Abstract
Self-compassion is an important psychological skill that may facilitate the adoption of a mindful way of parenting, especially during the COVID‐19 pandemic. However, the association between these constructs may be explained by several variables, such as maternal psychopathological symptoms, with a well-established interference in parenting. This study aimed to compare mothers who experienced and mothers who did not experience a negative emotional impact of the COVID-19 pandemic on self-compassion, mindful parenting, postpartum depressive symptoms (PPDS) and postpartum anxious symptoms (PPAS). We also explored whether mothers’ self-compassion was associated with mindful parenting and whether this relationship may be mediated by PPDS and PPAS. A sample of 977 Portuguese mothers of infants aged between zero and six months completed an online survey between December 2020 and January 2021, a period of major pandemic-related restrictions. The survey included several self-report questionnaires that assessed sociodemographic, clinical, and COVID-19 information, self-compassion, mindful parenting, PPDS and PPAS. Mothers who reported having felt that the pandemic had a negative emotional impact during their postpartum period (79.5%) presented lower levels of self-compassion and mindful parenting, and higher levels of PPDS and PPAS. Regarding the mediation model, higher levels of self-compassion were related to higher levels of mindful parenting, and this association was mediated by lower levels of PPAS. These results highlight the relevance of mothers’ self-compassion for helping them feel less anxious and to adopt a mindful way of parenting in the postpartum period, particularly during the pandemic. Compassion-based interventions may be particularly important in reducing PPAS and promoting mindful parenting and should be available to postpartum mothers, especially during, but also beyond the pandemic.
Similar content being viewed by others
Introduction
The COVID-19 Pandemic and Maternal Mental Health
During the last two years, the COVID-19 pandemic has had a biopsychosocial, spiritual, and economic global effect in population around the world (e.g., Tanhan et al., 2021). Over time, the pandemic went through different waves, characterized by periods when the number of patients with COVID-19 disease gradually increased. Many countries, including Portugal, have adopted social restrictive measures and lockdowns to control the number of newly infected patients (Oskovi-Kaplan et al., 2021). In Portugal, the periods of major pandemic-related restrictions occurred between March and May 2020 and between December 2020 and April 2021, including social physical distancing, lockdowns, the use of hygienic masks, the closure of schools and nonessential businesses such as cinemas and cafes, and the adoption of telework (Diário da República Eletrónico [DRE], 2020). Recent literature has shown that the pandemic and adopted restrictive measures are associated with an increased risk of mental health problems in the general population, especially in vulnerable groups, such as postpartum mothers (Baran et al., 2021; Fernandes et al., 2021b; Liu et al., 2021). Additionally, it is well-known that mental health problems, and specifically a mood disorder, generally predicts lower adherence to health care, including mental health care, which is essential during the postpartum period. Several predictors of nonadherence to treatment were identified, such as younger age (below 40 years old), comorbidity with substance use and personality disorders, patients’ beliefs, poor insight, illness severity, treatment-related side effects, specific features of the disease and a poor therapeutic alliance (Pompili et al., 2013), and all should be evaluated, to provide a more effective care, especially during a pandemic.
The postpartum requires particular attention since it is a period of increased vulnerability for mothers’ mental health. This period is characterized by major psychological and emotional changes, challenges, and new responsibilities (e.g., adaptation to the new role as a mother) (e.g., Keepanasseril et al., 2021), which may lead mothers to be more vulnerable to developing psychopathological symptoms. These symptoms can be exacerbated in stressful contexts such as the current pandemic (e.g., Harville et al., 2010). Despite the scarce literature, there is already evidence that the current pandemic has enhanced mental health problems during the postpartum period, leading to the development of maternal depressive and anxious symptoms (e.g., Chen et al., 2021; Davenport et al., 2020; Mariño-Narvaez et al., 2021). For instance, a study performed among postpartum mothers during the lockdown showed that mothers presented higher rates of depressive and anxious symptoms during the pandemic than in the prepandemic period (Suárez-Rico et al., 2021).
Maternal Mental Health and Mindful Parenting
It is well-established that maternal psychopathological symptoms have a negative impact on parenting practices and on the mother-infant relationship, as early as in the postpartum period. Mothers with depressive symptoms tend to adopt negative parenting behaviors and are less likely to be responsive (Lovejoy et al., 2000) and sensitive to their infant’s needs (Nath et al., 2019). Similarly, mothers with anxious symptoms typically exhibit more negative parenting behaviors (Crugnola et al., 2016) and present more impaired mother-infant bonding (Fallon et al., 2021; Tietz et al., 2014). Recently, a study developed by Fernandes et al. (2021a) showed a negative association between postpartum depressive symptoms (PPDS) and postpartum anxious symptoms (PPAS) with lower levels of mindful parenting.
Research in the field of maternal mental health and parenting during the pandemic is scarce. However, recent studies have shown that postpartum mothers with depressive symptoms present significantly less strong maternal attachment with their babies (Oskovi-Kaplan et al., 2021) and that mothers with anxious symptoms present more impaired mother-infant bonding (Provenzi et al., 2021). Additionally, mothers who gave birth during the pandemic were shown to present lower levels of the mindful parenting dimension pertaining to the ability to notice and be aware of one’s child’s emotions and more impaired bonding with their infant than those who gave birth before the pandemic (Fernandes et al., 2021b).
Mindful parenting is characterized by several parenting qualities or skills (Duncan et al., 2009), such as the ability to direct complete attention to the child and to be fully present during parent–child interactions (i.e., listening with full attention to the child); the ability to notice and correctly identify the child’s feelings and needs (i.e., emotional awareness of the child); the ability to adopt an attitude of nonjudgmental acceptance of the self as a parent and of the challenges of parenting (i.e., non-judgmental acceptance of parental functioning); the ability to self-regulate in parent–child interactions, in accordance with parenting values and goals (i.e., self-regulation in the parenting relationship); and the ability to be compassionate with the child, adopting a kind, sensitive and responsive attitude to the child’s needs (i.e., compassion for the child) (Caiado et al., 2020). In general, this parental approach allows parents to be better able to intentionally bring a nonjudgmental and present-centered awareness to everyday parent–child interactions (Bögels & Restifo, 2014; Kabat-Zinn & Kabat-Zinn, 1997). During the postpartum period, research on mindful parenting remains limited. A few studies have shown that postpartum mothers who engage in more mindful parenting practices tend to experience lower levels of parenting stress (Fernandes et al., 2021a) and that mindful parenting training can promote more positive mother-infant relationships (Potharst et al., 2017).
