Abstract
Purpose of Review
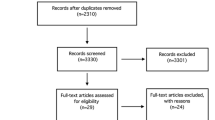
The purposes of this review are to (1) describe the anatomic and biomechanical rationale for high tibial osteotomy (HTO) in the setting of posterior cruciate ligament (PCL) deficiency, (2) review the indications for concomitant HTO and PCL reconstruction, (3) provide guidance for the clinical assessment of the patient with suspected PCL deficiency, and (4) summarize the key surgical steps necessary to attain the appropriate sagittal and coronal plane corrections.
Recent Findings
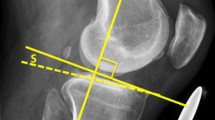
The preponderance of available biomechanical data pertaining to the PCL-deficient knee suggests that an increased proximal tibial slope limits posterior tibial translation under axial compressive loads. Moreover, recent clinical data has demonstrated that decreased proximal tibial slope may exacerbate residual anterior-posterior laxity and jeopardize the durability of PCL reconstruction. Thus, in the setting of PCL deficiency, an HTO that increases the posterior tibial slope may be advisable.
Summary
HTO may be an important treatment adjunct in the surgical management of PCL deficiency. In the setting of chronic injuries and varus malalignment, HTO should be considered in order to ensure a durable ligamentous reconstruction and forestall the progression of secondary osteoarthritis.





Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am. 1980;62(2):259–70.
Fukubayashi T, Torzilli PA, Sherman MF, Warren RF. An in vitro biomechanical evaluation of anterior-posterior motion of the knee. Tibial displacement, rotation, and torque. J Bone Joint Surg Am. 1982;64(2):258–64.
Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;106:216–31.
Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69(2):233–42.
Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988;70(1):88–97.
Race A, Amis AA. The mechanical properties of the two bundles of the human posterior cruciate ligament. J Biomech. 1994;27(1):13–24.
Race A, Amis AA. Loading of the two bundles of the posterior cruciate ligament: an analysis of bundle function in a-P drawer. J Biomech. 1996;29(7):873–9.
Li G, Gill TJ, DeFrate LE, Zayontz S, Glatt V, Zarins B. Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads—an in vitro experimental study. J Orthop Res. 2002;20(4):887–92. https://doi.org/10.1016/S0736-0266(01)00184-X.
Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Aroen A, et al. Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. 2013;41(12):2828–38. https://doi.org/10.1177/0363546513504287.
Gill TJ, DeFrate LE, Wang C, Carey CT, Zayontz S, Zarins B, et al. The biomechanical effect of posterior cruciate ligament reconstruction on knee joint function. Kinematic response to simulated muscle loads. Am J Sports Med. 2003;31(4):530–6. https://doi.org/10.1177/03635465030310040901.
Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995;11(5):526–9.
Aroen A, Sivertsen EA, Owesen C, Engebretsen L, Granan LP. An isolated rupture of the posterior cruciate ligament results in reduced preoperative knee function in comparison with an anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1017–22. https://doi.org/10.1007/s00167-012-2132-1.
Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45(3):462–9. https://doi.org/10.1249/MSS.0b013e318277acca.
Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93(19):1773–80. https://doi.org/10.2106/JBJS.J.01638.
Keller PM, Shelbourne KD, McCarroll JR, Rettig AC. Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med. 1993;21(1):132–6. https://doi.org/10.1177/036354659302100122.
Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41(7):1526–33. https://doi.org/10.1177/0363546513486771.
Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27(3):276–83. https://doi.org/10.1177/03635465990270030201.
Shelbourne KD, Muthukaruppan Y. Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy. 2005;21(4):457–61. https://doi.org/10.1016/j.arthro.2004.11.013.
LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43(12):3077–92. https://doi.org/10.1177/0363546515572770.
Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186–91. https://doi.org/10.1007/s00402-002-0471-y.
Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–8. https://doi.org/10.1016/j.knee.2006.01.005.
Sanders TL, Pareek A, Barrett IJ, Kremers HM, Bryan AJ, Stuart MJ, et al. Incidence and long-term follow-up of isolated posterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc. 2016;25:3017–23. https://doi.org/10.1007/s00167-016-4052-y.
