Abstract
Adverse childhood experiences (ACEs) have been associated with a variety of negative physical and psychological health outcomes. The mechanisms by which this occurs and potential protective factors present in this relationship are understudied. Mindfulness is a cognitive resource that may protect individuals against symptoms of psychological distress. It has five core facets and encourages a nonjudgmental acceptance of the present moment. The purpose of this study was to explore the role of mindfulness in the relationship between ACEs and depression, both as a mediator and as a moderator, or protective factor. We hypothesized that the aware, describe, and non-judgement facets of mindfulness would be key factors in both sets of analyses. Participants at a university (N = 279) were given the Five Factor Mindfulness Questionnaire (FFMQ), the Adverse Childhood Experiences Scale (ACES), and the Patient Health Questionnaire (PHQ-8) to measure depression. Results indicated that the describe CI [.02, .11], aware CI [.05, .17], and non-judgement CI [.06, .18] facets of mindfulness significantly mediated the relationship between ACEs and depression. Additionally, the aware facet of mindfulness was also a significant moderator in this relationship, [t (interaction) = −3.22, p < 0.01], such that individuals with a high level of awareness had no increase in depression even as the number of ACEs increased. Negative cognitions associated with ACEs may harm one’s ability to effectively describe their feelings and to be fully aware of the present moment, which may contribute to symptoms of depression. Implications for mindfulness-based interventions (MBIs) are discussed.
Similar content being viewed by others
Adverse childhood experiences (ACEs) are defined as traumatic life experiences that occur within the first eighteen years of life. Ten individual experiences are commonly recognized and can be categorized into three distinct groups: childhood abuse (emotional, physical, and sexual), childhood neglect (emotional and physical), and household dysfunction (exposure to domestic violence, substance abuse, mental illness, parental separation, and incarceration of a household member; Chapman et al., 2004; Dong et al., 2004; Felitti et al., 1998). Up to two-thirds of adults (67%) report having experienced at least one ACE (Dong et al., 2004). Additionally, these ten experiences are significantly associated with one another in that experiencing one ACE increases the likelihood that additional ACEs will co-occur (Dong et al., 2004; Felitti et al., 1998). ACEs can and frequently do lead to negative life outcomes. This may be partially attributed to the fact that these experiences can potentially increase one’s propensity towards developing a negative or depressogenic cognitive style (Liu, 2017; Sheffler et al., 2020). This paper will explore decreased mindfulness as a mechanism by which ACEs contribute to the development of depressive symptomatology, as well as identify mindfulness as a potential protective factor in this relationship. This may open avenues for targeted interventions aimed at individuals with a history of ACEs.
The impact of ACEs often extends far beyond childhood. ACEs may contribute to a wide variety of subsequent adverse psychological and physical health outcomes long after the trauma has ended. For example, ACEs have been associated with numerous chronic emotional, mental, and behavioral conditions that can, in turn, contribute to poor social and academic outcomes (Bethell et al., 2016). ACEs have been found to be positively correlated with a wide range of mood and anxiety disorders and symptoms of psychological distress including depression, anxiety, and PTSD (Anda et al., 2009; Chapman et al., 2004; Kroska et al., 2018; Liu, 2017; Sachs-Ericsson et al., 2017; Sheffler et al., 2020). Additionally, negative physical outcomes and adult health conditions associated with ACEs include alcohol dependence (Brett et al., 2018; Sheffler et al., 2020), problems such as migraines, obesity, and heart disease (Sachs-Ericsson et al., 2017; Whitaker et al., 2014), and premature death (Anda et al., 2009; Felitti et al., 1998; Whitaker et al., 2014).
Research supports the idea that mood disorders, particularly depression, may serve as a mediator in the relationship between ACEs and negative physical health conditions in adulthood such as migraines and other symptoms of chronic pain (Sachs-Ericsson et al., 2017). ACEs may hinder an individual’s ability to develop healthy and productive coping mechanisms as well as the mental resources necessary to handle subsequent life stressors. It is probable that these diminished mental resources may place individuals at a greater risk for the development of mood disorders, further decreasing one’s ability to deal with stress effectively. Without intervention, these increasingly diminished mental resources can lead to the development of physical health problems and further negative outcomes, particularly as the number of ACEs increase (Anda et al., 2009; Felitti et al., 1998; Sachs-Ericsson et al., 2017; Whitaker et al., 2014).
Given these findings, it is essential to explore the mechanisms by which ACEs lead individuals to symptoms of depression, as well as potential protective factors that may buffer this relationship. It is believed that ACEs worsen adult mental health in part through changes in the structure and function of the body’s stress-response systems (Sachs-Ericsson et al., 2017; Whitaker et al., 2014). Additionally, the presence of ACEs has been correlated with deficits in emotion regulation capacities in adult populations (Brett et al., 2018; Cameron et al., 2018; Cloitre et al., 2019). This deficit may harm one’s ability to regulate feelings of anger, depression, and anxiety (Cameron et al., 2018; Cloitre et al., 2019); as well as decrease one’s propensity towards effective self-monitoring, behavioral regulation, and self-control (Brett et al., 2018). Additionally, ineffective behavioral regulation has been associated with an increase in the use of problematic coping strategies, further increasing the likelihood that those with a history of ACEs may subsequently suffer from depression and other negative life outcomes (Sheffler et al., 2020; Whitaker et al., 2014).
