Abstract
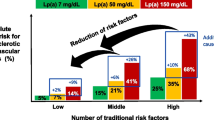
Elevated plasma concentration of lipoprotein (a) (Lp(a)) is an independent risk factor for the development of atherosclerotic coronary vascular disease. There is a causal relationship between Lp(a) elevation and myocardial infarction. In the pediatric population, Lp(a) has been associated with risk for ischemic stroke. However, a consensus regarding the clinical utility of Lp(a) measurement in children has not been established. In this article, we review recent literature regarding Lp(a) metabolism, its role in disease states such as in pediatric thrombosis and familial hypercholesterolemia (FH), and therapy directed at Lp(a) levels. Our findings show that Lp(a) remains a controversial but emerging risk factor for cardiovascular disease, especially in children. However, new and important research continues to contribute to our understanding of Lp(a) metabolism in children and to cardiovascular risk in diseases such as FH. What is clear is that Lp(a) has the potential to play a role in the management of cardiovascular risk in children and adults.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
•• Schmidt K, Noureen A, Kronenberg F, Utermann G. Structure, function, and genetics of lipoprotein (a). J Lipid Res. 2016;57:1339–59. An excelent resource related to the physiology and genetics of Lp(a).
•• Koschinsky ML, Marcovina, SM. Lipoprotein(a). In: Ballantyne CM, ed. Clinical lipidology, a companion to Braunwald’s Heart Disease: Elsevier Saunders; 2015:109–127.A comprehensive review of Lp(a).
Linton MF, Yancey PG, Davies SS, Jerome WGJ, Linton EF, Vickers KC. In: De Groot LJ, Beck-Peccoz P, Chrousos G, et al., editors. The role of lipids and lipoproteins in atherosclerosis. South Dartmouth: Endotext; 2016. p. 1–91.
Rader DJ, Cain W, Ikewaki K, et al. The inverse association of plasma lipoprotein(a) concentrations with apolipoprotein(a) isoform size is not due to differences in Lp(a) catabolism but to differences in production rate. J Clin Invest. 1994;93:2758–63.
Rader DJ, Mann WA, Cain W, et al. The low density lipoprotein receptor is not required for normal catabolism of Lp(a) in humans. J Clin Invest. 1995;95:1403–8.
Yang XP, Amar MJ, Vaisman B, et al. Scavenger receptor-BI is a receptor for lipoprotein(a). J Lipid Res. 2013;54:2450–7.
Taleb A, Witztum JL, Tsimikas S. Oxidized phospholipids on apoB-100-containing lipoproteins: a biomarker predicting cardiovascular disease and cardiovascular events. Biomark Med. 2011;5:673–94.
Linton MF, Farese RV Jr, Chiesa G, et al. Transgenic mice expressing high plasma concentrations of human apolipoprotein B100 and lipoprotein(a). J Clin Invest. 1993;92:3029–37.
Schneider M, Witztum JL, Young SG, et al. High-level lipoprotein [a] expression in transgenic mice: evidence for oxidized phospholipids in lipoprotein [a] but not in low density lipoproteins. J Lipid Res. 2005;46:769–78.
Tsimikas S, Clopton P, Brilakis ES, et al. Relationship of oxidized phospholipids on apolipoprotein B-100 particles to race/ethnicity, apolipoprotein(a) isoform size, and cardiovascular risk factors: results from the Dallas Heart Study. Circulation. 2009;119:1711–9.
Tsimikas S, Mallat Z, Talmud PJ, et al. Oxidation-specific biomarkers, lipoprotein(a), and risk of fatal and nonfatal coronary events. J Am Coll Cardiol. 2010;56:946–55.
Boerwinkle E, Leffert CC, Lin J, Lackner C, Chiesa G, Hobbs HH. Apolipoprotein(a) gene accounts for greater than 90% of the variation in plasma lipoprotein(a) concentrations. J Clin Invest. 1992;90:52–60.
Moliterno DJ, Jokinen EV, Miserez AR, et al. No association between plasma lipoprotein(a) concentrations and the presence or absence of coronary atherosclerosis in African-Americans. Arterioscler Thromb Vasc Biol. 1995;15:850–5.
Paultre F, Pearson TA, Weil HF, et al. High levels of Lp(a) with a small apo(a) isoform are associated with coronary artery disease in African American and white men. Arterioscler Thromb Vasc Biol. 2000;20:2619–24.
Virani SS, Brautbar A, Davis BC, et al. Associations between lipoprotein(a) levels and cardiovascular outcomes in black and white subjects: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2012;125:241–9.
Erqou S, Kaptoge S, Perry PL, et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009;302:412–23.
Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301:2331–9.
Luke MM, Kane JP, Liu DM, et al. A polymorphism in the protease-like domain of apolipoprotein(a) is associated with severe coronary artery disease. Arterioscler Thromb Vasc Biol. 2007;27:2030–6.
Clarke R, Peden JF, Hopewell JC, et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med. 2009;361:2518–28.