Therefore, considering the importance of parenting practices in the first year of life and their profound long-term effects on a child’s social, cognitive, and emotional development (Kirby, 2017), further studies are needed to better understand psychological resources that may reduce maternal psychopathological symptoms and promote a more adaptative parenting, particularly during a pandemic.
Self-compassion
An individual psychological resource (Neff & Germer, 2013) that has been associated with better maternal mental health and parenting, during the postpartum period, is self-compassion (e.g., Fernandes et al., 2021c). In general, self-compassion can be characterized by an attitude of kindness toward one’s suffering and the desire to relieve it (Neff, 2003, 2009; Neff, & Vonk, 2009), and more specifically it involves three interactive bipolar components: (1) self-kindness versus self-judgment, (2) mindfulness versus overidentification and (3) common humanity versus isolation (Neff et al., 2019). This adaptative way of self-to-self relating, characterized by an attitude of care, and understanding toward oneself, the capacity of being aware of one’s painful experiences and the recognition that all human beings are imperfect and suffer, can be highly beneficial for mothers experiencing postpartum challenges.
The literature on the role of self-compassion on maternal mental health in the postpartum period is growing, and there is emerging evidence that self-compassion can be considered an emotional regulation strategy during this period (Pedro et al., 2019), that has a positive and significant impact on maternal mental health. For instance, a study developed by Monteiro et al. (2019) and a study developed by Felder et al. (2016), both conducted with postpartum mothers, indicated that self-compassion was negatively associated with PPDS and PPAS. During the pandemic, several studies conducted among the general population have suggested an association between higher level of self-compassion and lower levels of depressive, anxious and stress symptoms (e.g., Gutiérrez-Hernández et al., 2021). However, the relationship between self-compassion and the negative impact of the COVID-19 pandemic, in terms of mental health, remains to be explored, in postpartum mothers.
Additionally, self-compassion is also associated with positive results in parenting, among parents of children and adolescents, such as less parenting stress, improved children’s well-being (Moreira et al., 2015), and higher levels of mindful parenting (Nguyen et al., 2020). Additionally, parents reporting higher levels of self-compassion were found to be less critical and to use fewer distressed reactions to cope with their children’s emotions (Psychogiou et al., 2016). In contrast, lower levels of self-compassion were associated with poor parenting (e.g., low warmth, high overprotection, and high rejection) (Pepping et al., 2015) and higher childhood emotional abuse, emotional neglect, and physical abuse (Tanaka et al., 2011). During the postpartum period, self-compassion and parenting has been scarcely investigated, however there is evidence that self-compassion was associated with higher levels of mindful parenting among mothers of infants (Fernandes et al., 2021b).
Overall, it is well-established that self-compassion is associated with a mindful parenting style, however this relationship may be explained by several variables. It is essential to identify the variables that can influence this association, to devise more effective screening and intervention strategies that may help mothers better cope with the postpartum period and parenting during and beyond the pandemic. Since maternal psychopathological symptoms, such as PPDS and PPAS, have a great interference in parenting, and that self-compassion may promote maternal mental health (that is reducing psychopathological symptoms) it is plausible to consider that such variables may explain the association between self-compassion and mindful parenting. However, these associations remain unexplored during the postpartum period and the current pandemic.
The Current Study
Therefore, the current study had two main goals. First, we aimed to compare mothers who experienced and mothers who did not experience a negative emotional impact of COVID-19 on self-compassion, mindful parenting, PPDS and PPAS. Second, we aimed to explore whether mothers’ self-compassion was associated with mindful parenting and whether this relationship was mediated by psychopathological symptoms, such as PPDS and PPAS. Based on the literature reviewed, we expect mothers with higher levels of self-compassion to present lower levels of psychopathological symptoms (depressive and anxious symptoms), which, in turn, will be associated with higher levels of mindful parenting.
Methods
Participants
The sample included 977 Portuguese mothers of infants aged between zero and six months. As presented in Table 1, most mothers had completed higher education, were employed and were currently on maternity leave. Most mothers were tested for COVID-19 before childbirth and were not infected by the virus. Also, most mothers reported having felt a negative emotional impact from the pandemic during the postpartum period (79.5%). About 5.4% of mothers were currently under psychological and/or psychiatric treatment; these mothers were not excluded from the present study since this variable was controlled in the mediation model. The complete sociodemographic, clinical, and COVID-19-related information of the mothers is presented in Table 1.
Procedure
This study is a cross-sectional study conducted between December 2020 and January 2021, which corresponds to a period of major restrictions in Portugal (state of national emergency). The sample was recruited online through a data collection website (LimeSurvey®) after approval from the Ethics Committee (blind for review). The survey link was shared through e-mail, unpaid cross-posting, and paid boosting campaigns. Several advertisements explaining the main goals of the study and presenting the inclusion criteria and the web link to the survey were posted on a Facebook page and an Instagram page about parenting and mental health, as well as on social networks, including Facebook pages about parenting issues after the birth of a child and parenting forums. Participants who clicked on the link were then given detailed information about the study, namely, a description of the objectives, the inclusion criteria, and the ethical statement of the study. Participants were informed that their participation was voluntary and anonymous.
Participants were eligible for the study if they fulfilled the following inclusion criteria: (i) were Portuguese; (ii) were over 18 years old; and (iii) had at least one child aged between zero and six months. Only those who agreed to the study conditions and who provided their informed consent by clicking on the option “I understand and accept the conditions of the study” completed the assessment protocol. Of the 1456 mothers who participated in this study, 434 mothers were excluded because one or more of the study questionnaires were not completed, 25 women were excluded because their babies were more than six months old, and 20 women were excluded because of their nationality (they were not Portuguese). Therefore, 977 participants completed all the questionnaires and were included in the present study.
Measures
Sociodemographic, Clinical and COVID-19-related Information
The first part of the online survey included a standard sociodemographic information form (e.g., age, marital status) and a clinical data form (e.g., obstetric information and history of psychopathological problems). It also included a question about COVID-19 diagnosis before childbirth (infected with COVID-19 versus not infected with COVID-19) and a question about the perceived negative emotional impact of the pandemic (“Do you consider that the current pandemic had a negative impact on your emotional well-being during the postpartum period?”) [yes or no]).