Mariani PP, Adriani E, Santori N, Maresca G. Arthroscopic posterior cruciate ligament reconstruction with bone-tendon-bone patellar graft. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):239–44. https://doi.org/10.1007/s001670050057.
Aglietti P, Buzzi R, Lazzara D. Posterior cruciate ligament reconstruction with the quadriceps tendon in chronic injuries. Knee Surg Sports Traumatol Arthrosc. 2002;10(5):266–73. https://doi.org/10.1007/s00167-002-0288-9.
Chen CH, Chen WJ, Shih CH. Arthroscopic double-bundled posterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy. 2000;16(7):780–2. https://doi.org/10.1053/jars.2000.8020.
Chen CH, Chen WJ, Shih CH. Arthroscopic reconstruction of the posterior cruciate ligament: a comparison of quadriceps tendon autograft and quadruple hamstring tendon graft. Arthroscopy. 2002;18(6):603–12.
L'Insalata JC, Harner CD. Treatment of acute and chronic posterior cruciate ligament deficiency. New approaches. Am J Knee Surg. 1996;9(4):185–93.
Noyes FR, Barber-Westin SD. Posterior cruciate ligament allograft reconstruction with and without a ligament augmentation device. Arthroscopy. 1994;10(4):371–82.
Noyes FR, Barber-Westin SD. Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33(5):646–54. https://doi.org/10.1177/0363546504271210.
Matava MJ, Ellis E, Gruber B. Surgical treatment of posterior cruciate ligament tears: an evolving technique. J Am Acad Orthop Surg. 2009;17(7):435–46.
Song EK, Park HW, Ahn YS, Seon JK. Transtibial versus tibial inlay techniques for posterior cruciate ligament reconstruction: long-term follow-up study. Am J Sports Med. 2014;42(12):2964–71. https://doi.org/10.1177/0363546514550982.
• Petrigliano FA, Suero EM, Voos JE, Pearle AD, Allen AA. The effect of proximal tibial slope on dynamic stability testing of the posterior cruciate ligament- and posterolateral corner-deficient knee. Am J Sports Med. 2012;40(6):1322–8. https://doi.org/10.1177/0363546512439180. This biomechanical study demonstrated that an increase in the posterior tibial slope may improve sagittal stability in the PCL/PLC- deficient knee. Additionally, this publication showed that a diminished posterior slope may have greater multiplanar instability.
Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124(9):575–84. https://doi.org/10.1007/s00402-004-0728-8.
• Gwinner C, Weiler A, Roider M, Schaefer FM, Jung TM. Tibial slope strongly influences knee stability after posterior cruciate ligament reconstruction: a prospective 5- to 15-year follow-up. Am J Sports Med. 2017;45(2):355–61. https://doi.org/10.1177/0363546516666354. This recent clinical study, in a 5 to 15-year follow-up, showed that a decreased tibial slope is associated with increased posterior laxity after PCL reconstruction. Therefore, surgeons may consider to increase the tibial slope when performing an osteotomy in PCL-deficient patients to prevent residual posterior laxity.
Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report. J Bone Joint Surg Am. 1965;47:984–90.
Savarese E, Bisicchia S, Romeo R, Amendola A. Role of high tibial osteotomy in chronic injuries of posterior cruciate ligament and posterolateral corner. J Orthop Traumatol. 2011;12(1):1–17. https://doi.org/10.1007/s10195-010-0120-0.
Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10(3):585–608.
Ahmad CS, Cohen ZA, Levine WN, Gardner TR, Ateshian GA, Mow VC. Codominance of the individual posterior cruciate ligament bundles. An analysis of bundle lengths and orientation. Am J Sports Med. 2003;31(2):221–5. https://doi.org/10.1177/03635465030310021101.
Van Dommelen BA, Fowler PJ. Anatomy of the posterior cruciate ligament. A review. Am J Sports Med. 1989;17(1):24–9. https://doi.org/10.1177/036354658901700104.
Amis AA, Gupte CM, Bull AM, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):257–63. https://doi.org/10.1007/s00167-005-0686-x.