Ballantyne CM. Clinical lipidology : a companion to Braunwald's heart disease. Philadelphia: Saunders/Elsevier; 2009.
Langer C, Tambyrayah B, Nowak-Göttl U. Testing for apolipoprotein(a) phenotype using isoelectric focusing and immunoblotting technique. Methods Mol Biol. 2013;992:407–12.
Langer C, Tambyrayah B, Thedieck S, Nowak-Göttl U. Testing for lipoprotein(a) concentration and apolipoprotein(a) phenotypes: method standardization and pediatric reference values. Semin Thromb Hemost. 2011;37:810–3.
Martin SS, Blaha MJ, Toth PP, et al. Very large database of lipids: rationale and design. Clin Cardiol. 2013;36:641–8.
Sorensen KE, Celermajer DS, Georgakopoulos D, Hatcher G, Betteridge DJ, Deanfield JE. Impairment of endothelium-dependent dilation is an early event in children with familial hypercholesterolemia and is related to the lipoprotein(a) level. J Clin Invest. 1994;93:50–5.
Giuliano IC, Coutinho MS, Freitas SF, Pires MM, Zunino JN, Ribeiro RQ. Serum lipids in school kids and adolescents from Florianópolis, SC, Brazil—Healthy Floripa 2040 study. Arq Bras Cardiol. 2005;85:85–91.
Kronenberg F. Lipoprotein(a): there's life in the old dog yet. Circulation. 2014;129:619–21.
Luca A, Holoc AS. The role of lipoprotein (a) in cardiovascular diseases in children and adolescents. SEA - Practical Application of Science 2016;11:229–32.
McNeal CJ. Lipoprotein(a): its relevance to the pediatric population. J Clin Lipidol. 2015;9:S57–66.
Rodríguez-Moran M, Guerrero-Romero F. Low birthweight and elevated levels of lipoprotein(a) in prepubertal children. J Paediatr Child Health. 2014;50:610–4.
Kwiterovich PO, Virgil DG, Garrett ES, et al. Lipoprotein heterogeneity at birth: influence of gestational age and race on lipoprotein subclasses and Lp (a) lipoprotein. Ethn Dis. 2004;14:351–9.
Obisesan O, Aliyu MH, Adediran AS, Bond V, Maxwell CJ, Rotimi CN. Correlates of serum lipoprotein (a) in children and adolescents in the United States. The third National Health Nutrition and Examination Survey (NHANES-III). Lipids Health Dis. 2004;3:29.
Srinivasan SR, Dahlen GH, Jarpa RA, Webber LS, Berenson GS. Racial (black-white) differences in serum lipoprotein (a) distribution and its relation to parental myocardial infarction in children. Bogalusa Heart Study Circ. 1991;84:160–7.
Emerging Risk Factors C, Erqou S, Kaptoge S, et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009;302:412–23.
Goldenberg NA, Bernard TJ, Hillhouse J, et al. Elevated lipoprotein (a), small apolipoprotein (a), and the risk of arterial ischemic stroke in north American children. Haematologica. 2013;98:802–7.
Kenet G, Lutkhoff LK, Albisetti M, et al. Impact of thrombophilia on risk of arterial ischemic stroke or cerebral sinovenous thrombosis in neonates and children: a systematic review and meta-analysis of observational studies. Circulation. 2010;121:1838–47.
Nave AH, Lange KS, Leonards CO, et al. Lipoprotein (a) as a risk factor for ischemic stroke: a meta-analysis. Atherosclerosis. 2015;242:496–503.
Smolders B, Lemmens R, Thijs V. Lipoprotein (a) and stroke: a meta-analysis of observational studies. Stroke. 2007;38:1959–66.
Sultan SM, Schupf N, Dowling MM, Deveber GA, Kirton A, Elkind MS. Review of lipid and lipoprotein(a) abnormalities in childhood arterial ischemic stroke. Int J Stroke. 2014;9:79–87.
Marcovina SM, Hegele RA, Koschinsky ML. Lipoprotein(a) and coronary heart disease risk. Curr Cardiol Rep. 1999;1:105–11.
Rowland CM, Pullinger CR, Luke MM, et al. Lipoprotein (a), LPA Ile4399Met, and fibrin clot properties. Thromb Res. 2014;133:863–7.
Angles-Cano E, Hervio L, Rouy D, et al. Effects of lipoprotein(a) on the binding of plasminogen to fibrin and its activation by fibrin-bound tissue-type plasminogen activator. Chem Phys Lipids. 1994;67-68:369–80.
Danik JS, Buring JE, Chasman DI, Zee RY, Ridker PM, Glynn RJ. Lipoprotein(a), polymorphisms in the LPA gene, and incident venous thromboembolism among 21483 women. J Thromb Haemost. 2013;11:205–8.
Kamstrup PR, Tybjaerg-Hansen A, Nordestgaard BG. Genetic evidence that lipoprotein(a) associates with atherosclerotic stenosis rather than venous thrombosis. Arterioscler Thromb Vasc Biol. 2012;32:1732–41.