Self-compassion
To assess mothers’ self-compassion, the short version of the Portuguese version of the Self-Compassion Scale (SCS-SF; Castilho et al., 2015; Raes et al., 2011) was used. The SCS-SF comprises 12 items (e.g., “When I’m going through a very hard time, I give myself the caring and tenderness I need”) answered on a five-point response scale, ranging from 1 (almost never) to 5 (almost always). The total score may be calculated by estimating the mean of the 12 items, with higher scores indicating higher levels of self-compassion. The Portuguese version of the SCS-SF has demonstrated good psychometric qualities. In the present sample, the Cronbach’s alpha coefficient was 0.88.
Mindful Parenting
To assess mindful parenting among mothers of infants, the infant version of the Portuguese Interpersonal Mindfulness in Parenting Scale (IM-P—Infant version; Caiado et al., 2020; Duncan, 2007) was used. This scale contains 28 items, answered on a five-point response scale, ranging from 1 (never true) to 5 (always true). The total score is the sum of the items, and higher scores indicate higher levels of mindful parenting. In the current sample, Cronbach’s alpha coefficient was 0.85.
Postpartum Depressive Symptoms
To assess depressive symptoms in the postpartum period, the Portuguese version of the Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987; Figueiredo, 1997) was used. The EPDS contains 10 items, in women are asked to rate their emotions (e.g., sadness, anxiety) over the previous seven days using a four-point response scale. Higher scores were indicative of higher depressive symptoms. In the Portuguese validation studies (Figueiredo, 1997), a score of 10 or higher was found to be indicative of clinically relevant depressive symptoms. In our sample, Cronbach's alpha was 0.89.
Postpartum Anxious Symptoms
To assess anxious symptoms, specifically the frequency of maternal and infant-related anxieties specific to the first six months postpartum experienced during the previous seven days, the Postpartum Specific Anxiety Scale (PSAS; Fallon et al., 2016) was used. The original version of this scale was used, after translation to Portuguese language. This scale contains 51 items, answered in four-point response scale ranging from 1 (not at all) to 4 (almost always). Its original structure comprises four factors: “Maternal Competence and Attachment Anxieties”; “Infant Safety and Welfare Anxieties”; “Practical Infant Care Anxieties”; and “Psychosocial Adjustment to Motherhood”. The total score is the sum of the items, with higher scores being indicative of higher anxious symptoms. A score of 112 or higher is indicative of clinically relevant anxious symptoms. In our sample, Cronbach's alpha was 0.94.
Data Analyses
Data analyses were conducted using the Statistical Package for the Social Sciences (IBM SPSS, version 25.0) and the macro-PROCESS for SPSS (Hayes, 2013). Descriptive statistics were computed for all sociodemographic and study variables. Cronbach’s alpha coefficient measured the internal consistency of the instruments. Pearson correlations between the study variables were computed. Cohen’s guidelines (1988) were used to describe and interpret the effect sizes of correlations (i.e., a small effect size for correlations close to 0.10, medium effect size for correlations near 0.30, and strong effect size for correlations 0.50 or higher). One-way ANOVAs were used to compare self-compassion, mindful parenting, PPDS and PPAS as a function of mothers’ perceived negative emotional impact of the pandemic (yes or no), and we used chi-squared tests to compare categorical variables, as a function of mothers’ perceived negative emotional impact of the pandemic. Effect sizes were presented for all analyses as eta-squared (small: η2p ≥ 0.01; medium: η2p≥ 0.06, and large: η2p≥ 0.14).
A mediation model (Model 4; Hayes, 2013) was estimated to test whether self-compassion (independent variable) was associated with mindful parenting (dependent variable) through postpartum depressive and anxious symptoms (mediator variables). To identify possible covariates that should be introduced into the mediation model, Pearson’s and point-biserial correlations between the mediator and the dependent variable and sociodemographic, clinical, and COVID-19-related information were also computed. A bootstrapping procedure using 10,000 resamples was used to assess the indirect effect. This procedure creates 95% bias-corrected and accelerated confidence intervals (95% BCaCIs) of indirect effects, which are considered significant when zero is not contained within the lower and upper CIs.
Results
Comparative Analyses and Correlations among the Study Variables
Approximately 38.2% (n = 373) of the mothers reported clinically significant levels of depressive symptoms (i.e., scored ≥ 10 on EPDS), and 47.5% (n = 464) reported clinically significant anxious symptoms (i.e., scored ≥ 112 on PSAS).
Firstly, to control confounding effects, we have explored if there were differences in sociodemographic variables as a function of mother’s perceived emotional impact of the pandemic. No differences were found in any variable.
Significant differences were found as a function of perceived emotional impact of the pandemic in self-compassion (F(1, 976) = 19.36, p < 0.001, η2p = 0.04), mindful parenting (F(1, 976) = 18.67, p = < 0.001, η2p = 0.02), depressive symptoms (F(1, 976) = 130.05, p < 0.001, η2p = 0.12), and anxious symptoms (F(1, 976) = 99.15, p < 0.001, η2p = 0.09), with mothers who reported having felt that the pandemic had a negative emotional impact during postpartum presenting lower levels of self-compassion and mindful parenting and higher levels of depressive and anxious symptoms (see Table 2).
Correlations between the study variables are presented in Table 2. Self-compassion was significantly and positively correlated with mindful parenting and negatively correlated with depressive symptoms and anxious symptoms; mindful parenting was significantly and negatively correlated with depressive symptoms and anxious symptoms; and depressive symptoms were significantly and positively correlated with anxious symptoms. The correlation between mindful parenting and depressive symptoms had a medium effect size, and all other correlations were strong.
The Indirect Effect of Mothers’ Self-compassion on Mindful Parenting through Postpartum Depressive and Anxious Symptoms
Prior to mediation analyses, Pearson’s and point-biserial correlations between sociodemographic, clinical, and COVID-19 variables and PPDS, PPAS, and mindful parenting were analyzed to determine whether any variable should be introduced in the model as a covariate.