Takahashi M, Matsubara T, Doi M, Suzuki D, Nagano A. Anatomical study of the femoral and tibial insertions of the anterolateral and posteromedial bundles of human posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1055–9. https://doi.org/10.1007/s00167-006-0192-9.
Kennedy JC, Hawkins RJ, Willis RB, Danylchuck KD. Tension studies of human knee ligaments. Yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone Joint Surg Am. 1976;58(3):350–5.
Marinozzi G, Pappalardo S, Steindler R. Human knee ligaments: mechanical tests and ultrastructural observations. Ital J Orthop Traumatol. 1983;9(2):231–40.
Trent PS, Walker PS, Wolf B. Ligament length patterns, strength, and rotational axes of the knee joint. Clin Orthop Relat Res 1976(117):263–70
Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94(21):1936–45. https://doi.org/10.2106/JBJS.K.01710.
Lopes OV Jr, Ferretti M, Shen W, Ekdahl M, Smolinski P, Fu FH. Topography of the femoral attachment of the posterior cruciate ligament. J Bone Joint Surg Am. 2008;90(2):249–55. https://doi.org/10.2106/JBJS.G.00448.
Noyes FR, Goebel SX, West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med. 2005;33(3):378–87. https://doi.org/10.1177/0363546504269034.
Brazier J, Migaud H, Gougeon F, Cotten A, Fontaine C, Duquennoy A. Evaluation of methods for radiographic measurement of the tibial slope. A study of 83 healthy knees. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(3):195–200.
Chiu KY, Zhang SD, Zhang GH. Posterior slope of tibial plateau in Chinese. J Arthroplast. 2000;15(2):224–7.
Genin P, Weill G, Julliard R. The tibial slope. Proposal for a measurement method. J Radiol. 1993;74(1):27–33.
Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg (Br). 1994;76(5):745–9.
Matsuda S, Miura H, Nagamine R, Urabe K, Ikenoue T, Okazaki K, et al. Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999;12(3):165–8.
Noyes FR, Dunworth LA, Andriacchi TP, Andrews M, Hewett TE. Knee hyperextension gait abnormalities in unstable knees. Recognition and preoperative gait retraining. Am J Sports Med. 1996;24(1):35–45. https://doi.org/10.1177/036354659602400107.
Skyhar MJ, Warren RF, Ortiz GJ, Schwartz E, Otis JC. The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. J Bone Joint Surg Am. 1993;75(5):694–9.
Ramaniraka NA, Terrier A, Theumann N, Siegrist O. Effects of the posterior cruciate ligament reconstruction on the biomechanics of the knee joint: a finite element analysis. Clin Biomech (Bristol, Avon). 2005;20(4):434–42. https://doi.org/10.1016/j.clinbiomech.2004.11.014.
Lubowitz JH, Bernardini BJ, Reid JB 3rd. Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med. 2008;36(3):577–94. https://doi.org/10.1177/0363546507312641.
Daniel DM, Stone ML, Barnett P, Sachs R. Use of the quadriceps active test to diagnose posterior cruciate-ligament disruption and measure posterior laxity of the knee. J Bone Joint Surg Am. 1988;70(3):386–91.
Clancy WG Jr, Shelbourne KD, Zoellner GB, Keene JS, Reider B, Rosenberg TD. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J Bone Joint Surg Am. 1983;65(3):310–22.
Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745–9.
Moore TM, Harvey JP Jr. Roentgenographic measurement of tibial-plateau depression due to fracture. J Bone Joint Surg Am. 1974;56(1):155–60.
Cullu E, Aydogdu S, Alparslan B, Sur H. Tibial slope changes following dome-type high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2005;13(1):38–43. https://doi.org/10.1007/s00167-004-0501-0.
Sekiya JK, Whiddon DR, Zehms CT, Miller MD. A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries. Evaluation of isolated and combined deficiency. J Bone Joint Surg Am. 2008;90(8):1621–7. https://doi.org/10.2106/jbjs.g.01365.
Mariani PP, Margheritini F, Christel P, Bellelli A. Evaluation of posterior cruciate ligament healing: a study using magnetic resonance imaging and stress radiography. Arthroscopy. 2005;21(11):1354–61. https://doi.org/10.1016/j.arthro.2005.07.028.
