Abstract
Background
Survival rates of head and neck squamous cell carcinoma (HNSCC) have only marginally improved in the last decades. Hence there is a need for predictive biomarkers for long-time survival that can help to guide treatment decisions and might lead to the development of new therapies. The phosphatidylinositol 3-kinase (PI3K)/AKT/mTOR signaling pathway is the most frequently altered pathway in HNSCC, genes are often mutated, amplificated and overexpressed causing aberrant signaling affecting cell growth and differentiation. Numerous genetic alterations of upstream and downstream factors have currently been clarified. However, their predictive value has yet to be established. Therefore we assess the predictive value of p-mTOR, p-ERK and PTEN expression.
Methods
Tissue microarrays (TMA’s) of HPV-negative patients with oropharyngeal (n = 48), hypopharyngeal (n = 16) or laryngeal (n = 13) SCC, treated with primary chemoradiation (cisplatin/carboplatin/cetuximab and radiotherapy), were histologically stained for p-mTOR, PTEN and p-ERK. Expression was correlated to overall survival (OS), disease free survival (DFS) and locoregional control (LRC). Also p-mTOR was histologically stained in a separate cohort of HNSCC organoids (n = 8) and correlated to mTOR-inhibitor everolimus response.
Results
High p-mTOR expression correlated significantly with worse OS in multivariate analysis in the whole patient cohort [Hazar Ratio (HR) 1.06, 95%CI 1.01–1.11, p = 0.03] and in the cisplatin/carboplatin group with both worse OS (HR 1.09, 95%CI 1.02–1.16, p = 0.02) and DFS (HR 1.06, 95%CI 1.00–1.12, p = 0,04). p-ERK expression correlated significantly with DFS in univariate analysis in the whole patient cohort (HR 1.03, 95%CI 1.00–1.05, p = 0.04) and cisplatin/carboplatin group (HR 1.03, 95%CI 1.00–1.07, p = 0.04). PTEN-expression did not correlate with OS/DFS/LRC. Better organoid response to everolimus correlated significantly to higher p-mTOR expression (Rs = − 0.731, p = 0.04).
Conclusions
High p-mTOR expression predicts and high p-ERK expression tends to predict worse treatment outcome in HPV negative HNSCC patients treated with chemoradiation, providing additional evidence that these markers are candidate prognostic biomarkers for survival in this patient population. Also this study shows that the use of HNSCC organoids for biomarker research has potential. The role of PTEN expression as prognostic biomarker remains unclear, as consistent evidence on its prognostic and predictive value is lacking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer is the 7th most common type of cancer worldwide with approximately 1.000.000 new cases in 2020 [1]. Over 95% of these cancers are squamous cell carcinoma (SCC) [2,3,4]. In current practice, therapy for head and neck squamous cell carcinoma (HNSCC) generally depends on the anatomical location. For oral SCC, the standard treatment is primary surgery, whereas pharyngeal and laryngeal SCC often undergo primary (chemo)radiation. At the time of diagnosis, HNSCC has frequently spread to regional lymph nodes. Despite advances in surgical techniques and adjuvant therapies, survival rates have only marginally improved over the last two decades [5]. Therefore, there is a need for biomarkers predicting long-time survival that can help to guide treatment decisions and might lead to the development of new therapies [6, 7].
The phosphatidylinositol 3-kinase (PI3K)/AKT/mTOR signaling pathway is the most frequently altered pathway in HNSCC [8]. Normal activation of this signaling pathway fosters cell growth, survival, development and differentiation [9]. In HNSCC, genes in the PI3K-pathway are often mutated, amplificated and overexpressed causing aberrant signaling [10]. This affects normal cell growth, survival and differentiation contributing to development and maintenance of cancer. Numerous genetic alterations of upstream and downstream factors have currently been clarified. However, their predictive value has yet to be established.
The ‘mammalian target of rapamycin’ (mTOR) is part of the PI3K/AKT/mTOR-pathway and is a serine/threonine kinase which mediates cellular homeostasis and growth [11, 12]. mTOR is activated by phosphorylation (p-mTOR). Aberrant mTOR signaling is commonly observed in cancer, making it an interesting therapeutic target. mTOR-inhibition as therapy for HNSCC was reviewed in several clinical trials. Tumor response improved after treatment with mTOR-inhibition in combination with other agents [13]. Increased activation of mTOR is associated with worse survival in several types of cancer [14,15,16,17,18,19]. Also for oral, tongue and esophageal SCC, mTOR-expression is associated with worse survival [20, 21].
