Abstract
Objective
Staging of bronchiolitis obliterans syndrome (BOS) following lung transplantation is based on declines in forced expiratory volume in 1 s (FEV1). The aim of this study was to evaluate the usefulness of 133Xe ventilation scintigraphy in the early detection of BOS following living-donor lobar lung transplantation (LDLLT), to compare 133Xe washout imaging with computed tomography (CT) findings for early detection of BOS following LDLLT, and to evaluate 133Xe washout imaging by quantitative analyses.
Methods
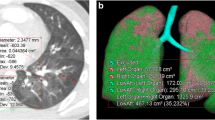
Subjects comprised 30 double-lung recipients and 1 single-lung recipient, who had undergone LDLLT at our institution and survived more than 1 year. Clinically diagnosed BOS developed in six recipients. Declines in graft function were evaluated using a combination of three methods, namely, dynamic spirometry, high-resolution CT (HRCT), and 133Xe ventilation scintigraphy. Findings for all transplanted lungs were compared between CT and 133Xe washout imaging. 133Xe washout imaging was assessed using mean transit time (MTT) of bi-and unilateral lungs. Correlations between MTT of bilateral lungs and FEV1% were evaluated. Differences in MTT between BOS and non-BOS lungs, and between non-BOS and donor lungs were also evaluated on unilateral lungs. Appropriate cut-off values of MTT of unilateral lungs were set for the diagnosis of BOS.
Results
In all six BOS cases, prolonged-washout images of engrafted lungs revealed early-phase BOS with declines from baseline FEV1, whereas only one BOS case could be detected using early CT findings of BO (bronchodilatation, decrease in number and size of pulmonary vessels, thickening of septal lines, and volume reduction). A significant correlation was identified between MTT and FEV1% (r = −0.346, P < 0.0001). MTT of unilateral lungs was significantly longer in BOS lungs than in non-BOS lungs (P < 0.0001). The cut-off MTT of unilateral lungs for the diagnosis of BOS was set at 64.77 s.
Conclusions
Our data show that 133Xe washout imaging offers excellent potential for early detection of BOS compared with early CT findings. Using 133Xe washout imaging and MTT with radioactive tracer offers a noninvasive indication of selective ventilatory function in engrafted lungs following LDLLT. MTT appears useful for identifying BOS following LDLLT and allows quantitative evaluation of graft function in unilateral lungs.
Similar content being viewed by others
References
Burke CM, Glanville AR, Theodore J, Robin ED. Lung immunogenicity, rejection, and obliterative bronchiolitis. Chest 1987;92:547–549.
Morrish WF, Herman SJ, Weisbrod GL, Chamberlain DW. Bronchiolitis obliterans after lung transplantation: findings at chest radiography and high-resolution CT. The Toronto Lung Transplant Group. Radiology 1991;179:487–490.
Ikonen T, Kivisaari L, Taskinen E, Piilonen A, Harjula AL. High-resolution CT in long-term follow-up after lung transplantation. Chest 1997;111:370–376.
Ikonen T, Harjula AL, Kinnula VL, Savola J, Sovijarvi A. Assessment of forced expiratory volume in one secondfraction of the engrafted lung with 133-Xe radiospirometry improves the diagnosis of bronchiolitis obliterans syndrome in single lung transplant recipients. J Heart Lung Transplant 1995;14:244–250.
Suga K, Nishigauchi K, Kume N, Takano K, Koike S, Shimizu K, et al. Ventilation abnormalities in obstructive airways disorder: detection with pulmonary dynamic densitometry by means of spiral CT versus dynamic Xe-133 SPECT. Radiology 1997;202:855–862.
Cooper JD, Billingham M, Egan T, Hertz MI, Higenbottam T, Lynch J, et al. A working formulation for the standardization of nomenclature and for clinical staging of chronic dysfunction in lung allografts: International Society for Heart and Lung Transplantation. J Heart Lung Transplant 1993;12:713–716.
