Abstract
Purpose of Review
Preimplantation genetic testing for monogenic conditions (PGT-M) is an increasingly utilized reproductive technology for patients with inherited heart disease (IHD). In this article, we provide an overview of the PGT-M process, including current guidance about its use, and review recent data about the perspectives and experiences of patients considering the use of PGT-M.
Recent Findings
PGT-M is used for a variety of IHDs; however, there is evidence that providers do not consistently raise this topic with patients, which may be due to a lack of knowledge about PGT-M. Regardless of the condition, patients report similar motivations for using PGT-M, such as the desire for a healthy child and the wish to save offspring from suffering. Patients make individualized decisions that are influenced by their lived experience with the diagnosis, a sense of responsibility to prevent disease transmission and other personal and logistical considerations. The PGT-M process can be challenging and each patient requires comprehensive information and support throughout.
Summary
PGT-M is a complex multi-step process whereby individual decision-making is influenced by various intrinsic and extrinsic factors. Adequate information and support are necessary for individual decision-making and expectation-setting. This is best accomplished by a multidisciplinary collaboration including cardiology, genetics, reproductive endocrinologists, and obstetric providers.


Similar content being viewed by others
Abbreviations
- ART:
-
Assisted reproductive technology
- CV:
-
Cardiovascular
- GC:
-
Genetic counseling
- GT:
-
Genetic testing
- IHD:
-
Inherited heart disease
- IVF:
-
In vitro fertilization
- PGT:
-
Preimplantation genetic testing
- PGT-A:
-
PGT for aneuploidy
- PGT-SR:
-
PGT for structural rearrangements
- PGT-M:
-
PGT for monogenic disorders
- SCD:
-
Sudden cardiac death
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Musunuru K, Hershberger RE, Day SM, Klinedinst NJ, Landstrom AP, Parikh VN, et al. Genetic testing for inherited cardiovascular diseases: a scientific statement from the American Heart Association. Circ Genom Precis Med. 2020;13(4):e000067.
Stiles MK, Wilde AAM, Abrams DJ, Ackerman MJ, Albert CM, Behr ER, et al. 2020 APHRS/HRS expert consensus statement on the investigation of decedents with sudden unexplained death and patients with sudden cardiac arrest, and of their families. Heart Rhythm. 2021;18(1):e1–50.
Wilde AAM, Semsarian C, Márquez MF, Shamloo AS, Ackerman MJ, Ashley EA, et al. European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) Expert consensus statement on the state of genetic testing for cardiac diseases. EP Europace. 2022;24(8):1307–67.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, De Mouzon J, Sokol R, Rienzi L, Sunde A, Schmidt L, Cooke ID, Simpson JL. The international glossary on infertility and fertility care, 2017. Fertil Steril. 2017;108(3):393–406.
ACOG Committee Opinion. Preimplantation genetic testing, Number 799. Obstet Gynecol. 2020;135(3):e133–7.
De Rycke M, Berckmoes V. Preimplantation genetic testing for monogenic disorders. Genes. 2020;11(8):871.
Kuliev A, Pakhalchuk T, Prokhorovich M, Rechitsky S. Preimplantation genetic testing for inherited predisposition to cardiac disease. Ann Heart. 2021;5(1). https://scholars.direct/Articles/heart/ahe-5-019.php?jid=heart. Kuliev et al. discuss outcomes of PGT-M cycles for inherited cardiac diseases. 109 cycles resulted in 54 liveborn children without the variant. The most common indication for PGT-M in this cohort was hypertrophic cardiomyopathy, with variants in MYBPC3 being the most prevalent. The article discusses the increasing usage of PGT-M for inherited cardiac diseases to prevent adverse outcomes like premature sudden death in offspring.
Daar J, Benward J, Collins L, Davis J, Davis O, Francis L, et al. Use of preimplantation genetic testing for monogenic defects (PGT-M) for adult-onset conditions: an Ethics Committee opinion. Fertil Steril. 2018;109(6):989–92.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Penzias A, Azziz R, Bendikson K, Cedars M, Falcone T, Hansen K, Hill M, Jindal S, Kalra S, Mersereau J, Racowsky C. Fertility evaluation of infertile women: a committee opinion. Fertil Steril. 2021;116(5):1255–65.
ESHRE PGT Consortium Steering Committee, Carvalho F, Coonen E, Goossens V, Kokkali G, Rubio C, et al. ESHRE PGT Consortium good practice recommendations for the organisation of PGT. Hum Reprod Open. 2020;2020(3):hoaa021.
Gurevich R. Verywell Family. 2021 PGT-M and PGT-A screening to reduce the risk of passing genetic diseases. https://www.verywellfamily.com/pgd-and-pgs-genetic-screening-before-ivf-4151705
Mathiesen A, Roy K. In: Baty B, editor. Foundations of perinatal genetic counseling : a guide for counselors. Oxford; New York: Oxford University Press; 2018. p. 289.