Phosphatase and tensin homolog (PTEN) is a protein encoded by the PTEN tumor suppressor gene [22]. PTEN is a natural inhibitor of the PI3K pathway and thereby a tumor suppressor gene. Loss of PTEN results in PI3K/AKT/mTOR pathway overactivity. PTEN mutations have been described in several tumor types [23,24,25,26]. Loss of PTEN on protein level correlates with a worse prognosis in breast, prostate and lung cancers [27,28,29]. In HNSCC, PTEN mutations are present in 5–10% of the patients [30,31,32]. Also for tongue cancer, loss of PTEN on protein level is associated with worse survival [33, 34].
Apart from the PI3K/AKT/mTOR pathway, the Ras/Raf/MEK/ERK pathway also contributes to cell cycle proliferation. Phosphorylated ERK (p-ERK) phosphorylates cytoskeletal proteins, kinases and several transcriptional factors [35], leading to cellular survival, proliferation, differentiation and angiogenesis [36]. ERK expression correlated with worse survival in several types of cancer [37,38,39,40,41]. In nasopharyngeal carcinoma, high p-ERK expression correlates with worse survival [42].
In this study, we assess the predictive value of p-mTOR, p-ERK and PTEN expression in a cohort of patients with HPV-negative oropharyngeal, hypopharyngeal and laryngeal SCC who were treated with primary chemoradiotherapy. Moreover, we assess the p-mTOR expression and mTOR inhibition response by everolimus in a cohort of HNSCC organoids.
Materials and Methods
Patients and Clinical Data
This study uses a retrospective cohort of patients with HNSCC, treated at the University Medical Center (UMC) Utrecht described previously by de Ruiter et al. [43]. Inclusion criteria were: HPV-negative oropharyngeal, hypopharyngeal and laryngeal SCC (1), treated with radiotherapy and concomitant cisplatin, carboplatin or cetuximab with curative aim (2) whereof both clinical response data and tumor tissue was available (3). Exclusion criteria were: previous radiotherapy in the head and neck region, complete surgical resection of tumor, presence of distant metastases, presence of a prognosis-affecting double or prior malignancy. The following clinical data were collected: age, sex, tumor site, T and N stage.
All patients were treated with primary chemoradiotherapy. Standard treatment consisted of 35 fractions of 2 Gy (total 70 Gy) on both the primary tumor and positive lymph nodes. An elective total dose of 46–57.75 Gy on other lymph nodes, combined with 3 cycles of cisplatin or carboplatin administered intravenously every three weeks, or weekly cetuximab intravenously.
Tissue Microarray Construction and Immunohistochemistry
Pre-treatment biopsies were collected from every patient and were formalin fixed and paraffin embedded (FFPE). To determine representative tumor regions, sections of the FFPE blocks were stained with hematoxylin and eosin and assessed by a head and neck pathologist (SW). From these tumor regions, three tissue cores of 0.6 mm were obtained from the FFPE blocks and collected in a tissue microarray (TMA). The TMA was constructed using an automated tissue microarray instrument as described before [44]. TMA tissue sections (4 µm) were immunohistochemically stained with antibodies for the following antigens: phospho-mTOR (Ser2448; 49F9; 1:300; Cell Signaling), phospho-MAPK (ERK1/2) (p42/44; D13.14.4E; 1:400; Cell Signaling), PTEN (138G6; 1:100; Cell signaling). All antibodies were visualized with 3,3′-diaminobenzidine (DAB) chromagen and hematoxylin was used for counterstaining. Like TMA’s, organoids were FFPE and stained for phosphor-mTOR as described above.
HPV Detection
All patients in this study had a HPV-negative tumor. Tumors were stained for p16 INK4a by immunohistochemistry (JC8, 1:1200, Immunologic) and considered HPV-negative if less than 70% of tumor cells stained positive. Presence of HPV-DNA was tested in p16 positive tumors by PCR. These tumors were excluded if high-risk HPV-DNA was detected [45].
Immunohistochemical Analysis
The staining assessment was performed by a head and neck researcher (EDR) and a dedicated head and neck pathologist (SW), who were blinded for clinical outcome. Discrepancies were resolved by consensus. For each marker, staining intensity (0–3) and the percentage of stained tumor cells (0–100%) were scored. Cells were considered positive for p-mTOR and PTEN if expression was observed in the cytoplasm. Scoring of p-ERK was based on expression in the cytoplasm and in the nucleus. For organoids, expression of p-mTOR was scored in the same way as described above.
Organoids and Everolimus
HNSCC organoids from oral cavity and larynx were cultured as described earlier by Driehuis et al. [46] and Millen et al. [47] Organoids were treated with everolimus (LC Laboratories, catalog no. E4040) an mTOR inhibitor. This drugscreen was described in detail by Driehuis et al. previously [46]. The Biobank Research Ethics Committee of the University Medical Center Utrecht (TCBio) approved the biobanking protocol: 12-093 HUB-Cancer according to the University Medical Center Utrecht (UMCU) Biobanking Regulation. All donors participating in this study signed informed-consent forms and can withdraw their consent at any time.