Individuals with a history of ACEs may have an increased propensity towards developing a negative or depressogenic cognitive style that may make it difficult to contend with subsequent life stressors (Liu, 2017; Sheffler et al., 2020). Research has suggested that these individuals are more likely to hold a negative perception of their environment as posing greater and more numerous threats than is accurate, as well as be more likely to internalize negative emotions. Additionally, the stress inflicted by ACEs may lead to damaged stress regulation mechanisms in the brain (McLaughlin et al., 2010). These factors together further increase one’s risk of psychopathology later in life (Kelifa et al., 2020; Sheffler et al., 2020). For example, one study found that current stressful events (CSEs) perpetuate negative mental health outcomes in college students with a history of ACEs and contribute to the occurrence and recurrence of depression. Additionally, individuals with a history of ACEs may display greater sensitivity to CSEs, as well as be less apt to deal with these stressors in a healthy and productive way so as to avoid further symptoms of depression (Kelifa et al., 2020).
Mindfulness is a cognitive resource that provides individuals with the tools necessary to deal with stress in a productive and healthy manner (Keng et al., 2011). Thus, decreased mindfulness may be a mechanism by which ACEs contribute to symptoms of depression. Furthermore, an increased level of mindfulness may serve as a protective factor against depression for individuals with a history of ACEs. At its core, mindfulness is a contemplative and restorative practice associated with psychological well-being that originates from Buddhist traditions (Keng et al., 2011). Mindfulness focuses heavily on present moment awareness of internal and external thoughts and stimuli, as well as a nonjudgmental acceptance of one’s moment-to-moment experiences (Keng et al., 2011). Buddhist mindfulness practices have been translated and modified in recent years for use in Western clinical practices. This adoption of mindfulness into Western cultures stems in part from the efforts of clinical psychologists to test and validate new treatments that might decrease suffering from, and symptoms related to, psychological disorders (Baer, 2011).
The benefits of mindfulness practices and interventions are numerous. Mindfulness has been shown to protect against symptoms of psychological distress such as depression, anxiety, and rumination (Kircaburun et al., 2019). Additionally, it has been associated with higher levels of life satisfaction, positive personality characteristics, enhanced cognitive performance and attention, and psychological well-being (Baer et al., 2012; Keng et al., 2011; Maloney et al., 2016). In addition to its positive effects on mental health, mindfulness practices have also been shown to alleviate symptoms of physical pain and lead to healthy changes in the structure and function of certain areas of the brain (Whitaker et al., 2014).
Research suggests that experiences of trauma, such as sexual assault, may contribute to an individual’s decreased level of mindfulness, which may in turn contribute to negative psychological outcomes (Kroska et al., 2018). Furthermore, other research has posited mindfulness as a mediator in the relationship between ACEs and problematic alcohol use (Brett et al., 2018). The role that mindfulness plays in the relationship between ACEs and depression has not yet been directly studied. However, a recent study has identified psychological inflexibility as a mechanism that may mediate the relationship between ACEs and depression (Makriyianis et al., 2019). People who are psychologically inflexible tend to avoid negative thoughts and emotions as well as have a difficult time disentangling their sense of self from their negative thoughts (Hayes et al., 2006; Kashdan & Rottenberg, 2010; Makriyianis et al., 2019). While psychological inflexibility is a multifaceted construct, a lack of awareness of the present moment is one of its core components (Hayes et al., 2006; Makriyianis et al., 2019). Similarly, awareness of the present moment is a core component of mindfulness.
In addition to potentially mediating the relationship between ACEs and depression, it is reasonable to postulate that mindfulness may also serve as a protective factor in this relationship, decreasing the likelihood that someone with a history of ACEs would develop symptoms of depression. Mindfulness-based interventions have been shown to decrease maladaptive emotional responses, increase emotion regulation, behavioral regulation and self-control, as well as increase one’s ability to tolerate future stressful situations. Difficulties with emotion regulation have been correlated with symptoms of psychopathology and low psychological resilience (Brett et al., 2018; Cameron et al., 2018; Cloitre et al., 2019). However, one study found that mindfulness moderated the relationship between childhood sexual abuse and anxiety and anger such that individuals who have experienced this type of abuse and who also have a high level of mindfulness actually had higher levels of anxiety and anger than did individuals who have not experienced this type of abuse (Daigneault et al., 2016). While counterintuitive, this finding may be explained in part by the possibility that individuals who have a low level of mindfulness might be better able to repress thoughts about past traumas and experiences. To our knowledge, other similar research has not provided further support for this finding. Therefore, in the present study we hypothesize that mindfulness may act as a moderator such that those with a history of ACEs but who also have high levels of trait mindfulness will be less likely to experience depression than those with similar levels of ACEs but lower levels of trait mindfulness.
