Verlag. 2016;40:1941–7.
Fallavollita P, Brand A, Wang L, Euler E, Thaller P, Navab N, et al. An augmented reality C-arm for intraoperative assessment of the mechanical axis: a preclinical study. Int J CARS [Internet]. 2016 [cited 2018 Mar 19];11:2111–7. Available from: https://link-springer-com.libproxy.lib.unc.edu/content/pdf/10.1007%2Fs11548-016-1426-z.pdf
Ogawa H, Hasegawa S, Tsukada S, Matsubara M. A pilot study of augmented reality technology applied to the acetabular cup placement during total hip arthroplasty. 2018 [cited 2018 Mar 16]; Available from: https://www-clinicalkey-com.libproxy.lib.unc.edu/service/content/pdf/watermarked/1-s2.0-S0883540318301050.pdf?locale=en_US
Fotouhi J, Alexander CP, Unberath M, Sing GT, Lee C, Fuerst B, et al. Plan in 2-D, execute in 3-D: an augmented reality solution for cup placement in total hip arthroplasty. Med Imag. 2018;5:21205.
• Logishetty K, Western L, Morgan R, Iranpour F, Cobb JP, Auvinet E. Can an augmented reality headset improve accuracy of acetabular cup orientation in simulated THA? A randomized trial. Clin Orthop Relat Res. Ovid Technologies (Wolters Kluwer Health); 2019;477:1190–9. Looked at accuracy differences in acetabular cup placement between novices trained by a surgeon vs. those trained with AR assistance with Hololens guidance. Found no differences in placement accuracy between groups.
•• Lei P-F, Su S-L, Kong L-Y, Wang C-G, Zhong D, Hu Y-H. Mixed Reality Combined with three-dimensional printing technology in total hip arthroplasty: an updated review with a preliminary case presentation. 2019; First example of using 3D printing, HMD, and anatomic referencing intraoperatively to perform Total Hip Arthroplasty. The authors developed a low-fidelity training protocol to teach residents how to insert cortical screws without stripping the screw-bone interface. Immediately following training, all residents demonstrated improved ability to insert screws without stripping, but at 3-month follow-up, only senior residents retained the benefits of the training protocol.
Guraya SY. Using telementoring and augmented reality in surgical specialties. J. Taibah Univ. Med. Sci. Elsevier B.V.; 2019. p. 101–2.
Kaylor J, Hooper V, Wilson A, Burkert R, Lyda M, Fletcher K, et al. Reliability testing of augmented reality glasses technology. J Wound, Ostomy Cont Nurs [Internet]. 2019 [cited 2019 Nov 12];1. Available from: http://insights.ovid.com/crossref?an=00152192-900000000-99717
Ponce BA, Brabston EW, Zu S, Watson SL, Baker D, Winn D, et al. Telemedicine with mobile devices and augmented reality for early postoperative care. 2016 38th Annu Int Conf IEEE Eng Med Biol Soc [Internet]. 2016;22031:4411–4. Available from: http://ieeexplore.ieee.org/document/7591705/
Ponce BA, Menendez ME, Oladeji LO, Fryberger CT, Dantuluri PK. Emerging technology in surgical education: combining real-time augmented reality and wearable computing devices. Orthopedics Slack Incorporated. 2014;37:751–7.
Lindeque BGP, Ponce BA, Menendez ME, Oladeji LO, Fryberger CT, Dantuluri PK. Emerging technology in surgical education: combining real-time augmented reality and wearable computing devices. Orthopedics [Internet]. 2014;37:751–7. Available from: http://www.healio.com/doiresolver?doi=10.3928/01477447-20141023-05
Dixon BJ, Daly MJ, Chan HHLL, Vescan A, Witterick IJ, Irish JC. Inattentional blindness increased with augmented reality surgical navigation. Am J Rhinol Allergy [Internet]. 2014;28:433–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25198032
Hughes-Hallett A, Mayer EK, Marcus HJ, Pratt P, Mason S, Darzi AW, et al. Inattention blindness in surgery. Surg Endosc Other Interv Tech [Internet]. 2015 [cited 2018 Mar 19];29:3184–9. Available from: https://link-springer-com.libproxy.lib.unc.edu/content/pdf/10.1007%2Fs00464-014-4051-3.pdf
Vávra P, Roman J, Zonča P, Ihnát P, Němec M, Kumar J, et al. Recent development of augmented reality in surgery: a review. J. Healthc. Eng. Hindawi Limited; 2017.
Antonini G, Stuflesser W, Crippa C, Touloupakis G. A distal-lock electromagnetic targeting device for intramedullary nailing: Suggestions and clinical experience. Chinese J Traumatol - English Ed Elsevier BV. 2016;19:358–61.
Veliceasa B, Bandac R, Popescu D, Puha B, Alexa O. Evaluation of TRIGEN SURESHOT® distal targeting system - a new electromagnetic computer-assisted guidance system. 2015 E-Health Bioeng Conf EHB 2015. Institute of Electrical and Electronics Engineers Inc.; 2016.
Elmi-Terander A, Skulason H, Soderman M, Racadio J, Homan R, Babic D, et al. Surgical navigation technology based on augmented reality and integrated 3D intraoperative imaging a spine cadaveric feasibility and accuracy study. Spine (Phila Pa 1976). 2016;41:E1303–11.
Funding
Dr. McKnight, Dr. Hsu, and Dr. Hwang received funding from the AOTrauma North America Fellows Research Support grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The other authors declare that they have no conflict of interest.
Joseph Hsu is a paid presenter or speaker for Smith & Nephew.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on The Use of Technology in Orthopaedic Surgery—Intraoperative and Post-Operative Management
Rights and permissions
About this article
Cite this article
McKnight, R.R., Pean, C.A., Buck, J.S. et al. Virtual Reality and Augmented Reality—Translating Surgical Training into Surgical Technique. Curr Rev Musculoskelet Med 13, 663–674 (2020). https://doi.org/10.1007/s12178-020-09667-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-020-09667-3