Statistical Analysis
For each TMA core, a H-score was calculated by multiplying the intensity with the percentage of positive cells resulting in scores ranging from 0 to 300 [48]. The H-score for each tumor was calculated by averaging their corresponding TMA cores. Tumors were excluded from analysis if less than two TMA cores were assessable. Of patients where three TMA cores were available, intraclass correlation coefficients (ICCs) were calculated. A model with two-way mixed-effects was used [49].
The expression p-mTOR, p-ERK and PTEN was correlated to overall survival (OS), disease-free survival (DFS) and locoregional control (LRC). OS was defined as the number of days between the date of inclusion (first hospital visit before start of treatment) and date of death. DFS and LRC were defined as the number of days between the last day of radiotherapy and recurrence of the disease or date of death. Patients were censored at the date of last visit in case of absence of an event.
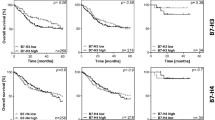
Expression of biomarkers was correlated with clinical variables. The correlation between tumor site and biomarker expression was assessed using a Kruskal–Wallis test. For dichotomous variables and biomarker expression Mann–Whitney U tests were used. Correlation of age and biomarker expression was assessed with a Spearman’s rank correlation coefficient (Fig. 1). Univariate and multivariate cox proportional hazard regressions were used to assess the correlation of biomarker expression with OS, DFS and LRC. The multivariate model contained: biomarker as predictor corrected for age, gender, T-stage and N-stage. Statistical analysis was performed with SPSS Statistics (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). The prognostic value of p-mTOR, p-ERK and PTEN expression was visualized by Kaplan–Meier curves comparing tumors with high and low biomarker expression stratified by the median value (Fig. 2, Supplementary Figs. 2, 3). A spearman’s rank-order correlation was run to assess the Correlation between p-mTOR and PTEN.
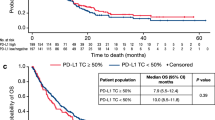
For organoids a H-score of p-mTOR was calculated as described above. Response to everolimus was extracted using the Area Under the Curve (AUC) in the dose–response curve (Fig. 3). A spearman’s rank-order correlation was run to assess the relationship between H-score of p-mTOR expression and AUC of everolimus response in all HNSCC organoids.
A Example of an everolimus dose–response curve depicted in blue with corresponding Area Under the Curve (AUC) shown in red. Everolimus dose increases on x-axis to the right. Organoid viability decreases if value on Y-axis is lower. B correlation of organoid response to everolimus (Y-axis) to H-score p-mTOR expression (X-axis)
Results
Patient Characteristics
A total of 77 patients with a mean age of 61.4 years were included for analysis: 48 with oropharyngeal, 16 with hypopharyngeal and 13 with laryngeal cancer. The 3- and 5-year OS of the patient cohort was 46% and 31%, respectively. The patient characteristics are described in Table 1.
All patients were treated with radiotherapy in combination with cisplatin (n = 53), carboplatin (n = 3) or cetuximab (n = 21).
A total of 8 HNSCC organoids were established including oral cavity (n = 6), larynx (n = 2).
Immunohistochemistry
Of each tumor, three tissue cores were included in the TMA. However, some tissue cores were lost during processing or didn’t contain sufficient tumor cells. Cases were excluded if there were less than 2 out of 3 cores assessable. Consequently, for p-mTOR, 75 cases were eligible for inclusion, for p-ERK 69 cases, and for PTEN 72 cases.
Representative images of TMA cores containing low and high expression of each marker are displayed in Fig. 1. Boxplots were generated to represent the distribution of the scoring data of each marker (Supplementary Fig. 1). The median H-scores per marker of the patient cohort and organoids with corresponding interquartile ranges are displayed in Supplementary Table 1.
ICCs were calculated for three TMA cores from the same patients. Three TMA cores were available for p-mTOR (n = 57, 76%), p-ERK (n = 48, 70%) and PTEN (n = 51, 71%). ICC for p-mTOR cases was 0.83 (95%CI 0.73–0.89), for p-ERK cases 0.78 (95%CI 0.65–0.87) and for PTEN cases 0.88 (95%CI 0.81–0.93). ICCs for all three markers are therefore considered good [49].
