Abstract
Background
Despite recent technological advances allowing for quantitative single-photon emission computed tomography (SPECT), quantitative SPECT has not been widely used in the clinical practice of osteoporosis. The aim of this study is to evaluate the feasibility of quantitative bone SPECT/CT for measuring lumbar standard uptake value (SUV) in patients with different bone-mineral density (BMD), and investigate the correlation between SUV measured with 99mTc-methylene diphosphonate (MDP) SPECT/CT and BMD assessment by dual-energy X-ray absorptiometry (DXA).
Methods
A retrospective analysis of 62 cases 99mTc-MDP whole-body bone imaging and local lumbar SPECT/CT tomography were performed. According to the results of dual-energy X-ray bone density examination, they were divided into normal group, osteopenic group, and osteoporosis group. The raw SPECT data were reconstructed using flash3D which includes attenuation correction, scatter compensation, and collimator resolution recovery, SPECT images from this algorithm were calibrated for SUV analysis. Comparing difference of lumbar SUV in different BMD subjects, and investigating the correlation between lumbar SUV and BMD. Data were analyzed by one-way ANOVA and Pearson regression analysis using SPSS 17.0 software.
Results
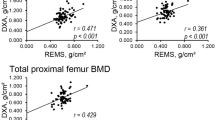
The maximum SUV (SUVmax) and mean SUV (SUVmean) of L1–L4 vertebral in 62 subjects were 7.39 ± 1.84 and 4.90 ± 1.27, respectively. The average BMD was 0.85 ± 0.15 (g/cm2), and the average CT value was 145.88 ± 53.99 (HU). The SUVmax, SUVmean, BMD, and CT values of the lumbar spine were statistically significantly different among the three groups (F = 24.089, 30.501, 94.847, 30.241, all p < 0.001), and the osteopenic group was significantly lower than the normal group (all p < 0.001), the osteoporosis group was significantly lower than the normal group and the osteopenic group (all p < 0.001). Lumbar SUVmax, SUVmean, and BMD were significantly negatively correlated with age (r = − 0.328 to − 0.442, all p < 0.05), and positively correlated with body weight and CT value (r = 0.299–0.737, all p < 0.05), but no significant correlation with height (r = 0.006–0.175, all p > 0.05). Lumbar SUVmax and SUVmean increased significantly with the increase of BMD (r = 0.638, 0.632, p < 0.001).
Conclusion
The SUV of lumbar spine in 99mTc-MDP bone SPECT/CT was significantly different among subjects with different BMD, and the SUV was positively correlated with BMD. These findings justify that quantitative bone SPECT/CT is an applicable tool for clinical quantification of bone metabolism in osteoporosis patients.


Similar content being viewed by others
References
Bailey DL, Willowson KP. Quantitative SPECT/CT: SPECT joins PET as a quantitative imaging modality. Eur J Nucl Med Mol Imaging. 2014;41(Suppl 1):S17–S25.
Armstrong IS, Hoffmann SA. Activity concentration measurementsusing a conjugate gradient (Siemens xSPECT) reconstruction algorithmin SPECT/CT. Nucl Med Commun. 2016;37:1212–7.
Ross JC, Vilic D, Sanderson T, Vöö S, Dickson J. Does quantification have a role to play in the future of bone SPECT? Eur J Hybrid Imaging. 2019;3:8.
Kaneta T, Ogawa M, Daisaki H, Nawata S, Yoshida K, Inoue T. SUV measurement of normal vertebrae using SPECT/CT with Tc-99m methylene diphosphonate. Am J Nucl Med Mol Imaging. 2016;6(5):262–8.
Cachovan M, Vija AH, Hornegger J, Kuwert T. Quantification of 99mTc-DPD concentration in the lumbar spine with SPECT/CT. EJNMMI Res. 2013;3:1–8.
Lewiecki EM, Laster AJ, Miller PD, Bilezikian JP. More bone density testing is needed, not less. J Bone Miner Res. 2012;27:739–42.
Söderberg M, Gunnarsson M. The effect of different adaptation strengths on image quality and radiation dose using Siemens Care Dose 4D. Radiat Prot Dosimetry. 2010;139:173–9.
Römer W, Reichel N, Vija HA, et al. Isotropic reconstruction of SPECT data using OSEM3D: correlation with CT. Acad Radiol. 2006;13:496–502.
Huang KM, Feng YL, Liang WT, Li L, Feng YX, Deng DL. Absolute quantitative phantom of SPECT/CT imaging based on specified reconstruction algorithms and correction methods. Chin J Nucl Med Mol Imaging. 2018;38:340–4.
Huang KM, Feng YL, Liang WT, et al. Impact of partial volume effect on quantitative results in SPECT/CT. Chin J Med Imaging. 2017;25:867–71.
Suh MS, Lee WW, Kim Y-K, Yun P-Y, Kim SE. Maximum standardized uptake evalue of (99m)Tc hydroxymethylene diphosphonate SPECT/CT for the evaluation of temporomandibular joint disorder. Radiology. 2016;280:890–6.