It is also important to note that in Western practice, mindfulness is conceptualized as a multifaceted construct. Specifically, it is commonly broken down into five facets as seen in the Five Factor Mindfulness Questionnaire (FFMQ). These five facets include observing bodily states (observe), describing one’s experiences (describe), acting with awareness (aware), approaching the world without immediate reaction (nonreactivity), and being nonjudgmental about one’s thoughts or experiences (non-judgement; Baer et al., 2006). While the implementation of mindfulness-based practices can add value to a variety of clinical treatments, not all five individual facets may be equally useful. Research has shown that the non-judgement and acting with awareness facets of mindfulness may be of unique importance in reducing symptoms of psychopathology. Specifically, non-judgement has been found to be inversely correlated with symptoms of depression, anxiety, and stress; while acting with awareness has been found to be of particular importance in predicting symptoms of depression (Baer et al., 2006; Cash & Whittingham, 2010). Similarly, non-judgement and acting with awareness were found to be the best protective factors in the relationship between ACEs and heavy alcohol use and related consequences (Brett et al., 2018). Additional research supports the idea that acting with awareness, non-judgement, and describing one’s experiences may be negatively correlated with a variety of symptoms of psychopathology, including but not limited to depression (Mandal et al., 2012). It is important to identify which of the five facets of mindfulness may be of particular importance in better understanding the relationship between ACEs and depression, both as a mediator and as a moderator.
Given the heavy focus on acting with awareness, describing one’s experiences, and non-judgement in previous research that is relevant to the relationship between ACEs and depression, we hypothesize that acting with awareness, describing one’s experiences, and non-judgement will be key factors in both mediation and moderation analyses. Specifically we hypothesize that these factors will mediate the relationship between ACES and symptoms of depression. We also hypothesize that these factors will serve as moderators such that individuals who have high ACES scores but are also high in acting with awareness, describing one’s experiences, and non-judgment will have lower depression scores than those with high ACES scores and low scores on these variables. While we will test all five facets of mindfulness in both sets of analyses, significant findings regarding the observe and nonreactivity facets of mindfulness in previous research are limited. Therefore, our hypotheses surrounding these two facets are more exploratory in nature.
Method
Participants
The final sample in the present study included a total of 279 students at a public liberal arts university in the southeast United States. The age range of our participants was 17 to 48 (M = 19.22, SD = 2.94). See Table 1 for the demographics of our participants. Overall, our participants largely identified as White heterosexual females that were middle to upper middle class.
Participants were also asked whether or not they regularly engage in any mindfulness practices. The majority, 71.0% (n = 198) reported that they do not regularly engage in any mindfulness practices, however, 29.0% (n = 81) reported that they do regularly engage in mindfulness practices. Participants who reported that they do regularly engage in mindfulness practices were also asked what types of mindfulness practices they engage in. A total of 12.5% (n = 35) reported that they journal, 12.2% (n = 34) reported that they meditate, 11.8% (n = 33) reported that they pray, 10.0% (n = 28) reported that they do yoga, 0.7% (n = 2) reported that they do tai chi, and 5.4% (n = 15) reported that they engage in another type of mindfulness practice that was not listed.
Procedures and Measures
Following the study’s review and approval by the University Institutional Review Board, participants were recruited through the University’s participant pool of general psychology students. For their participation in our study, participants were given a partial credit towards their experiment participation requirement. While most participants were at least 18 years old, participants who were 17 years old were allowed to participate in our study if they had a parental consent form on file with the Department of Psychological Science. The description of the study informed potential participants that the study was about understanding how peoples’ thoughts and behaviors are affected by past life experiences. Participants were able to voluntarily sign up for this study based on the description provided. This study was designed to test the relationship between ACEs, mindfulness, and depression; however, there were other variables included in the data collection that were not included in this study’s data analysis (e.g., variables about COVID-19 and social media use).
After participants signed up for our study, they received a secure link to our online survey that they were able to use at any time during the study’s availability window. Once participants clicked on the link taking them to the online survey, they were asked to fill out the informed consent. After they completed the informed consent and agreed to the terms of the survey, they were able to continue with the rest of the survey. Following their completion of the survey, participants were able to review the debriefing page that explained in greater detail the purpose of our study. Participants were also provided with information about available resources they could utilize if they felt the need for further information and/or support. After reviewing the debriefing page, participants were directed back to the University’s general psychology participant pool website and received partial credit towards their experiment participation requirement. The following measures were completed in the order listed below.
Five Factor Mindfulness Questionnaire (FFMQ)
The Five Factor Mindfulness Questionnaire (FFMQ; Baer et al., 2006) is a 39-item questionnaire measuring the five facets of mindfulness, with responses scored on a scale from 1 (never/rarely true of me) to 5 (very often/ always true of me). The five facets include nonreactivity (e.g., “I perceive my feelings and emotions without having to react to them”), observe (e.g., “I pay attention to sensations, such as the wind in my hair or sun on my face”), aware (e.g., “I find myself doing things without paying attention”), describe (e.g., “I can easily put my beliefs, opinions, and expectations into words”), and non-judgement (e.g., “I criticize myself for having irrational or inappropriate emotions”). Scores were averaged in each subscale and each scale was scored such that higher scores indicated greater levels of mindfulness. In the original investigation, each subscale had good internal reliability: nonreact (α = .75), observe (α = .83), aware (α = .87), describe (α = .91), and nonjudge (α = .87). Reliability for each subscale in the current sample was also good: nonreact (α = .77), observe (α = .70), aware (α = .87), describe (α = .89), and nonjudge (α = .91).