Rodriguez W Jr, Vinson EN, Helms CA, Toth AP. MRI appearance of posterior cruciate ligament tears. AJR Am J Roentgenol. 2008;191(4):1031–W159. https://doi.org/10.2214/ajr.07.2921.
DePhillipo NN, Cinque ME, Godin JA, Moatshe G, Chahla J, LaPrade RF. Posterior tibial translation measurements on magnetic resonance imaging improve diagnostic sensitivity for chronic posterior cruciate ligament injuries and graft tears. Am J Sports Med. 2017;46:341–7. https://doi.org/10.1177/0363546517734201.
Tewes DP, Fritts HM, Fields RD, Quick DC, Buss DD. Chronically injured posterior cruciate ligament: magnetic resonance imaging. Clin Orthop Relat Res. 1997;335:224–32.
LaPrade RF, Gilbert TJ, Bollom TS, Wentorf F, Chaljub G. The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am J Sports Med. 2000;28(2):191–9. https://doi.org/10.1177/03635465000280020901.
Lee SH, Jung YB, Lee HJ, Jung HJ, Kim SH. Revision posterior cruciate ligament reconstruction using a modified tibial-inlay double-bundle technique. J Bone Joint Surg Am. 2012;94(6):516–22. https://doi.org/10.2106/JBJS.K.00030.
• Tischer T, Paul J, Pape D, Hirschmann MT, Imhoff AB, Hinterwimmer S et al. The impact of sseous malalignment and realignment procedures in knee ligament surgery: a systematic review of the clinical evidence. Orthop J Sports Med. 2017;5(3) https://doi.org/10.1177/2325967117697287. This systematic review summarized the current literature regarding the impact of osseous malalignment and realigment procedures in knee ligament surgery. Concerning cases of chronic PCL and/or PCL instability, the study demonstrated that osseous correction of the varus alignment may reduce the failure rate, and is often the first step in treatment.
Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32(1):60–70. https://doi.org/10.1177/0363546503258907.
Noyes FR, Barber-Westin SD. Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med. 1996;24(4):415–26. https://doi.org/10.1177/036354659602400404.
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–82. https://doi.org/10.1177/0363546503258880.
Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35(9):1443–9. https://doi.org/10.1177/0363546507304665.
Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints—part I: tibial surface of the knee. J Biomech Eng. 1983;105(3):216–25.
Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Med. 1998;25(3):149–55.
LaPrade RF, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res. 2002;402:110–21.
Strobel MJ, Weiler A, Schulz MS, Russe K, Eichhorn HJ. Arthroscopic evaluation of articular cartilage lesions in posterior-cruciate-ligament-deficient knees. Arthroscopy. 2003;19(3):262–8. https://doi.org/10.1053/jars.2003.50037.
Li G, Papannagari R, Li M, Bingham J, Nha KW, Allred D, et al. Effect of posterior cruciate ligament deficiency on in vivo translation and rotation of the knee during weight bearing flexion. Am J Sports Med. 2008;36(3):474–9. https://doi.org/10.1177/0363546507310075.
Goyal K, Tashman S, Wang JH, Li K, Zhang X, Harner C. In vivo analysis of the isolated posterior cruciate ligament-deficient knee during functional activities. Am J Sports Med. 2012;40(4):777–85. https://doi.org/10.1177/0363546511435783.
Noyes FR, Barber SD, Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees. A two- to seven-year follow-up study. Am J Sports Med. 1993;21(1):2–12. https://doi.org/10.1177/036354659302100102.
Badhe NP, Forster IW. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc. 2002;10(1):38–43. https://doi.org/10.1007/s001670100244.
Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med. 2007;35(11):1844–50. https://doi.org/10.1177/0363546507304717.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on PCL Update
Rights and permissions
About this article
Cite this article
Novaretti, J.V., Sheean, A.J., Lian, J. et al. The Role of Osteotomy for the Treatment of PCL Injuries. Curr Rev Musculoskelet Med 11, 298–306 (2018). https://doi.org/10.1007/s12178-018-9488-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-018-9488-x