ESHRE PGT-M Working Group, Carvalho F, Moutou C, Dimitriadou E, Dreesen J, Giménez C, et al. ESHRE PGT Consortium good practice recommendations for the detection of monogenic disorders†. Human Reprod Open. 2020;2020(3):hoaa018.
Scott RT, Upham KM, Forman EJ, Zhao T, Treff NR. Cleavage-stage biopsy significantly impairs human embryonic implantation potential while blastocyst biopsy does not: a randomized and paired clinical trial. Fertil Steril. 2013;100(3):624–30.
Goisis A, Remes H, Martikainen P, Klemetti R, Myrskylä M. Medically assisted reproduction and birth outcomes: a within-family analysis using Finnish population registers. Lancet. 2019;393(10177):1225–32.
Hwang SS, Dukhovny D, Gopal D, Cabral H, Missmer S, Diop H, et al. Health of infants after ART-treated, subfertile, and fertile deliveries. Pediatrics. 2018;142(2):e20174069.
Liberman RF, Getz KD, Heinke D, Luke B, Stern JE, Declercq ER, et al. Assisted reproductive technology and birth defects: effects of subfertility and multiple births. Birth Defects Res. 2017;109(14):1144–53.
Khorshid A, Boyd ALH, Behr B, Zhao Q, Alvero R, Bavan B. Cost-effectiveness of IVF with PGT-M/A to prevent transmission of spinal muscular atrophy in offspring of carrier couples. J Assist Reprod Genet. 2023;40:793–801.
Lipton JH, Zargar M, Warner E, Greenblatt EE, Lee E, Chan KKW, et al. Cost effectiveness of in vitro fertilisation and preimplantation genetic testing to prevent transmission of BRCA1/2 mutations. Hum Reprod. 2020;35(2):434–45.
Bunnell ME, Dobson LJ, Lanes A, Ginsburg ES. Use of preimplantation genetic testing for monogenic disorders and subsequent prenatal care and diagnostic testing. Prenat Diagn. 2022;42(8):1022–30.
Rechitsky S, Kuliev A. Preimplantation genetic testing (PGT) for non-traditional indications. Reprod BioMed Online. 2019;38:e3.
Tester DJ, Ackerman MJ. Genetic testing for potentially lethal, highly treatable inherited cardiomyopathies/channelopathies in clinical practice. Circulation. 2011;123(9):1021–37.
Bayefsky M. Who should regulate preimplantation genetic diagnosis in the United States? AMA J Ethics. 2018;20(12):E1160–7.
Mital S, Musunuru K, Garg V, Russell MW, Lanfear DE, Gupta RM, et al. Enhancing literacy in cardiovascular genetics: a scientific statement from the American Heart Association. Circ Cardiovasc Genet. 2016;9(5):448–67.
Capelouto S, Evans M, Shannon J, Jetelina K, Bukulmez O, Carr B. Specialist physicians’ referral behavior regarding preimplantation genetic testing for single-gene disorders: is there room to grow? F S Rep. 2021;2(2):215–23.
Klitzman R. Challenges, Dilemmas and factors involved in PGD decision-making: providers’ and patients’ views, experiences and decisions. J Genet Couns. 2018;27(4):909–19.
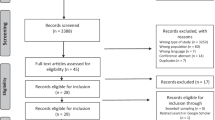
Hughes T, Bracewell-Milnes T, Saso S, Jones BP, Almeida PA, Maclaren K, et al. A review on the motivations, decision-making factors, attitudes and experiences of couples using pre-implantation genetic testing for inherited conditions. Hum Reprod Update. 2021;27(5):944–66. Hughes et al. conducted a systematic literature review to report aspects of couples’ experiences with PGT. They used thematic analysis to summarize common patient motivations, attitudes, and decision-making factors and describe patient experiences with the decision process and the PGT process. The review provides insight on how to use these findings in clinical practice to best support patients considering PGT including holistic and thorough counseling and a multidisciplinary care team.
Lee I, Alur-Gupta S, Gallop R, Dokras A. Utilization of preimplantation genetic testing for monogenic disorders. Fertil Steril. 2020;114(4):854–60.
Yeates L, McDonald K, Burns C, Semsarian C, Carter S, Ingles J. Decision-making and experiences of preimplantation genetic diagnosis in inherited heart diseases: a qualitative study. Eur J Hum Genet. 2022;30(2):187–93. Yeates et al. conducted semi-structured interviews with 20 individuals recruited from a specialized cardiovascular genetics clinic in Australia to understand their experiences learning about and utilizing PGT-M for inherited cardiac conditions. Three themes emerged including the patient/family experience with the disease, familial and generational factors, and practical considerations which all impacted participants’ imagined future and their decision to pursue PGT-M or not. The article provides main points to discuss with patients/families considering PGT-M to best support families and highlights the benefit of a multidisciplinary specialized clinic in this setting.