Significant correlations were found between babies’ ages and anxious (r = 0.094, p = 0.003) and depressive symptoms (r = 0.140, p < 0.001); mothers’ education (0 = basic and secondary education and 1 = higher education) and anxious (rpb = -0.131, p < 0.001) and depressive symptoms (rpb = -0.154, p < 0.001); household monthly income (0 = less than 2000€ and 1 = 2000€ or above) and anxious (rpb = -0.116, p < 0.001) and depressive symptoms (rpb = -0.082, p = 0.010); current psychological or psychiatric treatment (0 = no; 1 = yes) and anxious (rpb = 0.110, p = 0.001) and depressive symptoms (rpb = 0.134, p < 0.001); parity (0 = primiparous and 1 = multiparous) and anxious symptoms (rpb = -0.217, p < 0.001); and mindful parenting (rpb = -0.064, p = 0.045). Therefore, babies’ age, mothers’ education, household monthly income, current psychological and/or psychiatric treatment and parity, and were introduced as covariates into the regression model.
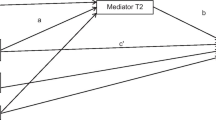
As presented in Fig. 1, self-compassion was significantly and negatively associated with depressive symptoms (b = -4.14, p < 0.001) and, along with the covariates, explained 37.56% of its variance. Self-compassion was significantly and negatively associated with anxious symptoms (b = -16.91, p < 0.001) and, along with the covariates, explained 37.94% of its variance. The total model explained 33.24% of the mindful parenting variance. Although depressive symptoms were not significantly associated with mindful parenting (b = -0.13, p = 0.114), higher levels of self-compassion (b = 6.01, p < 0.001) and lower levels of anxious symptoms (b = -0.19, p < 0.001) significantly predicted higher levels of mindful parenting. All paths for the full process model, as well as unstandardized regression coefficients, are illustrated in Fig. 1.
Statistical diagram of the mediation model for the presumed influence of postpartum depressive symptoms and postpartum anxious symptoms on the association between self-compassion and mindful parenting. Note. Path values represent unstandardized regression coefficients. In the arrow linking self-compassion and mindful parenting, the value outside the parentheses represents the total effect model of self-compassion on mindful parenting after the inclusion of the mediators. The value in parentheses represents the direct effect from the bootstrapping analysis of self-compassion on mindful parenting after the inclusion of the mediators. Babies’ age, household monthly income, mothers’ education, parity, and current psychological and/or psychiatric treatment were introduced as covariates into the regression model. For simplicity, these covariates are not shown in the figure.*p < 0.001
While the total effect (9.81; 95% BCaCIs = 8.92/10.70) and direct effect (6.01; 95% BCaCIs = 4.95/7.07) of self-compassion on mindful parenting were significant, the indirect effect was not found through depressive symptoms (estimated value = 0.55 (95% BCaCIs = -0.13/1.20)), as presented in Table 3. On the other hand, self-compassion was found to be indirectly associated with mindful parenting through anxious symptoms, with an estimated value of 3.25 (95% BCaCIs = 2.50/4.12) (see Table 3).
Discussion
Overall, the present study indicated that mothers who reported having felt that the pandemic had a negative emotional impact during their postpartum period (79.5%) presented lower levels of self-compassion and mindful parenting, and higher levels of PPDS and PPAS. Regarding the mediation model, higher levels of self-compassion were related to higher levels of mindful parenting, and this association was mediated by lower levels of PPAS.
First, most mothers reported having felt a negative emotional impact from the pandemic during the postpartum period (79.5%). These mothers presented lower levels of self-compassion and mindful parenting than mothers who reported not having felt a negative emotional impact from the pandemic. One possible explanation for these mothers having lower levels of self-compassion is that their threat regulation system might be more easily activated due to the pandemic. When the threat system is activated, it prevents mothers from activating the affiliation/soothing system, which would enable them to feel calm, content, and soothed (Gilbert, 2009) and adopt a kind and compassionate attitude toward themselves. Additionally, having their threat system more easily activated may lead mothers to focus their attention on threats, fears, and their own negative emotions, which may not allow them to disconnect from their own thoughts and be fully attentive to their infant’s signals, emotions and needs. Consequently, these mothers may be less able to respond sensitively to their baby, to regulate themselves in mother-infant interactions, and to adopt a mindful parenting approach (Duncan et al., 2009).
Additionally, mothers who reported felt a negative emotional impact from the pandemic during the postpartum period presented higher levels of PPDS and PPAS, which is in accordance with other recent studies, suggesting that changes and uncertainty triggered by the pandemic and pandemic-related measures, may have had a psychological impact on the population's mental well-being, and that is associated with an increase of psychopathological symptoms, such as depressive and anxious symptoms (e.g., Killgore et al., 2020; Lima et al., 2020).
Second, our results indicated that higher levels of self-compassion predicted higher levels of mindful parenting and that this association was mediated by lower levels of PPAS. As expected and consistent with previous literature (e.g., Moreira et al., 2016), self-compassion was positively associated with mindful parenting. As described in the present study, self-compassion is a multicomponent construct comprised of three interactive bipolar components: self-kindness versus self-judgment, mindfulness versus overidentification, and common humanity versus isolation (Neff et al., 2019). Therefore, our results may suggest that mothers who are more self-compassionate have higher levels of self-kindness, so they adopt a more caring and supportive attitude toward themselves, their failures, and their suffering, including in their parenting. This may facilitate the adoption of a kinder way of parenting since they are less critical regarding their parenting behaviors (e.g., Gouveia et al., 2016). Additionally, self-compassionate mothers have a greater capacity to be aware of their own painful experiences in a balanced manner and adopt a more mindful and accepting attitude toward their emotions and thoughts, which may help them to be more easily aware of their infant’s emotional states and behaviors and then provide them responsive and sensitive responses in a mindful way. Furthermore, it can be stated that self-compassionate mothers have a greater sense of common humanity, which can help them to recognize that all human beings are imperfect, fail, and suffer and to accept, in a nonjudgmental way, their limitations as mothers. This may facilitate the adoption of a more accepting and nonjudgmental approach in their parenting (e.g., Moreira et al., 2016). Thus, all these self-compassion components may facilitate the adoption of a mindful approach to parenting.
Moreover, self-compassion was associated with lower psychopathological symptoms, such as PPDS and PPAS, which is in accordance with previous studies during the postpartum period (e.g., Monteiro et al., 2019). This result may be explained by several factors. First, mothers with higher levels of self-compassion are better able to activate the soothing system of affect regulation (Gilbert, 2014), which may help them to better regulate their negative emotions and, for instance, feel less negatively affected by the challenges of parenting (e.g., Gouveia et al., 2016). Additionally, it can be hypothesized that self-compassionate mothers cope with challenging emotions with a greater degree of understanding, self-directed care, and support, which may lead them to experience lower levels of psychopathological symptoms (Pauley & McPherson, 2010). In addition, self-compassionate mothers are kinder to themselves and experience a higher sense of common humanity, which may lead them to feel less isolated, especially during a pandemic context, and less self-judgmental (Singh & Sharma, 2020), which may prevent them from experiencing depressive and anxious symptoms.