Adverse Childhood Experiences (ACEs)
The Adverse Childhood Experiences Scale (ACEs; Dong et al., 2004) is a 10-item measure assessing negative childhood experiences occurring in the first 18 years of life. The items in the measure focus on categories of experiences such as abuse, neglect, and household dysfunction (e.g., “Did a parent or other adult in the household often... swear at you, insult you, put you down, or humiliate you? Or act in a way that made you afraid that you might be physically hurt?”). Response options for all items were yes (coded as 1) or no (coded as 0). The total score was summed and could potentially range from 0 to 10.
Patient Health Questionnaire (PHQ-8)
The Patient Health Questionnaire (PHQ-8; Kroenke et al., 2009) is an 8-item measure assessing depressive symptomatology. The measure (e.g., “How often have you been bothered by...little interest or pleasure in doing things?”) examines the presence of symptoms of depression over the past two weeks. Responses are scored on a scale from 0 (not at all) to 3 (nearly every day), and scores are summed together with higher scores indicating a greater presence of depression symptoms. Previous research (Hwang et al., 2011) has proven the scale to have high internal reliability (α = .87). This scale also has good reliability in the present study (α = .90).
Analysis Plan
First, the data was examined to ensure that it was within the acceptable range for both skewness and kurtosis (−2 to +2; George & Mallery, 2010). Next, total scores were calculated for each variable and participant as appropriate (e.g., ACEs were summed to create a total score). Bivariate correlations were run between variables in order to determine whether there was a relationship between our IV (ACEs), our mediators (the five facets of mindfulness), and our DV (depression). Mediation analyses were then run using Process Model 4 (Hayes, 2018) with ACES as the predictor variable, each mindfulness factor as the mediators, and depression as the outcome variable. In each analysis, if the 95% confidence interval of the lower and upper levels of the completely standardized indirect effect did not cross zero, then that facet of mindfulness was considered to be a significant mediator. Finally, moderation analyses were run using Process Model 1 (Hayes, 2018) to determine if any of the five facets of mindfulness significantly moderated the relationship between ACEs and depression. Each of the five facets of mindfulness was considered to be a moderator if the interaction term in the analysis was significant. For analyses with significant moderation, the effects of ACES on depression were explored at one standard deviation above and below the mean using regression.
Results
On average, our sample reported a similar number of exposures to adverse childhood experiences compared to reports in previous research. Our sample reported a slightly higher rate of exposure when compared to the original CDC study (Felitti et al., 1998). See Table 2 for the prevalence of exposure to each of the ten ACEs. Just over a quarter of our participants (29.0%) reported exposure to zero ACEs, 24.4% reported exposure to one, 17.9% reported exposure to two, 10.8% reported exposure to three, 7.2% reported exposure to four, and 10.8% reported exposure to five or more. Overall, 71.1% of participants reported exposure to at least one ACE.
The means, standard deviations, ranges, and correlations among all measures are reported in Table 3. In terms of reported levels of depression, 30.5% of participants reported no significant depressive symptoms, 29.5% reported mild depressive symptoms, 19% reported moderate depressive symptoms, 11.5% reported moderately severe depressive symptoms, and 9.7% reported severe depressive symptoms. Participants reported low to average levels of mindfulness across the five facets.
ACEs were positively correlated with depression, and negatively correlated with the describe, aware, and non-judgement facets of mindfulness (see Table 3). ACEs were not significantly correlated with the observe or nonreactivity facets of mindfulness. Depression was negatively correlated with the describe, aware, nonreactivity, and non-judgement facets of mindfulness. The five facets of mindfulness were generally significantly positively correlated with one another.
Process Model 4 (Hayes, 2018) was used to determine whether or not each of the five facets of mindfulness significantly mediated the relationship between ACEs and depression. Mediation analyses were run on the full 279 participants. Analyses revealed that the describe, aware, and non-judgement facets of mindfulness were significant mediators in this relationship (see Fig. 1 for the path coefficients for each analysis). Describe had a completely standardized indirect effect of .07 (SE = .02, CI [.02, .11]). This model explained 21.9% of the variance in depression scores, F(2, 276) = 37.37, p < .001. Aware had a completely standardized indirect effect of .11 (SE = .03, CI [.05, .17]). This model explained 39.6% of the variance in depression scores, F(2, 276) = 105.60, p < .001. Non-judgement had a completely standardized indirect effect of .12 (SE = .03, CI [.06, .18]). This model explained 36.6% of the variance in depression scores, F(2, 276) = 80.94, p < .001. See Table 4 for the confidence intervals for the remaining non-significant variables.
