Abstract
Objective
False-positive bone lesions (bone pseudometastases) have been often reported in patients with esophageal cancer (EsoC). This study aimed to evaluate the vertebral 2-deoxy-2-[18F] fluoro-d-glucose (FDG) accumulation pattern in patients with newly diagnosed esophageal cancers and other malignancies (OtherT) to elucidate the possible mechanism that causes bone pseudometastasis.
Methods
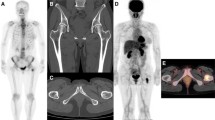
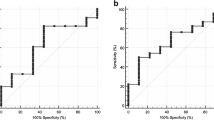
FDG positron emission tomography/computed tomography performed for 90 patients with EsoC, and 112 patients with OtherT was retrospectively evaluated. The uptake pattern in the thoracic (Th) and lumbar (L) vertebrae was visually assessed regarding predominance (TL, Th ≒ L; Td, Th > L; Ld, L > Th), main intensity compared with the uptake in the blood pool (BP) (Grade 1 < BP, Grade 2 ≒ BP, or Grade 3 > BP), and homogeneity (homogeneous, heterogeneous, marginal, or spotty). The patterns between EsoC and OtherT and between Th and L were compared.
Results
TL, Td, and Ld patterns were observed in 51.1%, 48.9%, and 0% in EsoC and 79.7%, 20.3%, and 0% in OtherT. Though Grade 2 was most frequently observed in both groups, the ratio of Grade 3 in Th and Grade 1 in L was significantly higher in EsoC than in OtherT. Heterogeneous and spotty patterns were more frequently observed in L and in EsoC, and these were strongly associated with Td pattern.
Conclusion
Td pattern was frequently seen, especially in EsoC, and was strongly associated with a heterogeneous or marginal pattern in the L. Heterogeneous marrow distribution with declined lumbar uptake is suspected as the mechanism of bone pseudometastasis.





Similar content being viewed by others
References
Gundlapalli S, Ojha B, Mountz JM. Granulocyte colony-stimulating factor: confounding F-18 FDG uptake in outpatient positron emission tomographic facilities for patients receiving ongoing treatment of lymphoma. Clin Nucl Med. 2002;27:140–1.
Hanaoka K, Hosono M, Usami K, Tatsumi Y, Yamazoe Y, Komeya Y, et al. Fluorodeoxyglucose uptake in the bone marrow after granulocyte colony-stimulating factor administration in patients with non-Hodgkin’s lymphoma. Nucl Med Commun. 2011;32:678–83.
Kazama T, Swanston N, Podoloff DA, Macapinlac HA. Effect of colony-stimulating factor and conventional- or high-dose chemotherapy on FDG uptake in bone marrow. Eur J Nucl Med Mol Imaging. 2005;32:1406–11.
Abravan A, Eide HA, Løndalen AM, Helland Å, Malinen E. Mapping bone marrow response in the vertebral column by positron emission tomography following radiotherapy and erlotinib therapy of lung cancer. Mol Imaging Biol. 2019;21:391–8.
Elicin O, Callaway S, Prior JO, Bourhis J, Ozsahin M, Herrera FG. [(18)F]FDG-PET standard uptake value as a metabolic predictor of bone marrow response to radiation: impact on acute and late hematological toxicity in cervical cancer patients treated with chemoradiation therapy. Int J Radiat Oncol Biol Phys. 2014;90:1099–107.
Okuyama C, Kubota T, Matsushima S, Nishida K, Oda M, Takenaka H, et al. FDG avid patchy bone marrow misinterpreted as melanoma metastases to bone in a case of aplastic anemia. Clin Nucl Med. 2009;34:927–30.
Bordalo-Rodrigues M, Galant C, Lonneux M, Clause D, Vande Berg BC. Focal nodular hyperplasia of the hematopoietic marrow simulating vertebral metastasis on FDG positron emission tomography. AJR Am J Roentgenol. 2003;180:669–71.
Ida S, Watanabe M, Yamao T, Ishimoto T, Nagai Y, Iwatsuki M, et al. False-positive 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) findings of bone metastasis from esophagogastric cancer: report of two cases. Surg Today. 2014;44:2191–4.
Okuda S, Nishibori H, Hoshi H. Utility of (111) In-Cl3 scintigraphy for differentiating bone marrow reconversion. J Nucl Med Technol. 2017. https://doi.org/10.2967/jnmt.117.197913.
Okuyama C, Sasaki N, Nishimura M, Matsushima S, Yoshimatsu R. Active bone marrow with focal FDG accumulation mimicking bone metastasis with a case of early esophageal cancer. Clin Nucl Med. 2018;43:258–61.
Shigematsu Y, Hirai T, Kawanaka K, Shiraishi S, Yoshida M, Kitajima M, et al. Distinguishing imaging features between spinal hyperplastic hematopoietic bone marrow and bone metastasis. AJNR Am J Neuroradiol. 2014;35:2013–20.
Tanaka T, Gobara H, Inai R, Iguchi T, Tada A, Sato S, et al. A case of focal bone marrow reconversion mimicking bone metastasis: the value of 111Indium chloride. Acta Med Okayama. 2016;9:679–84.
Yasuda H, Shimura T, Okigami M, Yoshiyama S, Ohi M, Tanaka K, et al. Esophageal cancer with bone marrow hyperplasia mimicking bone metastasis: report of a case. Case Rep Oncol. 2016;9:679–84.