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster J-Y (2013) European guidance for thediagnosis and management of osteoporosis in postmeno-pausal women. Osteoporos Int 24:23–57.
Bailey DL, Willowson KP. An evidence-based review of quantitative SPECT imaging and potential clinical applications. J Nucl Med. 2013;54:83–9.
Ritt P, Vija H, Hornegger J, Kuwert T. Absolute quantification in SPECT. Eur J Nucl Med Mol Imaging. 2011;38(Suppl 1):S67–S77.
Willowson K, Bailey DL, Bailey EA, Baldock C, Roach PJ. In vivo validation of quantitative SPECT in the heart. Clin Physiol Funct Imaging. 2010;30:214–9.
Rowe SP, Vicente E, Anizan N, et al. Repeatability of radiotracer uptake in normal abdominal organs with 111In-pentetreotide quantitative SPECT/CT. J Nucl Med. 2015;56:985–8.
Willowson K, Bailey DL, Schembri G, Baldock C. CT-based quantitative SPECT for the radionuclide 201Tl: experimental validation and a standardized uptake value for brain tumour patients. Cancer Imaging. 2012;12:31–40.
Zeintl J, Vija AH, Yahil A, Hornegger J, Kuwert T. Quantitative accuracy of clinical 99mTc SPECT/CT using ordered-subset expectation maximization with 3-dimensional resolution recovery, attenuation, and scatter correction. J Nucl Med. 2010;51:921–8.
Shcherbinin S, Celler A, Belhocine T, Vanderwerf R, Driedger A. Accuracy of quantitative reconstructions in SPECT/CT imaging. Phys Med Biol. 2008;53:4595–604.
Yamane T, Kuji I, Seto A, Matsunari I. Quantification of osteoblastic activity in epiphyseal growth plates by quantitative bone SPECT/CT. Skeletal Radiol. 2018;47:805–10.
Umeda T, Koizumi M, Fukai S, et al. Evaluation of bone metastatic burden by bone SPECT/CT in metastatic prostate cancer patients: defining threshold value for total bone uptake and assessment in radium-223 treated patients. Ann Nucl Med. 2018;32:105–13.
Kim J, Lee H-H, Kang Y, et al. Maximum standardised uptake value of quantitative bone SPECT/CT in patients with medial compartment osteoarthritis of the knee. Clin Radiol. 2017;72:580–9.
Uchida K, Nakajima H, Miyazaki T, et al. Effects of alendronate on bone metabolism in glucocorticoid-induced osteoporosis measured by 18 F-fluoride PET: a prospective study. J NuclMed. 2009;50:1808–14.
Kuji I, Yamane T, Seto A, Yasumizu Y, Shirotake S, Oyama M. Skeletal standardized uptake values obtained by quantitative SPECT/CT as anosteoblastic biomarker for the discrimination of active bone metastasis in prostate cancer. Eur J Hybrid Imaging. 2017;1:2–17.
He W, Zhai W, Steien S, et al. A novel quantification of 99mTc-MDP concentration and 18F-FDG PET/CT metabolism in lumbar disc herniation patients. J Nucl Med. 2016;57(Suppl 2):1817.
Beck M, Sanders JC, Ritt P, Reinfelder J, Kuwert T. Longitudinal analysis of bone metabolism using SPECT/CT and 99mTc-diphosphono-Propanedi carboxylic acid: comparison of visual and quantitative analysis. EJNMMI Res. 2016;6:60.
Toegel S, Hoffmann O, Wadsak W, et al. Uptake of boneseekers is solely associated with mineralization: a study with 99mTc-MDP,153Sm-EDTMP and 18F-fluoride on osteoblasts. Eur J Nucl Med. 2006;33:491–4.
Blake GM, Frost ML, Moore AE, Siddique M, Fogelman I. The Assessment of regional skeletal metabolism: studies of osteoporosis treatments using quantitative radionuclide imaging. J Clin Densitom. 2011;3(14):263–71.
Moore AE, Blake GM, Taylor KA, Ruff VA, Rana AE, Wan XH, et al. (2012) Changes observed in radionuclide bone scan during and after teriparatide treatment for osteoporosis. Eur J Nucl Med Mol Imaging 39:326–336.
Jassel IS, Siddique M, Frost ML, Moore AEB, Puri T, Blake GM. The influence of CT and dual-energy X-ray absorptiometry (DXA) bone density on quantitative [18F] sodium fluoride PET. Quant Imaging Med Surg. 2019;9:201–9.
Blain H, Chavassieux P, Portero-Muzy N, et al. Cortical and trabecular bone distribution in the femoral neck in osteoporosis and osteoarthritis. Bone. 2008;43:862–8.
Acknowledgements
We would like to thank Yexia Feng and Dalang Deng for the data collection. We also thank Fengwen Yu and Ming Yang for their excellent technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest that would prejudice their impartiality.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, K., Feng, Y., Liu, D. et al. Quantification evaluation of 99mTc-MDP concentration in the lumbar spine with SPECT/CT: compare with bone mineral density. Ann Nucl Med 34, 136–143 (2020). https://doi.org/10.1007/s12149-019-01425-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-019-01425-x