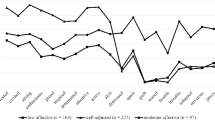
Process Model 1 (Hayes, 2018) was used to determine whether or not each of the five facets of mindfulness significantly moderated the relationship between ACEs and depression. Moderation analyses were run on the full 279 participants. Table 5 displays the coefficients for each variable and their interaction terms. ACEs had a significant main effect in each analysis. There was also a significant main effect of the mindfulness variable for every facet of mindfulness except observe. Additionally, there was a significant interaction for aware, indicating that the aware facet of mindfulness significantly moderated the relationship between ACEs and depression. Table 5 lists the main effects and interactions for all variables. Figure 2 demonstrates the effects of ACES on depression at low, medium, and high levels of awareness. Cutoff scores for low and high levels of awareness were one standard deviation below and above the mean score, respectively as these are standard values used in Process. At low (cutoff score of 1.88) and average (cutoff score of 2.75) levels of awareness, ACEs significantly predicted depression. Interestingly, at high levels of awareness (beginning at a score of 3.20), ACEs no longer significantly predicted depressive symptomatology. As can be seen in Fig. 2, for those with awareness scores at one standard deviation above the mean, increased ACEs were unrelated to an increase in depression scores.
The association between ACEs and depression as moderated by the aware facet of mindfulness. ACEs = Adverse Childhood Experiences; PHQ = depression; Low, Medium, and High = the 16th, 50th, and 84th percentile of aware scores, respectively; Low, Medium, and High aware score cutoffs = 1.88, 2.75, and 3.63, respectively
Discussion
The purpose of this study was to explore decreased mindfulness as a mechanism by which individuals with a history of ACEs may develop depressive symptomatology, as well as identify mindfulness as a potential protective factor in this relationship. While we tested all five facets of mindfulness, we hypothesized that describing one’s experiences, acting with awareness, and non-judgement would be key factors in both mediation and moderation analyses. Our hypotheses were partially supported. We found that the describe, aware, and non-judgement facets of mindfulness significantly mediated the relationship between ACEs and depression. Additionally, we found that the aware facet of mindfulness also significantly moderated this relationship such that a high level of awareness may serve as a protective factor against depression even as the number of ACEs increase. The observe and nonreactivity facets of mindfulness were not found to be significant in either set of analyses.
Our findings regarding the describe, aware, and non-judgement facets of mindfulness as mediators in the relationship between ACEs and depression are consistent with previous research. Specifically, one study found that mindfulness may mediate the relationship between ACEs and problematic alcohol use (Brett et al., 2018). Another study found that psychological inflexibility, a multifaceted construct defined in part by a lack of awareness of the present moment, significantly mediated the relationship between ACEs and depression (Makriyianis et al., 2019). This supports the idea that the awareness facet of mindfulness may be an important factor in the relationship between ACEs and mental health. Other research looking at trauma more broadly has indicated that decreased mindfulness may be an important factor by which traumatic experiences such as sexual assault contribute to negative psychological outcomes such as PTSD, anxiety, and anger (Daigneault et al., 2016; Kroska et al., 2018).
In our study, we found that the three facets of mindfulness most influential in the relationship between ACEs and depression are describe, aware, and non-judgement. Previous research on mindfulness as a mediator in the relationship between ACEs and problematic alcohol use also identified the aware and non-judgement facets as significant mediators in this relationship (Brett et al., 2018). It is plausible that the negative emotions associated with a high number of ACEs may harm one’s ability to be fully aware of the present moment and their surrounding environment, and that this lack of awareness or sense of being outside of the present moment or perhaps being stuck in the past may contribute to symptoms of depression. ACEs may also increase the tendency to have a negative or judgmental attitude toward one’s own thoughts and experiences, which may also contribute to symptoms of depression.
Limited research exists that explores the describe facet of mindfulness in this context. We postulate that describe may be a significant mediator in the relationship between ACEs and depression due to the fact that a high number of ACEs may harm a child’s ability to describe their emotions effectively, with difficulties in this area persisting throughout the lifespan. Research has shown that alexithymia, a disorder characterized in part by an inability to recognize and describe one’s emotions effectively, is highly correlated with depression (Honkalampi et al., 2000). Furthermore, research has demonstrated that ACEs are closely associated with the alexithymia construct “difficulty in describing feelings to others” in a population of individuals with major depressive disorder (Honkalampi et al., 2019). This may be partially explained by the fact that ACEs may harm one’s abilities to develop effective emotion regulation capacities (Brett et al., 2018; Honkalampi et al., 2019). Therefore, it is logical that the describe facet of mindfulness may be an important mediator in the relationship between ACEs and depression.
Our findings regarding the aware facet of mindfulness as a moderator in the relationship between ACEs and depression are also consistent with the majority of previous research that has supported the idea that mindfulness may serve as a protective factor against a variety of symptoms of psychological distress (Kircaburun et al., 2019). However, our findings contradict the counterintuitive findings of a single study that found mindfulness to be a moderator in the relationship between childhood sexual abuse and anxiety and anger such that individuals with a history of sexual abuse who also had high levels of mindfulness experienced increased anxiety and anger (Daigneault et al., 2016). It is important to note, however, that this aforementioned study looked at the relationship between sexual abuse and anxiety and anger, and our study looked at the relationship between ACEs more broadly and depression. To our knowledge, the present study is the first to identify mindfulness as a moderator in the relationship between ACEs and mental health outcomes, specifically depression. Our findings were consistent with our expectation that it would play a protective role. Individuals with a high level of awareness had a nonsignificant increase in depression scores even as the number of ACEs increased. A mindful awareness of the present moment seems to be an important protective factor for individuals with a history of ACEs.