Correlation Clinicopathologic Parameters
No significant correlations between clinicopathologic parameters and immunohistochemical expression of p-mTOR, p-ERK and PTEN were observed. The results of all correlations are displayed in Supplementary Table 2. None of the clinical variables showed a correlation with OS, DFS and LRC (Table 2).
p-mTOR Expression
A 10-point p-mTOR H-score increase correlated significantly with a worse OS in univariate analysis (HR 1.06, 95%CI 1.01–1.11, p = 0.03) (Table 2), sub analysis of the Cisplatin/Carboplatin group showed this worse OS likewise (HR 1.08, 95%CI 1.01–1.15, p = 0.02) (Table 3). In multivariate analysis a 10-point p-mTOR H-score increase remained independently correlated with worse OS in the whole patient cohort (HR 1.06, 95%CI 1.01–1.11, p = 0.03) (Table 2) as well as in the cisplatin/carboplatin group (HR 1.09, 95%CI 1.02–1.16, p = 0.02) (Table 3).
10-point p-mTOR H-score increase did not correlate with DFS and LRC in univariate and multivariate analysis in the patient cohort (Table 2). However, sub analysis of the cisplatin/carboplatin group showed a significant correlation with worse DFS in multivariate analysis (HR 1.06, 95%CI 1.00–1.12, p = 0.04) (Table 3). The prognostic value of p-mTOR in a Kaplan–Meier curve is displayed in Fig. 2. Sub analysis per subsite is displayed in Supplementary Table 3.
p-ERK Expression
10-point p-ERK H-score increase correlated significantly with worse DFS in univariate analysis in the patient cohort (HR 1.03, 95%CI 1.00–1.05, p = 0.04 (Table 2) and in the cisplatin/carboplatin group (HR 1.03, 95%CI 1.00–1.07, p = 0.04) (Table 3). In multivariate analysis 10-point p-ERK H-score increase did not remain independently correlated with DFS, although trends were observed: whole patient cohort (HR 1.02, 95%CI 0.99–1.05, p = 0.07 (Table 2) and cisplatin/carboplatin group (HR 1.03, 95%CI 1.00–1.06, p = 0.08) (Table 3).
10 point p-ERK H-score increase did not correlate with OS and LRC in uni – and multivariate analysis. However trends were observed for worse LRC in univariate analysis; whole patient cohort (HR 1.03, 95%CI 1.00–1.06, p = 0.08) (Table 2) and cisplatin/carboplatin group (HR 1.03 95%CI 1.00–1.08, p = 0.08) (Table 3). The prognostic value of p-ERK in a Kaplan–Meier curve is displayed in Supplementary Fig. 2. Sub analysis per subsite is displayed in Supplementary Table 3.
PTEN-Expression
10 point PTEN H-score increase did not correlate with OS, DFS and LRC. Though, a trend was observed in the cisplatin/carboplatin group for worse OS in univariate (HR 1.09, 95%CI 0.99–1.20, p = 0.07) (Table 3) and in multivariate analysis (HR 1.10, 95%CI 1.00–1.21, p = 0.06) (Table 3). The prognostic value of PTEN in a Kaplan–Meier curve is displayed in Supplementary Fig. 3. Sub analysis per subsite is displayed in Supplementary Table 3.
Everolimus Organoid Response
The mean AUC of the organoids was 177.2 (95%CI 120.9–233.4). The mean H-score op p-mTOR expression in the organoids was 90.6 (95%CI 51.5–129.7). There was a statistically significant negative correlation between H-score and AUC Rs = − 0.731, p = 0.04 (Spearman’s rank order correlation), indicating a lower AUC (less organoid viability interpreted as better response to everolimus) correlates with a higher expression of p-mTOR measured as H-score.
Discussion
HNSCC-survival only marginally improved over the last decades [5]. Therefore, there is a need for prognostic and predictive biomarkers for long-time survival that can help to guide treatment decisions and might lead to the development of new therapies [6, 7]. In this study we determined p-mTOR, PTEN and p-ERK expression and correlated it with survival in patients with HPV-negative oropharyngeal, hypopharyngeal and laryngeal SCC, treated with primary chemoradiotherapy and assessed p-mTOR expression and everolimus response in a subset of HNSCC organoids.
In solid tumors, mTOR is often activated [50]. The prognostic value of mTOR expression is still unclear. This study demonstrates in multivariate analysis that higher p-mTOR expression correlates with worse OS in a homogeneous cohort of 75 HNSCC patients. Several other studies also investigated the prognostic value of mTOR in HNSCC. For oral SCC, high p-mTOR expression correlated with poor survival in two studies [51, 52]. Li et al. investigated p-mTOR expression in patients with tongue SCC and found a worse overall survival with higher p-mTOR expression [21]. For laryngeal SCC, one study showed that high p-S6 expression, a surrogate marker of mTORC1 activation, correlated with improved survival [53]. This is not in line with the studies mentioned above, however, the investigated marker was different from p-mTOR. Although several subsites of HNSCC were examined, results are inconclusive.