Estenne M, Maurer JR, Boehler A, Egan JJ, Frost A, Hertz M, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant 2002;21:297–310.
Allen MD, Burke CM, McGregor CG, Baldwin JC, Jamieson SW, Theodore J. Steroid-responsive bronchiolitis obliterans after human heart-lung transplantation. J Thorac Cardiovasc Surg 1986;92:449–451.
Glanville AR, Baldwin JC, Burke CM, Theodore J, Robin ED. Obliterative bronchiolitis after heart-lung transplantation: apparent arrest by augmented immunosuppression. Ann Intern Med 1987;107:300–304.
Hisada K, Tonami N, Kubo A. A new textbook of clinical nuclear medicine. 3rd ed. Tokyo: Kanehara; 2002. p. 308.
Suga K, Nishigauchi K, Kume N, Koike S, Takano K, Tokuda O, et al. Dynamic pulmonary SPECT of xenon-133 gas washout. J Nucl Med 1996;37:807–814.
Suga K, Nishigauchi K, Kume N, Koike S, Takano K, Matsunaga N. Regional ventilatory evaluation using dynamic SPET imaging of xenon-133 washout in obstructive lung disease: an initial study. Eur J Nucl Med 1995;22:220–226.
Uchiyama H, Uchiyama M, Shishikura Y, Hoshi Y, Mori Y, Tominaga S. Bronchiolitis obliterans after bone marrow transplantation: evaluation with lung scintigraphy. Int J Hematol 1998;68:213–220.
Ikonen T, Sovijarvi AR, Taskinen E, Uusitalo M, Kivisaari L, Aarnio P, et al. Detection of acute rejection by 133Xe radiospirometry after single lung transplantation in an experimental porcine model. Eur Surg Res 1997;29:12–19.
Levine SM, Jenkinson SG, Bryan CL, Anzueto A, Zamora CA, Gibbons WJ, et al. Ventilation-perfusion inequalities during graft rejection in patients undergoing single lung transplantation for primary pulmonary hypertension. Chest 1992;101:401–405.
Kramer MR, Marshall SE, McDougall IR, Kloneck A, Strarnes VA, Lewiston NJ, et al. The distribution of ventilation and perfusion after single-lung transplantation in patients with pulmonary fibrosis and pulmonary hypertension. Transplant Proc 1991;23:1215–1216.
Johansson A, Moonen M, Enocson A, Martensson G, Bake B. Detection of chronic rejection by quantitative ventilation scintigrams in lung-transplanted patients: a pilot study. Clin Physiol Funct Imaging 2005;25:183–187.
Ouwens JP, van der Bij W, van der Mark TW, Geertsma A, Piers DA, de Boer WJ, et al. The value of ventilation scintigraphy after single lung transplantation. J Heart Jung Transplant 2004;23:115–121.
Hudson M, Ninan T, Russell G. Evaluation of mean transit time in children as an indicator of airways obstruction. Respir Med 1992;86:301–304.
Burke CM, Theodore J, Dawkins KD, Yousem SA, Blank N, Billingham ME, et al. Post-transplant obliterative bronchiolitis and other late lung sequelae in human heart-lung transplantation. Chest 1984;86:824–829.
Paradis I, Yousem S, Griffith B. Airway obstruction and bronchiolitis obliterans after lung transplantation. Clin Chest Med 1993;14:751–763.
Date H. Experience with cyclosporine in living-donor lobar lung transplantation. Transplant Proc 2004;36:349S–351S.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shinya, T., Sato, S., Kato, K. et al. Assessment of mean transit time in the engrafted lung with 133Xe lung ventilation scintigraphy improves diagnosis of bronchiolitis obliterans syndrome in living-donor lobar lung transplant recipients. Ann Nucl Med 22, 31–39 (2008). https://doi.org/10.1007/s12149-007-0078-z
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s12149-007-0078-z