Limitations and Future Research
Limitations to our study include a largely homogenous pool of participants. Our sample consisted of primarily white and female undergraduate students at a single university. Due to this homogeneity, we did not use our demographic variables as controls or conduct separate analyses to determine whether our results would hold for different demographic groups. Future research may wish to consider determining whether these effects would hold in demographically different groups. While our sample reported a statistically similar number of ACEs as compared to previous research, an overwhelming majority (approximately 75.0%) reported their socioeconomic status to be middle or upper middle class. We know that families of a higher socioeconomic status tend to have greater financial resources to afford services like therapy following adverse experiences such as childhood trauma. Additionally, individuals of a lower socioeconomic status and/or racial/ethnic minority backgrounds tend to face more numerous chronic stressors, adversities, and experiences of discrimination (Myers et al., 2015). This multitude of factors can quickly compound for at risk populations and may be important in understanding the relationship between ACEs and depression. Future research could examine the role mindfulness plays in the relationship between ACEs and depression with either a broader community population not specific to a university or perhaps even a community known to have limited resources or a large population of low-SES families. It is likely that high levels of trait mindfulness would have an even greater impact in breaking the link between ACEs and depression for populations with fewer financial and community resources.
Furthermore, while we modeled depression as a result of decreased mindfulness, this relationship is likely bidirectional. It is plausible that higher levels of depression may result in decreased mindfulness. Nevertheless, our findings are important because trait mindfulness is something that can be changed over time through intervention. For this reason, it may be more useful to look at depression as a result of decreased mindfulness because one’s level of mindfulness can be increased through intervention before depression symptoms are ever experienced. Knowing that individuals with a history of ACEs might benefit from early mindfulness interventions is an important practical application of these findings. Longitudinal studies would be needed to determine whether decreased mindfulness is a temporal precursor to increased depression.
Other limitations include the fact that all of our variables were retrospective self-report. Self-report measures are subject to a variety of biases that may alter the reported results, most of which are difficult to measure or control for. Future research may wish to use daily dairies or other methods in order to determine how mindfulness affects levels of depression in real time. Finally, we selected the PHQ-8 which excludes the item about suicidality. Future research may wish to use the PHQ-9 which includes this item or an additional measure of suicidal ideation in order to determine if these effects are also relevant for suicidal ideation.
Despite these limitations, these findings have important implications both for preventative treatments for individuals with a history of ACEs who are at an increased risk for the development of depressive symptomatology, as well as for individuals with a history of ACEs who are already suffering from symptoms of depression. Mindfulness-based interventions (MBIs) have been developed in an effort to harness the positive effects of mindfulness in a way that can be implemented with clinical populations to provide treatment for mental health disorders (Keng et al., 2011), as well as with adults and children in a variety of different contexts (Maloney et al., 2016). These interventions assist individuals in developing a mindful awareness, which encourages an acceptance of one’s own experiences and an understanding of those of others leading to greater compassion and patience. Examples of current MBIs used in clinical practice include Mindfulness Based Cognitive-Therapy (MBCT), Dialectical Behavior Therapy (DBT), and even Mindfulness-Based Stress Reduction (MBSR) which aims to reduce the impact of chronic physical pain (Keng et al., 2011). Recent research has found that MBIs may improve treatment outcomes of patients with depression even more so than current clinical best practices (Goldberg et al., 2021). Our findings suggest that a MBI focused specifically on cultivating an individual’s ability to describe their experiences and feelings, an ability to maintain a mindful awareness of the present moment, and an ability to experience feelings and thoughts without immediately judging them to be bad or inappropriate may be a beneficial course of intervention for individuals with a history of ACEs, with or without current depressive symptomatology.
Finally, given the fact that ACEs occur before the age of eighteen, our findings have critical implications for early intervention programs aimed at children with a history of trauma or who are at a high risk for childhood trauma. Mindfulness based programs and practices have been found to have a positive effect on young children and students in a variety of ways. For example, these practices have been shown to increase executive functioning in second grade students (Flook et al., 2010) as well as empathy and self-regulation among economically disadvantaged preschoolers (Poehlmann-Tynan et al., 2016). Mindfulness may work to enhance attention and academic skills by helping students slow down and learn to self-regulate when they are feeling overwhelmed and stressed (Moreno, 2017).
MBIs aimed at developing a mindful awareness of the present moment implemented with children in schools with a large high-risk population may make a significant contribution to the prevention of negative long-term outcomes such as depression. A high level of awareness may encourage children to stay focused on the present moment and what is happening in the classroom instead of thinking about traumatic events that have happened in the past. Children currently dealing with ACEs might use mindful awareness to separate themselves from difficulties at home and focus to a greater degree on their academics and opportunities to be safe and socialize at school. Additionally, awareness may interrupt the cycle of ruminative thoughts children may have about past traumatic experiences. We know from previous research that a tendency to ruminate on the past frequently leads individuals to depression and other negative outcomes (Nolen-Hoeksema, 1998). Children may also use an awareness of the present moment as a tool to develop effective emotion regulation skills and make better decisions when difficult situations arise (Brett et al., 2018; Moreno, 2017). Future research should continue to explore the five facets of mindfulness as both mediators and moderators in the relationship between ACEs and depression.
Data Availability
All data generated and analyzed during this study is available from the corresponding author upon request.