Okuyama C, Higashi T, Ishizu K, Nakamoto R, Takahashi M, Kusano K, et al. Bone pseudometastasis on 18F-FDG PET in Japanese patients with esophageal cancer. Clin Nucl Med. 2019;44:771–6.
Nakamoto Y, Osman M, Wahl RL. Prevalence and patterns of bone metastases detected with positron emission tomography using F-18 FDG. Clin Nucl Med. 2003;28:302–7.
Abouzied MM, Crawford ES, Nabi HA. 18F-FDG imaging: pitfalls and artifacts. J Nucl Med Technol. 2005;33:145–55.
Cook GJ, Wegner EA, Fogelman I. Pitfalls and artifacts in 18FDG PET and PET/CT oncologic imaging. Semin Nucl Med. 2004;34:122–33.
Shammas A, Lim R, Charron M. Pediatric FDG PET/CT: physiologic uptake, normal variants, and benign conditions. RadioGraphics. 2009;29:1467–86.
Hwang S, Panicek DM. Magnetic resonance imaging of bone marrow in oncology, part 1. Skeletal Radiol. 2007;36:913–20.
Vogler JB 3rd, Murphy WA. Bone marrow imaging. Radiology. 1988;168:679–93.
Vande Berg BC, Lecouvet FE, Galant C, Maldague BE, Malghem J. Normal variants and frequent marrow alterations that simulate bone marrow lesions at MR imaging. Radiol Clin North Am. 2005;43:761–70.
Małkiewicz A, Dziedzic M. Bone marrow reconversion—imaging of physiological changes in bone marrow. Pol J Radiol. 2012;77:45–50.
Nouh MR, Eid AF. Magnetic resonance imaging of the spinal marrow: basic understanding of the normal marrow pattern and its variant. World J Radiol. 2015;7:448–58.
Ollivier L, Gerber S, Vanel D, Brisse H, Leclère J. Improving the interpretation of bone marrow imaging in cancer patients. Cancer Imaging. 2006;6:194–8.
Chen C, Yan LM, Guo KY, Wang YJ, Zou F, Gu WW, et al. The diagnostic value of 18F-FDG-PET/CT in hematopoietic radiation toxicity: a Tibet minipig model. J Radiat Res. 2012;53:537–44.
Klaus HD. Possible prostate cancer in northern Peru: Differential diagnosis, vascular anatomy, and molecular signaling in the paleopathology of metastatic bone disease. Int J Paleopathol. 2018;21:147–57.
Zhang HZ, Jin GF, Shen HB. Epidemiologic differences in esophageal cancer between Asian and Western populations. Chin J Cancer. 2012;31:281–6.
Chen S, Zhou K, Yang L, Ding G, Li H. Racial differences in esophageal squamous cell carcinoma: incidence and molecular features. Biomed Res Int. 2017. https://doi.org/10.1155/2017/1204082.
Brooks PJ, Enoch MA, Goldman D, Li TK, Yokoyama A. The alcohol flushing response: an unrecognized risk factor for esophageal cancer from alcohol consumption. PLOS Med. 2009. https://doi.org/10.1371/journal.pmed.1000050.
Yokoyama A, Kato H, Yokoyama T, Tsujinaka T, Muto M, Omori T, et al. Genetic polymorphisms of alcohol and aldehyde dehydrogenases and glutathione S-transferase M1 and drinking, smoking, and diet in Japanese men with esophageal squamous cell carcinoma. Carcinogenesis. 2002;23:1851–9.
Shinomiya H, Shinomiya H, Kubo M, Saito Y, Yoshida M, Ando M, et al. Prognostic value of ALDH2 polymorphism for patients with oropharyngeal cancer in a Japanese population. PLoS ONE. 2017;12:e0187992.
Oze I, Matsuo K, Hosono S, Ito H, Kawase T, Watanabe M, et al. Comparison between self-reported facial flushing after alcohol consumption and ALDH2 Glu504Lys polymorphism for risk of upper aerodigestive tract cancer in a Japanese population. Cancer Sci. 2010;101:1875–80.
Ballard HS. The hematological complications of alcoholism. Alcohol Health Res World. 1997;21:42–52.
Latvala J, Parkkila S, Niemelä O. Excess alcohol consumption is common in patients with cytopenia: studies in blood and bone marrow cells. Alcohol Clin Exp Res. 2004;28:619–24.
Maddalozzo GF, Turner RT, Edwards CH, Howe KS, Widrick JJ, Rosen CJ, et al. Alcohol alters whole body composition, inhibits bone formation, and increases bone marrow adiposity in rats. Osteoporos Int. 2009;20:1529–38.
Yokoyama A, Brooks PJ, Yokoyama T, Mizukami T, Shiba S, Nakamoto N, et al. Recovery from anemia and leukocytopenia after abstinence in Japanese alcoholic men and their genetic polymorphisms of alcohol dehydrogenase-1B and aldehyde dehydrogenase-2. Jpn J Clin Oncol. 2017;47:306–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okuyama, C., Higashi, T., Nakamoto, R. et al. Predominance and homogeneity patterns of physiological FDG accumulation in thoracic and lumbar vertebrae: suspected mechanism of “bone pseudometastasis” on FDG-PET in Japanese patients with esophageal cancer. Ann Nucl Med 34, 182–191 (2020). https://doi.org/10.1007/s12149-019-01430-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-019-01430-0