Patton K, Wong EK, Cirino AL, Dobson LJ, Harris S. Reproductive decision-making and the utilization of preimplantation genetic testing among individuals with inherited aortic or vascular disease. J Genet Couns. 2023; https://doi.org/10.1002/jgc4.1759.
Pastore LM, Cordeiro Mitchell CN, Rubin LR, Nicoloro-SantaBarbara J, Genoff Garzon MC, Lobel M. Patients’ preimplantation genetic testing decision-making experience: an opinion on related psychological frameworks. Hum Reprod Open. 2019;2019(4):hoz019.
Hershberger PE, Gallo AM, Kavanaugh K, Olshansky E, Schwartz A, Tur-Kaspa I. The decision-making process of genetically at-risk couples considering preimplantation genetic diagnosis: initial findings from a grounded theory study. Soc Sci Med. 2012;74(10):1536–43.
Cheng L, Meiser B, Kirk E, Kennedy D, Barlow-Stewart K, Kaur R. Factors influencing patients’ decision-making about preimplantation genetic testing for monogenic disorders. Hum Reprod. 2022;37(11):2599–610.
Mor P, Brennenstuhl S, Metcalfe KA. Uptake of preimplantation genetic diagnosis in female BRCA1 and BRCA2 Mutation Carriers. J Genet Couns. 2018;27(6):1386–94.
Zuckerman S, Gooldin S, Zeevi DA, Altarescu G. The decision-making process, experience, and perceptions of preimplantation genetic testing (PGT) users. J Assist Reprod Genet. 2020;37(8):1903–12.
Resta R, Biesecker BB, Bennett RL, Blum S, Estabrooks Hahn S, Strecker MN, et al. A new definition of genetic counseling: national society of genetic counselors’ task force report. J Genet Couns. 2006;15(2):77–83.
Arscott P, Caleshu C, Kotzer K, Kreykes S, Kruisselbrink T, Orland K, et al. A case for inclusion of genetic counselors in cardiac care. Cardiol Rev. 2016;24(2):49–55.
Platt J. A person-centered approach to cardiovascular genetic testing. Cold Spring Harb Perspect Med. 2020;10(7):a036624.
Bains S, Neves R, Bos JM, Giudicessi JR, MacIntyre C, Ackerman MJ. Phenotypes of overdiagnosed long QT syndrome. J Am Coll Cardiol. 2023;81(5):477–86.
Amendola LM, Jarvik GP, Leo MC, McLaughlin HM, Akkari Y, Amaral MD, et al. Performance of ACMG-AMP variant-interpretation guidelines among nine laboratories in the clinical sequencing exploratory research consortium. Am J Hum Genet. 2016;98(6):1067–76.
Bland A, Harrington EA, Dunn K, Pariani M, Platt JCK, Grove ME, et al. Clinically impactful differences in variant interpretation between clinicians and testing laboratories: a single-center experience. Genet Med. 2018;20(3):369–73.
Reuter C, Grove ME, Orland K, Spoonamore K, Caleshu C. Clinical cardiovascular genetic counselors take a leading role in team-based variant classification. J Genet Couns. 2018;27(4):751–60.
Wain KE, Azzariti DR, Goldstein JL, Johnson AK, Krautscheid P, Lepore B, et al. Variant interpretation is a component of clinical practice among genetic counselors in multiple specialties. Genet Med. 2020;22(4):785–92.
Porto A, Gaber Caffrey R, Crowley-Matoka M, Spencer S, Li M, Propst L. Offering preimplantation genetic testing for monogenic disorders (PGT-M) for conditions with reduced penetrance or variants of uncertain significance: ethical insight from U.S. laboratory genetic counselors. J Genet Couns. 2022;31(1):261–8.
Landry LG, Rehm HL. Association of racial/ethnic categories with the ability of genetic tests to detect a cause of cardiomyopathy. JAMA Cardiol. 2018;3(4):341.
Cheng L, Meiser B, Kirk E, Kennedy D, Barlow-Stewart K, Kaur R. Decisional needs of patients considering preimplantation genetic testing: a systematic review. Reprod Biomed Online. 2022;44(5):839–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Chelsea Stevens declares that she has no conflict of interest related to this work.
Robyn Hylind that she has no conflict of interest related to this work.
Sophie Adams declares she has no conflicts of interest related to this work.
Allison Cirino that she has no conflict of interest related to this work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stevens, C., Hylind, R., Adams, S. et al. Preimplantation Genetic Testing for Inherited Heart Diseases. Curr Cardiovasc Risk Rep 17, 195–203 (2023). https://doi.org/10.1007/s12170-023-00727-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12170-023-00727-0