References
Anda, R. F., Dong, M., Brown, D. W., Felitti, V. J., Giles, W. H., Perry, G. S., Valerie, E. J., & Dube, S. R. (2009). The relationship of adverse childhood experiences to a history of premature death of family members. BMC Public Health, 9(1), 106–115. https://doi.org/10.1186/1471-2458-9-106.
Baer, R. A. (2011). Measuring mindfulness. Contemporary Buddhism, 12(1), 241–261. https://doi.org/10.1080/14639947.2011.564842.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504.
Baer, R. A., Lykins, E. L., & Peters, J. R. (2012). Mindfulness and self-compassion as predictors of psychological wellbeing in long-term meditators and matched nonmeditators. The Journal of Positive Psychology, 7(3), 230–238. https://doi.org/10.1080/17439760.2012.674548.
Bethell, C., Gombojav, N., Solloway, M., & Wissow, L. (2016). Adverse childhood experiences, resilience and mindfulness-based approaches: Common denominator issues for children with emotional, mental, or behavioral problems. Child and Adolescent Psychiatric Clinics of North America, 25(2), 139–156. https://doi.org/10.1016/j.chc.2015.12.001.
Brett, E. I., Espeleta, H. C., Lopez, S. V., Leavens, E. L., & Leffingwell, T. R. (2018). Mindfulness as a mediator of the association between adverse childhood experiences and alcohol use and consequences. Addictive Behaviors, 84, 92–98. https://doi.org/10.1016/j.addbeh.2018.04.002.
Cameron, L., Carroll, P., & Hamilton, K. (2018). Evaluation of an intervention promoting emotion regulation skills for adults with persisting distress due to adverse childhood experiences. Child Abuse and Neglect, 79, 423–433. https://doi.org/10.1016/j.chiabu.2018.03.002.
Cash, M., & Whittingham, K. (2010). What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness, 1(3), 177–182. https://doi.org/10.1007/s12671-010-0023-4.
Chapman, D. P., Whitfield, C. L., Felitti, V. J., Dube, S. R., Edwards, V. J., & Anda, R. F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82, 217–225. https://doi.org/10.1016/j.jad.2003.12.013.
Cloitre, M., Khan, C., Mackintosh, M., Garvert, D. W., Henn-Haase, C. M., Falvey, E. C., & Saito, J. (2019). Emotion regulation mediates the relationship between ACES and physical and mental health. Psychological Trauma: Theory, Research, Practice, and Policy, 11(1), 82–89. https://doi.org/10.1037/tra0000374.
Daigneault, I., Dion, J., Hébert, M., & Bourgeois, C. (2016). Mindfulness as mediator and moderator of post-traumatic symptomatology in adolescence following childhood sexual abuse or assault. Mindfulness, 7, 1306–1315. https://doi.org/10.1007/s12671-016-0571-3.
Dong, M., Anda, R. F., Felitti, V. J., Dube, S. R., Williamson, D. F., Thompson, T. J., Loo, C. M., & Giles, W. H. (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28(7), 771–784. https://doi.org/10.1016/j.chiabu.2004.01.008.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventative Medicine, 14(4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8.
Flook, L., Smalley, S. L., Kitil, M. J., Galla, B. M., Kaiser-Greenland, S., Locke, J., Ishijima, E., & Kasari, C. (2010). Effects of mindful awareness practices on executive functions in elementary school children. Journal of Applied School Psychology, 26, 70–95. https://doi.org/10.1080/15377900903379125.
George, D. & Mallery, M. (2010). SPSS for windows step by step: A simple guide and reference, 17.0 update (10a ed.) Pearson.
Goldberg, S. B., Riordan, K. M., Sun, S., & Davidson, R. J. (2021). The empirical status of mindfulness-based interventions: A systematic review of 44 meta-analyses of randomized controlled trials. Perspectives on Psychological Science, 1–23. Advanced Online Publication. https://doi.org/10.1177/1745691620968771.
Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). Guilford Press.
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. https://doi.org/10.1016/j.brat.2005.06.006.
Honkalampi, K., Hintikka, J., Tanskanen, A., Lehtonen, J., & Viinamäki, H. (2000). Depression is strongly associated with alexithymia in the general population. Journal of Psychosomatic Research, 48(1), 99–104. https://doi.org/10.1016/S0022-3999(99)00083-5.
Honkalampi, K., Flink, N., Lehto, S. M., Ruusunen, A., Koivumaa-Honkanen, H., Valkonen-Korhonen, M., & Viinamäki, H. (2019). Adverse childhood experiences and alexithymia in patients with major depressive disorder. Nordic Journal of Psychiatry, 74(1), 45–50. https://doi.org/10.1080/08039488.2019.1667430.
Hwang, B., Fleischmann, K. E., Howie-Esquivel, J., Stotts, N. A., & Dracup, K. (2011). Caregiving for patients with heart failure: Impact on patient's families. American Journal of Critical Care, 20, 431–442. https://doi.org/10.4037/ajcc2011472.
Kashdan, T. B., & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878. https://doi.org/10.1016/j.cpr.2010.03.001.