Our study only included HPV-negative patients. HPV-positive patients are considered a separate group of HNCC and appear to have an increased survival [54, 55]. Wilson et al. assessed the prognostic value of mTOR in both HPV-negative and HPV-positive patients and found that high mTOR expression correlated with worse outcome in HPV-negative patients, which is in line with our findings. For HPV-positive patients they were not able to correlate mTOR expression with outcome [56]. This could be because HPV-positive patients harbor significantly less p53 mutations compared to HPV-negative patients [57] and, once activated, p53 is known to inhibit the activity of mTOR [58]. There are several studies that assessed the prognostic value of mTOR. Most of the studies included patients receiving postoperative chemotherapy and/or radiotherapy, which is different from our study that only included patients treated with primary chemoradiotherapy. The results of this study are in line with aforementioned studies [21, 51, 52], indicating that mTOR expression correlates with worse overall survival.
In addition to p-mTOR expression in patients, we investigated p-mTOR expression in a panel of HNSCC organoids. Here we show that HNSCC organoids express p-mTOR on protein level and that the expression, depicted in H-score, is comparable with p-mTOR expression in our patient cohort (Supplementary Fig. 1). As mTOR is a potential target for targeted therapy we assessed everolimus response in 8 HNSCC organoids and investigated if p-mTOR expression correlated with everolimus response. Despite the small sample size we demonstrated a correlation of p-mTOR expression and everolimus response. This finding underscores that organoid-platforms are suitable to perform biomarker research, validation and assessment of targeted therapies in HNSCC [46, 47].
As PTEN loss is more often seen in an aggressive tumor-type [59] it could explain the worse survival in HNSCC [33, 34]. Malfunctioning leads to overactivity of the AKT/mTOR signaling pathway, and a correlation between loss of PTEN and worse survival seems logical. However, the results of this study do not support this hypothesis. Patients with lower PTEN tumor expression even have a tendency to improved OS (p = 0.11). This could be explained by ignition of negative feedback loops by AKT/mTOR overexpression leading to higher PTEN expression in response [60]. In our cohort, sub analysis shows a statistically significant positive correlation between p-mTOR and PTEN expression Rs = 0.245, p = 0.04 which supports this hypothesis.
Lee et al. found worse survival in case of PTEN loss in patients with oral tongue SCCs receiving surgery [33]. Compared to this study, they investigated a different treatment modality and a different subsite. Additionally, PTEN expression can differ per subsite [61]. Also scoring systems of PTEN expression differ. Lee et al. compare PTEN expression in tumor and normal tissue to assess PTEN-loss [33]. Zhao et al. use four percentage categories of PTEN expressing cells combined with staining intensity [34] and our study uses a continuous scale for assessing the percentage of PTEN expressing cells multiplied by the staining intensity ranging from 0 to 3. These different scoring systems indicate a lack of standard approach. Furthermore, in literature, the terms ‘PTEN-expression’ and ‘PTEN-loss’ are used interchangeably and both arguments make it hard to compare results not supporting generalizability. In other tumor types, loss of PTEN expression has been linked to advanced stage disease [27,28,29] which in our study was not assessable as we only included advanced stage HNSCC. Overall, studies investigating PTEN expression report different findings for HNSCC.
The Ras/Raf/MEK/ERK pathway also contributes to cell cycle proliferation [35]. Activation results in cellular survival, proliferation, differentiation and angiogenesis [36]. P-ERK is one of the last steps in the pathway making it an interesting therapeutic target. ERK expression correlates with worse overall survival in several types of cancer [37,38,39,40,41].
For HNSCC, this study demonstrates that high p-ERK expression correlates with a worse DFS only in univariate analysis and not in the multivariate model (p = 0.07). The value of p-ERK as prognostic biomarker was analyzed in a few other studies. p-ERK expression correlated with a worse overall survival in nasopharyngeal carcinoma [42], esophageal SCC [62] and oral tongue SCC [63]. In contrast, the study of Psyrri et al. showed an improved overall survival with high ERK expression in patients with oral cavity, oropharyngeal, hypopharyngeal and laryngeal SCC [64]. Although this finding indicates the opposite, this correlation applies for the unphosphorylated ERK expression. Computational biology studies indicate that ERK is inversely correlated with p-ERK [65], meaning low levels of ERK correspond with high levels of p-ERK. With this in mind, the findings of Psyrri et al. [64] are in line with the aforementioned studies [42, 62, 63]. Since this study is partially in line with literature, p-ERK may be considered a possible prognostic biomarker for HNSCC.
A limitation of this study is the application of TMA’s that only partially represent the whole character of the tumor, which is inevitable in daily clinical practice after obtaining tissue biopsies. To overcome this issue, three TMA cores were taken per patient whereby the heterogeneity within the tumor biopsy is taken into account [66].