Although self-compassion is positively associated with mindful parenting and negatively associated with depressive and anxious symptoms, our results indicated that the indirect effect of self-compassion on mindful parenting happens only through PPAS and not through PPDS. Therefore, it seems that having higher levels of self-compassion may be associated with a decrease in anxious symptoms related to parenting and mother-infant relationship during the postpartum period, which, in turn, facilitates the adoption of a mindful approach in parenting but not a decrease in maternal depressive symptoms. These results can be understood considering several issues.
First, a postpartum period-specific scale was used to measure mothers’ anxious symptoms; therefore, specific postpartum issues were assessed, such as competence and attachment anxieties, infant safety and welfare anxieties, practical baby care anxieties and psychosocial adjustment to motherhood (Fallon et al., 2016). In contrast, the EPDS was used to assess depressive symptoms, which is a measure that only contains general questions to assess mothers’ depressive levels. The difference between the specificity levels of these measures may have influenced the results.
Second, research has suggested a distinct neurobiological pattern for anxious and depressive symptoms when they occur during the peripartum period compared with other times during a woman's life (Pawluski et al., 2017). Regarding anxious symptoms, from an evolutionary perspective, it can be stated that individuals who could quickly detect potential threats and react automatically were more likely to survive and adopting a reactive and anxious parenting style may have helped our ancestors survive and protect their children. This fast and automatic reaction to perceived threats was clearly advantageous in the evolutionary past, when life was characterized by several threats (LeDoux, 1996). Currently, we may suppose that a pandemic context can be felt as an environment with great threats for mothers, leading them to feel more anxious in their parenting and in taking care of their vulnerable infants. In a different way, depressive symptoms are associated with a lack of cognitive control over emotional states (Messina et al., 2016), which may result in a ruminative way of thinking, lack of energy, inability to concentrate, feelings of worthlessness or excessive guilt, and a loss of pleasure or interest in things a person used to enjoy (American Psychological Association [APA], 2014). During the pandemic, it seems that self-compassion facilitates the adoption of a mindful parenting approach by specifically “slowing down” the threat response of the mother’s brain, especially those related to parenting situations and mother-infant relationships, instead of reducing individual symptoms, such as maternal depressive symptoms.
Finally, in general, anxious, and depressive symptoms may be distinguished considering time orientation; that is, it seems that mothers who experience anxious symptoms are future-oriented and focus on threats (APA, 2021), whereas depressive mothers are tied to past events (Dobson, 1985). It may be hypothesized that during a pandemic, especially during a period of major pandemic-related restrictions, self-compassion may help mothers implement a more accepting, emotionally attuned and compassionate approach to parenting by 1) helping mothers be in the present moment instead of worrying about the future; 2) by promoting a more accepting attitude toward their failures as mothers; and 3) by reducing anxieties related to practical infant care tasks and their protection, more than helping them focus on past events.
Limitations
This study presents several limitations that should be mentioned. First, the sample was collected online, which may compromise the representativeness of the sample. This method of data collection if often associated with self-selection bias because participants who participated in the study were likely to be more motivated to participate and interested in parenting and mental health subject, than those in the general population. Second, this study included only mothers, which limits the generalization of these results to fathers. Third, the validity of the results can be compromised because only self-reported instruments were used to assess the study variables. Participants may be influenced by social desirability and their answers may not reflect their feelings or thoughts in a reliable way. Forth, a postpartum period-specific scale was used to measure mothers’ anxious symptoms and, in contrast, a measure that only contains general questions was used to assess mothers’ depressive levels, which may have influenced the results. Finally, this study has a cross-sectional design, therefore, a causal relationship cannot be inferred between self-compassion and mindful parenting. Future longitudinal studies would be needed to better understand if self-compassion effectively promotes the development of a mindful parenting approach and whether maternal psychopathological symptoms may interfere in this relationship over time.
Implications
Despite limitations previously presented, we may draw some suggestions and implications to several areas. First, regarding future research, the present study provides an innovative contribution to research in the field of the postpartum period during the COVID-19 pandemic, contributing to the understanding of the interrelationship between self-compassion, mental health, and parenting, during the pandemic. Future research may focus, for instance, in other mechanisms, through which self-compassion may exert an effect in mindful parenting. Also, other effective research methodologies should be considered, for instance qualitative, and they should be compared with mixed- or quantitative methods. For instance, Online Photovoice (OPV; Tanhan & Strack, 2020) seemed to be a very useful and effective qualitative research methodology, already used during the current pandemic (e.g., Tanhan, 2020). Moreover, collaborative efforts such as community-based participatory research (CBPR) methods can be used to explore the causes and effects of the negative emotional impact of the COVID-19 pandemic on self-compassion and mindful parenting, in collaboration with populations most impacted by it, such as postpartum mothers (e.g., Dari et al., 2021).
Second, regarding implications for professionals and mental health services, our results indicated that, in clinical practice, it is relevant to promote mothers’ self-compassion since this psychological resource may help them feel less anxious during the postpartum period and to adopt a mindful way of parenting toward their infant. The results highlighted the need of mental health professionals distinguish anxious from depressive symptoms, and to provide appropriate treatments that target specific symptoms and etiologies (Milgrom et al., 1999). Also, it seems important that psychological interventions focus on individual-related variables, such as on managing anxious symptomatology and promoting self-compassion, since they have influence on parenting-related variables. Compassion-based interventions applied to the postpartum period (e.g., Cree, 2015; Potharst et al., 2017) may be particularly important in reducing PPAS and promoting mindful parenting skills and should be available to postpartum mothers during and beyond the pandemic. Currently, given the pandemic constraints, the use of e-mental health will improve care access (Chen et al., 2021) and may be an important alternative to conventional interventions. The intervention developed by Potharst et al. (2019), a web-based mindful and compassionate parenting intervention, may be particularly important in promoting self-compassion, reducing maternal psychopathology, and promoting mindful parenting skills.