Kelifa, M. O., Yang, Y., Herbert, C., He, Q., & Wang, P. (2020). Psychological resilience and current stressful events as potential mediators between adverse childhood experiences and depression among college students in Eritrea. Child Abuse & Neglect, 106. Advanced Online Publication. https://doi.org/10.1016/j.chiabu.2020.104480.
Keng, S., Smoski, M., & Robins, C. (2011). Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review, 31(6), 1041–1056. https://doi.org/10.1016/j.cpr.2011.04.006.
Kircaburun, K., Griffiths, M. D., & Billieux, J. (2019). Trait emotional intelligence and problematic online behaviors among adolescents: The mediating role of mindfulness, rumination, and depression. Personality and Individual Differences, 139, 208–213. https://doi.org/10.1016/j.paid.2018.11.024.
Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B. W., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114, 163–173. https://doi.org/10.1016/jad.2008.06.026.
Kroska, E. B., Miller, M. L., Roche, A. I., Kroska, S. K., & O’Hara, M. W. (2018). Effects of traumatic experiences on obsessive-compulsive and internalizing symptoms: The role of avoidance and mindfulness. Journal of Affective Disorders, 225, 326–336. https://doi.org/10.1016/j.jad.2017.08.039.
Liu, R. T. (2017). Childhood adversities and depression in adulthood: Current findings and future directions. Clinical Psychology: Science and Practice, 24(2), 140–153. https://doi.org/10.1111/cpsp.12190.
Makriyianis, H. M., Adams, E. A., Lozano, L. L., Mooney, T. A., Morton, C., & Liss, M. (2019). Psychological inflexibility mediates the relationship between adverse childhood experiences and mental health outcomes. Journal of Contextual Behavioral Science, 14, 82–89. https://doi.org/10.1016/j.jcbs.2019.09.007.
Maloney, J. E., Lawlor, M. S., Schonert-Reichl, K. A., & Whitehead, J. (2016). A mindfulness-based social and emotional learning curriculum for school-aged children: The MindUP program. Handbook of Mindfulness in Education, 20, 313–334. https://doi.org/10.1007/978-1-4939-3506-2_20.
Mandal, S. P., Arya, Y. K., & Pandey, R. (2012). Mental health and mindfulness: Mediational role of positive and negative affect. SIS Journal of Projective Psychology and Mental Health, 19(2), 150–159.
McLaughlin, K. A., Conron, K. J., Koenen, K. C., & Gilman, S. E. (2010). Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: A test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine, 40(10), 1647–1658. https://doi.org/10.1017/S0033291709992121.
Moreno, A. J. (2017). A theoretically and ethically grounded approach to mindfulness practices in the primary grades. Childhood Education, 93(2), 100–108. https://doi.org/10.1080/00094056.2017.1300487.
Myers, H. F., Wyatt, G. E., Ullman, J. B., Loeb, T. B., Chin, D., Prause, N., Zhang, M., Williams, J. K., Slavich, G. M., & Liu, H. (2015). Cumulative burden of lifetime adversities: Trauma and mental health in low-SES African Americans and Latino/as. Psychological Trauma: Theory, Research, Practice, and Policy, 7(3), 243–251. https://doi.org/10.1037/a0039077.
Nolen-Hoeksema, S. (1998). The other end of the continuum: The costs of rumination. Psychological Inquiry, 9(3), 216–219. https://doi.org/10.1207/s15327965pli0903_5.
Poehlmann-Tynan, J., Vigna, A. B., Weymouth, L. A., Gerstein, E. D., Burnson, C., Zabransky, M., Lee, P., & Zahn-Waxler, C. (2016). A pilot study of contemplative practices with economically disadvantaged preschoolers: Children’s empathic and self-regulatory behaviors. Mindfulness, 7(1), 46–58. https://doi.org/10.1007/s12671-015-0426-3.
Sachs-Ericsson, N. J., Sheffler, J. L., Stanley, I. H., Piazza, J. R., & Preacher, K. J. (2017). When emotional pain becomes physical: Adverse childhood experiences, pain, and the role of mood and anxiety disorders. Journal of Clinical Psychology, 73(10), 1403–1428. https://doi.org/10.1002/jclp.22444.
Sheffler, J. L., Stanley, I., & Sachs-Ericsson, N. (2020). ACEs and mental health outcomes. In Adverse childhood experiences (pp. 47-69). Academic Press. https://doi.org/10.1016/B978-0-12-816065-7.00004-5.
Whitaker, R. C., Dearth-Wesley, T., Gooze, R. A., Becker, B. D., Gallagher, K. C., & McEwen, B. S. (2014). Adverse childhood experiences, dispositional mindfulness, and adult health. Preventative Medicine, 67, 147–153. https://doi.org/10.1016/j.ypmed.2014.07.029.
Code Availability
Not applicable.
Author information
Authors and Affiliations
Contributions
ML supervised the project and HM did the bulk of the writing. The remaining four authors participated in the conceptualization of the project, data collection, data analysis, and assisted with the writing.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Institutional Review Board at the University of Mary Washington and informed consent was obtained from all participants prior to conducting this research. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McKeen, H., Hook, M., Podduturi, P. et al. Mindfulness as a mediator and moderator in the relationship between adverse childhood experiences and depression. Curr Psychol 42, 6576–6586 (2023). https://doi.org/10.1007/s12144-021-02003-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-021-02003-z