Thom K, Male C, Mannhalter C, et al. No impact of endogenous prothrombotic conditions on the risk of central venous line-related thrombotic events in children: results of the KIDCAT study (KIDs with Catheter Associated Thrombosis). J Thromb Haemost. 2014;12:1610–5.
Fullerton HJ, Wu YW, Sidney S, Johnston SC. Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: the importance of cerebrovascular imaging. Pediatrics. 2007;119:495–501.
Schoenberg BS, Mellinger JF, Schoenberg DG. Cerebrovascular disease in infants and children: a study of incidence, clinical features, and survival. Neurology. 1978;28:763–8.
Fullerton HJ, Wintermark M, Hills NK, et al. Risk of recurrent arterial ischemic stroke in childhood: a prospective international study. Stroke. 2016;47:53–9.
Ganesan V, Prengler M, Wade A, Kirkham FJ. Clinical and radiological recurrence after childhood arterial ischemic stroke. Circulation. 2006;114:2170–7.
Berglund L, Ramakrishnan R. Lipoprotein(a): an elusive cardiovascular risk factor. Arterioscler Thromb Vasc Biol. 2004;24:2219–26.
Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: national heart, lung, and blood institute: expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 2011;128 Suppl 5:S213–56.
Gidding SS, Champagne MA, de Ferranti SD, et al. The agenda for familial hypercholesterolemia: a scientific statement from the American Heart Association. Circulation. 2015;132:2167–92.
•• Langsted A, Kamstrup PR, Benn M, Tybjærg-Hansen A, Nordestgaard BG. High lipoprotein(a) as a possible cause of clinical familial hypercholesterolaemia: a prospective cohort study. Lancet Diabetes Endocrinol. 2016;4:577–87. An important study highlighting the role of Lp(a) in patients with Familial Hypercholesterolemia.
Alonso R, Andres E, Mata N, et al. Lipoprotein(a) levels in familial hypercholesterolemia: an important predictor of cardiovascular disease independent of the type of LDL receptor mutation. J Am Coll Cardiol. 2014;63:1982–9.
Santos RD. Familial hypercholesterolaemia: beware of lipoprotein(a). Lancet Diabetes Endocrinol. 2016;4:553–5.
Seed M, Hoppichler F, Reaveley D, et al. Relation of serum lipoprotein(a) concentration and apolipoprotein(a) phenotype to coronary heart disease in patients with familial hypercholesterolemia. N Engl J Med. 1990;322:1494–9.
Alonso R, Mata P, Muñiz O, et al. PCSK9 and lipoprotein (a) levels are two predictors of coronary artery calcification in asymptomatic patients with familial hypercholesterolemia. Atherosclerosis. 2016;254:249–53.
Vlahos AP, Naka KK, Bechlioulis A, et al. Endothelial dysfunction, but not structural atherosclerosis, is evident early in children with heterozygous familial hypercholesterolemia. Pediatr Cardiol. 2014;35:63–70.
Lapinleimu J, Raitakari OT, Lapinleimu H, et al. High lipoprotein(a) concentrations are associated with impaired endothelial function in children. J Pediatr. 2015;166:947–52. e1-2
Khera AV, Everett BM, Caulfield MP, et al. Lipoprotein(a) concentrations, rosuvastatin therapy, and residual vascular risk: an analysis from the JUPITER trial (justification for the use of statins in prevention: an intervention trial evaluating rosuvastatin). Circulation. 2014;129:635–42.
Maher VM, Brown BG, Marcovina SM, Hillger LA, Zhao XQ, Albers JJ. Effects of lowering elevated LDL cholesterol on the cardiovascular risk of lipoprotein(a). JAMA. 1995;274:1771–4.
Catapano AL, Reiner Z, De Backer G, et al. ESC/EAS guidelines for the management of dyslipidaemias the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European atherosclerosis society (EAS). Atherosclerosis. 2011;217:3–46.
•• Tsimikas S, Viney NJ, Hughes SG, et al. Antisense therapy targeting apolipoprotein(a): a randomised, double-blind, placebo-controlled phase 1 study. Lancet. 2015;386:1472–83. Landmark phase 1 study of ASO to apo(a) results in 78% reduction in Lp(a) levels.
Acknowledgements
This work was supported in part by the National Institutes of Health grants NIGMS NIH (T32 GM007569), HL116263, HL127173, HL105375.
None of the authors of this paper have a financial interest related to these studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Prendergast, Kelley and Lintons have no conflicts of interest to declare.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatrics
Rights and permissions
About this article
Cite this article
Prendergast, C.J., Kelley, J.C., Linton, E.F. et al. Lp(a) in Childhood. Curr Cardiovasc Risk Rep 11, 26 (2017). https://doi.org/10.1007/s12170-017-0553-6
Published:
DOI: https://doi.org/10.1007/s12170-017-0553-6