Conclusion
This study shows that high p-mTOR expression predicts and p-ERK expression tends to predict worse treatment outcome in a cohort of advanced stage, HPV negative HNSCC patients treated with chemoradiation, providing additional evidence that these markers are candidate prognostic biomarkers for survival in this patient population. Also this study shows that the use of HNSCC organoids for biomarker research has potential. The role of PTEN expression as prognostic biomarker remains unclear, as consistent evidence on its prognostic and predictive value is lacking.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Consent for Publication
For this type of study consent for publication is not required.
Stats Declaration
Statistical methods employed are performed by an experienced person, with authorship (acknowledgement) on the manuscript, and the contributor(s) specified.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/CAAC.21660
Chen J, Eisenberg E, Krutchkoff DJ, Katz RV (1991) Changing trends in oral cancer in the United States, 1935 to 1985: a Connecticut study. J Oral Maxillofac Surg 49(11):1152–1158. https://doi.org/10.1016/0278-2391(91)90406-C
Ostman J, Anneroth G, Gustafsson H, Tavelin B (1995) Malignant oral tumours in Sweden 1960–1989–an epidemiological study. Eur J Cancer B Oral Oncol 31B(2):106–112. https://doi.org/10.1016/0964-1955(94)00018-y
Muir C, Weiland L (1995) Upper aerodigestive tract cancers. Cancer 75(1 Suppl):147–153. https://doi.org/10.1002/1097-0142(19950101)75:1+%3c147::AID-CNCR2820751304%3e3.0.CO;2-U
Haddad RI, Shin DM (2008) Recent advances in head and neck cancer. N Engl J Med 359(11):1143. https://doi.org/10.1056/NEJMra0707975
Weber RS, Lewis CM, Eastman SD et al (2010) Quality and performance indicators in an academic department of head and neck surgery. Arch Otolaryngol Head Neck Surg 136(12):1212–1218. https://doi.org/10.1001/archoto.2010.215
Hessel AC, Moreno MA, Hanna EY et al (2010) Compliance with quality assurance measures in patients treated for early oral tongue cancer. Cancer 116(14):3408–3416. https://doi.org/10.1002/cncr.25031
Lui VWY, Hedberg ML, Li H et al (2013) Frequent mutation of the PI3K pathway in head and neck cancer defines predictive biomarkers. Cancer Discov 3(7):761–769. https://doi.org/10.1158/2159-8290.CD-13-0103
Cantley LC (2002) The phosphoinositide 3-kinase pathway. Science 296(5573):1655–1657. https://doi.org/10.1126/science.296.5573.1655
Cai Y, Dodhia S, Su GH (2017) Dysregulations in the PI3K pathway and targeted therapies for head and neck squamous cell carcinoma. Oncotarget 8(13):22203–22217. https://doi.org/10.18632/oncotarget.14729
Wullschleger S, Loewith R, Hall MN (2006) TOR signaling in growth and metabolism. Cell 124(3):471–484. https://doi.org/10.1016/j.cell.2006.01.016
Shaw RJ, Cantley LC (2006) Ras, PI(3)K and mTOR signalling controls tumour cell growth. Nature 441(7092):424–430. https://doi.org/10.1038/nature04869
Patel J, Nguyen SA, Ogretmen B, Gutkind JS, Nathan C, Day T (2020) mTOR inhibitor use in head and neck squamous cell carcinoma: a meta-analysis on survival, tumor response, and toxicity. Laryngoscope Investig Otolaryngol 5(2):243–255. https://doi.org/10.1002/lio2.370
Zhou L, Huang Y, Li J, Wang Z (2010) The mTOR pathway is associated with the poor prognosis of human hepatocellular carcinoma. Med Oncol 27(2):255–261. https://doi.org/10.1007/s12032-009-9201-4
Bakarakos P, Theohari I, Nomikos A et al (2010) Immunohistochemical study of PTEN and phosphorylated mTOR proteins in familial and sporadic invasive breast carcinomas. Histopathology 56(7):876–882. https://doi.org/10.1111/j.1365-2559.2010.03570.x
Sun CH, Chang YH, Pan CC (2011) Activation of the PI3K/Akt/mTOR pathway correlates with tumour progression and reduced survival in patients with urothelial carcinoma of the urinary bladder. Histopathology 58(7):1054–1063. https://doi.org/10.1111/j.1365-2559.2011.03856.x
Xu DZ, Geng QR, Tian Y et al (2010) Activated mammalian target of rapamycin is a potential therapeutic target in gastric cancer. BMC Cancer 10(1):1–10. https://doi.org/10.1186/1471-2407-10-536