To conclude, these results corroborate the idea that self-compassion is a healthy way to relate to oneself, with impact in maternal mental health, and then, in parenting practices. Therefore, low-cost, and easily accessible programs (e.g., Potharst et al., 2019) may be implemented in primary healthcare services as early interventions focused on promoting self-compassion skills, to promote maternal mental health and a mindful and compassionate parenting, to all mothers during the postpartum period.
Data Availability
The data that support the findings of this study are not publicly available because them containing information that could compromise participant’s privacy/consent. The data are available on reasonable request from the corresponding author [DVF].
References
APA. (2014). Diagnostic and statistical manual of mental disorders (5th ed). Arlington, VA.
APA. (2021). Anxiety. In APA Dictionary of Psychology.
Baran, J., Leszczak, J., Baran, R., Biesiadecka, A., Weres, A., Czenczek-Lewandowska, E., & Kalandyk-Osinko, K. (2021). Prenatal and postnatal anxiety and depression in mothers during the COVID-19 pandemic. Journal of Clinical Medicine, 10(14). https://doi.org/10.3390/jcm10143193.
Bögels, S., & Restifo, K. (2014). Mindful parenting: A guide for mental health practitioners. Springer Science.
Caiado, B., Fernandes, D. V., Moreira, H., & Canavarro, M. C. (2020). The Interpersonal Mindfulness in Parenting Scale - Infant Version: Psychometric properties and factor structure in a sample of portuguese mothers in the postpartum period. Psychologica, 63(2), 139–157. https://doi.org/10.14195/1647-8606_63-2_7
Castilho, P., Pinto-Gouveia, J., & Duarte, J. (2015). Evaluating the multifactor structure of the long and short versions of the Self-Compassion Scale in a clinical sample. Journal of Clinical Psychology, 71(9), 856–870. https://doi.org/10.1002/jclp.22187
Chen, H., Selix, N., & Nosek, M. (2021). Perinatal anxiety and depression during COVID-19. The Journal for Nurse Practitioners, 17(1), 26–31. https://doi.org/10.1016/j.nurpra.2020.09.014
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.) Lawrence Erlbaum Associates.
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150, 782–786. https://doi.org/10.1192/bjp.150.6.782
Cree, M. (2015). The compassionate mind approach to postnatal depression: Using compassion focused therapy to enhance mood, confidence and bonding. Hachette UK.
Crugnola, R. C., Ierardi, E., Ferro, V., Gallucci, M., Parodi, C., & Astengo, M. (2016). Mother-infant emotion regulation at three months: The role of maternal anxiety, depression and parenting stress. Psychopathology, 49(4), 285–294. https://doi.org/10.1159/000446811
Dari, T., Chan, C., & Del Re, J. (2021). Integrating culturally responsive group work in schools to foster the development of career aspirations among marginalized youth. Journal for Specialists in Group Work, 46(1), 75–89. https://doi.org/10.1080/01933922.2020.1856255
Davenport, M., Meyer, S., Meah, V., Strynadka, M., & Khurana, R. (2020). Moms are not OK: COVID-19 and maternal mental health. Frontiers in Global Women's Health, 1.https://doi.org/10.3389/fgwh.2020.00001.
Dobson, K. S. (1985). The relationship between anxiety and depression. Clinical Psychology Review, 5(4), 307–324. https://doi.org/10.1016/0272-7358(85)90010-8
DRE (2020). Decreto n.º 11-A/2020. Retrieved from https://dre.pt/pesquisa/-/search/151904698/details/maximized.
Duncan, L. G. (2007). Assessment of mindful parenting among parents of early adolescents: Development and validation of the Interpersonal Mindfulness in Parenting scale [Doctoral Dissertation, The Pennsylvania State University]. Pennsylvania.
Duncan, L. G., Coatsworth, J. D., & Greenberg, M. T. (2009). A model of mindful parenting: Implications for parent-child relationships and prevention research. Clinical Child and Family Psychology Review, 12(3), 255–270. https://doi.org/10.1007/s10567-009-0046-3
Fallon, V., Halford, J. C. G., Bennett, K. M., & Harrold, J. A. (2016). The Postpartum Specific Anxiety Scale: Development and preliminary validation. Archives of Women Mental Health, 19(6), 1079–1090. https://doi.org/10.1007/s00737-016-0658-9
Fallon, V., Silverio, S., Halford, J. C. G., Bennett, K. M., & Harrold, J. A. (2021). Postpartum-specific anxiety and maternal bonding: Further evidence to support the use of childbearing specific mood tools. Journal of Reproductive and Infant Psychology, 39(2), 114–124. https://doi.org/10.1080/02646838.2019.1680960
Felder, J., Lemon, E., Shea, K., Kripke, K., & Dimidjian, S. (2016). Role of self-compassion in psychological well-being among perinatal women. Archives of Women Mental Health, 19(4), 687–690. https://doi.org/10.1007/s00737-016-0628-2
Fernandes, D. V., Canavarro, M. C., & Moreira, H. (2021a). The mediating role of parenting stress in the relationship between anxious and depressive symptomatology, mothers’ perception of infant temperament, and mindful parenting during the postpartum period. Mindfulness, 12, 275–290. https://doi.org/10.1007/s12671-020-01327-4
Fernandes, D. V., Canavarro, M. C., & Moreira, H. (2021b). Postpartum during COVID-19 pandemic: Portuguese mothers’ mental health, mindful parenting and mother-infant bonding. Journal of Clinical Psychology, 77(9), 1997–2010. https://doi.org/10.1002/jclp.23130
Fernandes, D. V., Canavarro, M. C., & Moreira, H. (2021c). The role of mothers’ self-compassion on mother-infant bonding during the COVID-19 pandemic: A longitudinal study exploring the mediating role of mindful parenting and parenting stress in the postpartum period. Infant Mental Health Journal, 42(5), 621–635. https://doi.org/10.1002/imhj.21942
Figueiredo, B. (1997). Depressão pós-parto, interação mãe-bebê e desenvolvimento infantil [Dissertação de Doutoramento não publicada]. Universidade do Minho.
Gilbert, P. (2009). The compassionate mind. Hachette.
Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53(1), 6–41. https://doi.org/10.1111/bjc.12043
Gouveia, M. J., Carona, C., Canavarro, M. C., & Moreira, H. (2016). Self-compassion and dispositional mindfulness are associated with parenting styles and parenting stress: The mediating role of mindful parenting. Mindfulness, 7(3), 700–712. https://doi.org/10.1007/s12671-016-0507-y
Gutiérrez-Hernández, M., Fanjul, L., Díaz-Megolla, A., Reyes-Hurtado, P., Herrera-Rodríguez, J., Enjuto-Castellanos, M., & Peñate, W. (2021). COVID-19 lockdown and mental health in a sample population in Spain: The role of self-compassion. International Journal of Environmental Research and Public Health, 18(4). https://doi.org/10.3390/ijerph18042103
Harville, E., Xiong, X., & Buekens, P. (2010). Disasters and perinatal health: A systematic review. Obstetrical & Gynecological Survey, 65(11), 713–728. https://doi.org/10.1097/OGX.0b013e31820eddbe
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. The Guilford Press.
Kabat-Zinn, M., & Kabat-Zinn, J. (1997). Everyday blessings: The inner work of mindful parenting. Hachette.
Keepanasseril, A., Singh, S., & Bharadwaj, B. (2021). Postpartum mental health status & role transition to mother in primigravid women: A cross-sectional study. Journal of Reproductive and Infant Psychology, 1-10. https://doi.org/10.1080/02646838.2021.1952552.
Killgore, W. D., Taylor, E. C., Cloonan, S. A., & Dailey, N. S. (2020). Psychological resilience during the COVID-19 lockdown. Psychiatry Research, 291. https://doi.org/10.1016/j.psychres.2020.113216.
Kirby, J. N. (2017). Compassion-focused parenting. In E. M. Seppälä, E. Simon-Thomas, S. L. Brown, M. C. Worline, C. D. Cameron, & J. R. Doty (Eds.), The Oxford Handbook of Compassion Science (pp. 91–105). Oxford University Press.
LeDoux, J. E. (1996). The emotional brain: The mysterious underpinnings of emotional life. Simon & Schuster.
Lima, C. K. T., Carvalho, P. M., Lima, I., Nunes, J., Saraiva, J., Souza, R., Silva, C., & Neto, M. (2020). The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Research, 287. https://doi.org/10.1016/j.psychres.2020.112915.
Liu, C., Erdei, C., & Mittal, L. (2021). Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Research, 295. https://doi.org/10.1016/j.psychres.2020.113552.
Lovejoy, M. C., Graczyk, P. A., O’Hare, E., & Neuman, G. (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20(5), 561–592. https://doi.org/10.1016/s0272-7358(98)00100-7
Mariño-Narvaez, C., Puertas-Gonzalez, J., Romero-Gonzalez, B., & Peralta-Ramirez, M. (2021). Giving birth during the COVID-19 pandemic: The impact on birth satisfaction and postpartum depression. International Journal of Gynecology & Obstetrics, 153(1), 83–88. https://doi.org/10.1002/ijgo.13565
Messina, I., Bianco, F., Cusinato, M., Calvo, V., & Sambin, M. (2016). Abnormal default system functioning in depression: Implications for emotion regulation. Frontiers in Psychology, 7(858). https://doi.org/10.3389/fpsyg.2016.00858.
Milgrom, J., Martin, P., & Negri, L. (1999). Treating postnatal depression. New York.
Monteiro, F., Fonseca, A., Pereira, M., Alves, S., & Canavarro, M. C. (2019). What protects at-risk postpartum women from developing depressive and anxiety symptoms? The role of acceptance-focused processes and self-compassion. Journal of Affective Disorders, 246, 522–529. https://doi.org/10.1016/j.jad.2018.12.124
Moreira, H., Carona, C., Silva, N., Nunes, J., & Canavarro, M. C. (2016). Exploring the link between maternal attachment-related anxiety and avoidance and mindful parenting: The mediating role of self-compassion. Psychology & Psychotherapy: Theory, Research & Practice, 89(4), 369–384. https://doi.org/10.1111/papt.12082
Moreira, H., Gouveia, M. J., Carona, C., Silva, N., & Canavarro, M. C. (2015). Maternal attachment and children’s quality of life: The mediating role of self-compassion and parenting stress. Journal of Child & Family Studies, 24(8), 2332–2344. https://doi.org/10.1007/s10826-014-0036-z
Nath, S., Pearson, R. M., Moran, P., Pawlby, S., Molyneaux, E., Challacombe, F., & Howard, L. (2019). The association between prenatal maternal anxiety disorders and postpartum perceived and observed mother-infant relationship quality. Journal of Anxiety Disorders, 68. https://doi.org/10.1016/j.janxdis.2019.102148.
Neff, K. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860390209035
Neff, K. (2009). Self-Compassion. In M. Leary & R. Hoyle (Eds.), Handbook of individual differences in social behavior (pp. 561–573). The Guilford Press.
Neff, K., & Vonk, R. (2009). Self-compassion versus global self-esteem: Two different ways of relating to oneself. Journal of Personality, 77(1), 23–50. https://doi.org/10.1111/j.1467-6494.2008.00537.x
Neff, K., & Germer, C. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69(1), 28–44. https://doi.org/10.1002/jclp.21923
Neff, K., Tóth-Király, I., Yarnell, L., Arimitsu, K., Castilho, P., Ghorbani, N., Guo, H., Hirsch, J., Hupfeld, J., & Hutz, C. (2019). Examining the factor structure of the Self-Compassion Scale in 20 diverse samples: Support for use of a total score and six subscale scores. Psychological Assessment, 31(1), 27–45. https://doi.org/10.1037/pas0000629
Nguyen, T. M., Bui, T., Xiao, X., & Le, V. H. (2020). The influence of self-compassion on mindful parenting: A mediation model of gratitude. The Family Journal. https://doi.org/10.1177/1066480720950421
Oskovi-Kaplan, Z. A., Buyuk, G., Ozgu-Erdinc, A. S., Keskin, H. L., Ozbas, A., & Moraloglu Tekin, O. (2021). The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: A preliminary study. Psychiatric Quarterly, 92(2), 675–682. https://doi.org/10.1007/s11126-020-09843-1
Pauley, G., & McPherson, S. (2010). The experience and meaning of compassion and self-compassion for individuals with depression or anxiety. Psychology and Psychotherapy: Theory, Research and Practice, 83(2), 129–143. https://doi.org/10.1348/147608309X471000
Pawluski, J. L., Lonstein, J. S., & Fleming, A. S. (2017). The neurobiology of postpartum anxiety and depression. Trends in Neurosciences, 40(2), 106–120. https://doi.org/10.1016/j.tins.2016.11.009
Pedro, L., Branquinho, M., Canavarro, M. C., & Fonseca, A. (2019). Self-criticism, negative automatic thoughts and postpartum depressive symptoms: The buffering effect of self-compassion. Journal of Reproductive and Infant Psychology, 37(5), 539–553. https://doi.org/10.1080/02646838.2019.1597969
Pepping, C., Davis, P., O’Donovan, A., & Pal, J. (2015). Individual differences in self-compassion: The role of attachment and experiences of parenting in childhood. Self and Identity, 14(1), 104–117. https://doi.org/10.1080/15298868.2014.955050
Pompili, M., Venturini, P., Palermo, M., Stefani, H., Seretti, M. E., Lamis, D., Serafini, G., Amore, M., & Girardi, P. (2013). Mood disorders medications: Predictors of nonadherence: Review of the current literature. Expert Review of Neurotherapeutics, 13(7), 809–825. https://doi.org/10.1586/14737175.2013.811976
Potharst, E., Aktar, E., Rexwinkel, M., Rigterink, M., & Bögels, S. (2017). Mindful with your baby: Feasibility, acceptability, and effects of a mindful parenting group training for mothers and their babies in a mental health context. Mindfulness, 8(5), 1236–1250. https://doi.org/10.1007/s12671-017-0699-9
Potharst, E., Boekhorst, M., Cuijlits, I., van Broekhoven, K., Jacobs, A., Spek, V., Nyklicek, I., Bögels, S., & Pop, V. (2019). A randomized control trial evaluating an online mindful parenting training for mothers with elevated parental stress. Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.01550.
Provenzi, L., Grumi, S., Altieri, L., Bensi, G., Bertazzoli, E., Biasucci, G., Cavallini, A., Decembrino, L., Falcone, R., Freddi, A., Gardella, B., Giacchero, R., Giorda, R., Grossi, E., Guerini, P., Magnani, M. L., Martelli, P., Motta, M., Nacinovich, R., Pantaleo, D., Pisoni, C., Prefumo, F., Riva, L., Scelsa, B., Spartà, M. V., Spinillo, A., Vergani, P., Orcesi, S., & Borgatti, R. (2021). Prenatal maternal stress during the COVID-19 pandemic and infant regulatory capacity at 3 months: A longitudinal study. Development and Psychopathology, 1-9. https://doi.org/10.1017/S0954579421000766.
Psychogiou, L., Legge, K., Parry, E., Mann, J., Nath, S., Ford, T., & Kuyken, W. (2016). Self-compassion and parenting in mothers and fathers with depression. Mindfulness, 7(4), 896–908. https://doi.org/10.1007/s12671-016-0528-6
Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the Self-Compassion Scale. Clinical Psychology & Psychotherapy, 18(3), 250–255. https://doi.org/10.1002/cpp.702
Singh, S., & Sharma, A. (2020). Positive parenting amidst COVID-19. Mrida: An International Journal of Humanities and Social Sciences, 1(1). Retrieved from https://mrida.highereduhry.ac.in/assets/pdf/Mrida10.pdf
Suárez-Rico, B. V., Estrada-Gutierrez, G., Sánchez-Martínez, M., Perichart-Perera, O., Rodríguez-Hernández, C., González-Leyva, C., Osorio-Valencia, E., Cardona-Pérez, A., Helguera-Repetto, A. C., Espino y Sosa, S., Solis-Paredes, M., & Reyes-Muñoz, E. (2021). Prevalence of depression, anxiety, and perceived stress in postpartum mexican women during the COVID-19 lockdown. International Journal of Environmental Research and Public Health, 18(9), 4627. https://doi.org/10.3390/ijerph18094627
Tanhan, A. (2020). Utilizing Online Photovoice (OPV) methodology to address biopsychosocial spiritual economic issues and wellbeing during COVID-19: Adapting OPV to Turkish. Turkish Studies, 15(4), 1029–1086. https://doi.org/10.7827/TurkishStudies.44451
Tanhan, A., Arslan, G., Yavuz, K. F., Young, J. S., Çiçek, İ., Akkurt, M. N., Ulus, İ. Ç., Görünmek, E. T., Demir, R., Kürker, F., Çelik, C., Akça, M. Ş., Ünverdi, B., Ertürk, H., & Allen, K. (2021). A constructive understanding of mental health facilitators and barriers through Online Photovoice (OPV) during COVID-19. ESAM Ekonomik ve Sosyal Araştırmalar Dergisi, 2(2), 214–249. https://dergipark.org.tr/en/pub/esamdergisi/issue/64932/956618
Tanhan, A., & Strack, R. W. (2020). Online photovoice to explore and advocate for Muslim biopsychosocial spiritual wellbeing and issues: Ecological systems theory and ally development. Current Psychology, 39(6), 2010–2025. https://doi.org/10.1007/s12144-020-00692-6
Tanaka, M., Wekerle, C., Schmuck, M., & Paglia-Boak, A. (2011). The linkages among childhood maltreatment, adolescent mental health, and self-compassion in child welfare adolescents. Child Abuse & Neglect, 35(10), 887–898. https://doi.org/10.1016/j.chiabu.2011.07.003
Tietz, A., Zietlow, A. L., & Reck, C. (2014). Maternal bonding in mothers with postpartum anxiety disorder: The crucial role of subclinical depressive symptoms and maternal avoidance behaviour. Archives of Women Mental Health, 17(5), 433–442. https://doi.org/10.1007/s00737-014-0423-x
Funding
This study was funded by the Portuguese Foundation for Science and Technology (SFRH/BD/132588/2017).
Author information
Authors and Affiliations
Contributions
DVF: designed and executed the study, conducted the data analyses, and wrote the paper. MCC: collaborated in editing the final manuscript. HM: collaborated with the design and writing of the study and assisted with the data analyses. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Ethics Committee (blind for review) approved the study on October 4th, 2018.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fernandes, D.V., Canavarro, M.C. & Moreira, H. Self-compassion and mindful parenting among postpartum mothers during the COVID-19 pandemic: The role of depressive and anxious symptoms. Curr Psychol 42, 17560–17572 (2023). https://doi.org/10.1007/s12144-022-02959-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-02959-6