Herberger B, Puhalla H, Lehnert M et al (2007) Activated mammalian target of rapamycin is an adverse prognostic factor in patients with biliary tract adenocarcinoma. Clin Cancer Res 13(16):4795–4799. https://doi.org/10.1158/1078-0432.CCR-07-0738
Liu D, Huang Y, Chen B et al (2011) Activation of mammalian target of rapamycin pathway confers adverse outcome in nonsmall cell lung carcinoma. Cancer 117(16):3763–3773. https://doi.org/10.1002/cncr.25959
Hirashima K, Baba Y, Watanabe M et al (2010) Phosphorylated mTOR expression is associated with poor prognosis for patients with esophageal squamous cell carcinoma. Ann Surg Oncol 17(9):2486–2493. https://doi.org/10.1245/s10434-010-1040-1
Li S-H, Chien C-Y, Huang W-T et al (2017) Prognostic significance and function of mammalian target of rapamycin in tongue squamous cell carcinoma. Sci Rep 7(1):8178. https://doi.org/10.1038/s41598-017-08345-8
Steck PA, Pershouse MA, Jasser SA et al (1997) Identification of a candidate tumour suppressor gene, MMAC1, at chromosome 10q23.3 that is mutated in multiple advanced cancers. Nat Genet 15(4):356–362. https://doi.org/10.1038/ng0497-356
Cairns P, Okami K, Halachmi S et al (1997) Frequent inactivation of PTEN/MMAC1 in primary prostate cancer. Cancer Res 57(22):4997–5000
Tsao H, Zhang X, Benoit E, Haluska FG (1998) Identification of PTEN/MMAC1 alterations in uncultured melanomas and melanoma cell lines. Oncogene 16(26):3397–3402. https://doi.org/10.1038/sj.onc.1201881
Duerr EM, Rollbrocker B, Hayashi Y et al (1998) PTEN mutations in gliomas and glioneuronal tumors. Oncogene 16(17):2259–2264. https://doi.org/10.1038/sj.onc.1201756
Perren A, Weng LP, Boag AH et al (1999) Immunohistochemical evidence of loss of PTEN expression in primary ductal adenocarcinomas of the breast. Am J Pathol 155(4):1253–1260. https://doi.org/10.1016/S0002-9440(10)65227-3
Depowski PL, Rosenthal SI, Ross JS (2001) Loss of expression of the PTEN gene protein product is associated with poor outcome in breast cancer. Mod Pathol 14(7):672–676. https://doi.org/10.1038/modpathol.3880371
McMenamin ME, Soung P, Perera S, Kaplan I, Loda M, Sellers WR (1999) Loss of PTEN expression in paraffin-embedded primary prostate cancer correlates with high Gleason score and advanced stage. Cancer Res 59(17):4291–4296
Tang JM, He QY, Guo RX, Chang XJ (2006) Phosphorylated Akt overexpression and loss of PTEN expression in non-small cell lung cancer confers poor prognosis. Lung Cancer 51(2):181–191. https://doi.org/10.1016/j.lungcan.2005.10.003
Stransky N, Egloff AM, Tward AD et al (2011) The mutational landscape of head and neck squamous cell carcinoma. Source Sci New Ser 333(6046):1157–1160. https://doi.org/10.1126/science.l206923
Poetsch M, Lorenz G, Kleist B (2002) Detection of new PTEN/MMAC1 mutations in head and neck squamous cell carcinomas with loss of chromosome 10. Cancer Genet Cytogenet 132(1):20–24. https://doi.org/10.1016/S0165-4608(01)00509-X
Shao X, Tandon R, Samara G et al (1998) Mutational analysis of the PTEN gene in head and neck squamous cell carcinoma. Int J Cancer 77(5):684–688. https://doi.org/10.1002/(SICI)1097-0215(19980831)77:5%3c684::AID-IJC4%3e3.0.CO;2-R
Lee JI, Soria JC, Hassan KA et al (2001) Loss of PTEN expression as a prognostic marker for tongue cancer. Arch Otolaryngol-Head Neck Surg 127(12):1441–1445. https://doi.org/10.1001/archotol.127.12.1441
Zhao J, Chi J, Gao M, Zhi J, Li Y, Zheng X (2017) Loss of PTEN expression is associated with high MicroRNA 24 level and poor prognosis in patients with tongue squamous cell carcinoma. J Oral Maxillofac Surg 75(7):1449.e1-1449.e8. https://doi.org/10.1016/j.joms.2017.03.025
Wortzel I, Seger R (2011) The ERK cascade: Distinct functions within various subcellular organelles. Genes Cancer 2(3):195–209. https://doi.org/10.1177/1947601911407328
Gough NR (2011) MAPK signaling focus issue: recruiting players for a game of ERK. Sci Signal. 4(196):9. https://doi.org/10.1126/scisignal.2002601
Bartholomeusz C, Gonzalez-Angulo AM, Liu P et al (2012) High ERK protein expression levels correlate with shorter survival in triple-negative breast cancer patients. Oncologist 17(6):766–774. https://doi.org/10.1634/theoncologist.2011-0377
Schmitz KJ, Wohlschlaeger J, Lang H et al (2008) Activation of the ERK and AKT signalling pathway predicts poor prognosis in hepatocellular carcinoma and ERK activation in cancer tissue is associated with hepatitis C virus infection. J Hepatol 48(1):83–90. https://doi.org/10.1016/j.jhep.2007.08.018
Oba J, Nakahara T, Abe T, Hagihara A, Moroi Y, Furue M (2011) Expression of c-Kit, p-ERK and cyclin D1 in malignant melanoma: an immunohistochemical study and analysis of prognostic value. J Dermatol Sci 62(2):116–123. https://doi.org/10.1016/j.jdermsci.2011.02.011
Fujimori Y, Inokuchi M, Takagi Y, Kato K, Kojima K, Sugihara K (2012) Prognostic value of RKIP and P-ERK in gastric cancer. J Exp Clin Cancer Res 31(1):1–8. https://doi.org/10.1186/1756-9966-31-30
Chadha KS, Khoury T, Yu J et al (2006) Activated Akt and Erk expression and survival after surgery in pancreatic carcinoma. Ann Surg Oncol 13(7):933–939. https://doi.org/10.1245/ASO.2006.07.011
Wang SS, Guan ZZ, Xiang YQ et al (2006) Significance of EGFR and p-ERK expression in nasopharyngeal carcinoma. Zhonghua Zhong Liu Za Zhi 28(1):28–31
de Ruiter EJ, de Roest RH, Brakenhoff RH et al (2020) Digital pathology-aided assessment of tumor-infiltrating T lymphocytes in advanced stage, HPV-negative head and neck tumors. Cancer Immunol Immunother 69(4):581–591. https://doi.org/10.1007/s00262-020-02481-3
van Kempen PMW, van Bockel L, Braunius WW et al (2014) HPV-positive oropharyngeal squamous cell carcinoma is associated with TIMP3 and CADM1 promoter hypermethylation. Cancer Med 3(5):1185–1196. https://doi.org/10.1002/cam4.313
Smeets SJ, Hesselink AT, Speel EJM et al (2007) A novel algorithm for reliable detection of human papillomavirus in paraffin embedded head and neck cancer specimen. Int J Cancer 121(11):2465–2472. https://doi.org/10.1002/ijc.22980
Driehuis E, Kolders S, Spelier S et al (2019) Oral mucosal organoids as a potential platform for personalized cancer therapy. Cancer Discov 9(7):852–871. https://doi.org/10.1158/2159-8290.CD-18-1522
Millen R, De Kort WWB, Koomen M et al (2023) Patient-derived head and neck cancer organoids allow treatment stratification and serve as a tool for biomarker validation and identification. Med 4(5):290-310.e12. https://doi.org/10.1016/j.medj.2023.04.003
McCarty KS, Miller LS, Cox EB, Konrath J, McCarty KS (1985) Estrogen receptor analyses. Correlation of biochemical and immunohistochemical methods using monoclonal antireceptor antibodies. Arch Pathol Lab Med 109(8):716–721
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Sabatini DM (2006) mTOR and cancer: insights into a complex relationship. Nat Rev Cancer 6(9):729–734. https://doi.org/10.1038/nrc1974
Monteiro LS, Delgado ML, Ricardo S et al (2013) Phosphorylated mammalian target of rapamycin is associated with an adverse outcome in oral squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol 115(5):638–645. https://doi.org/10.1016/j.oooo.2013.01.022
Naruse T, Yanamoto S, Yamada S et al (2015) Anti-tumor effect of the mammalian target of rapamycin inhibitor everolimus in oral squamous cell carcinoma. Pathol Oncol Res 21(3):765–773. https://doi.org/10.1007/s12253-014-9888-1
García-Carracedo D, Ángeles Villaronga M, Álvarez-Teijeiro S et al (2016) Impact of PI3K/AKT/mTOR pathway activation on the prognosis of patients with head and neck squamous cell carcinomas. Oncotarget 7(20):29780–29793. https://doi.org/10.18632/oncotarget.8957
Ang KK, Harris J, Wheeler R et al (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363(1):24–35. https://doi.org/10.1056/NEJMoa0912217
Fakhry C, Westra WH, Li S et al (2008) Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100(4):261–269. https://doi.org/10.1093/jnci/djn011
Wilson TG, Hanna A, Recknagel J, Pruetz BL, Baschnagel AM, Wilson GD (2020) Prognostic significance of MTOR expression in HPV positive and negative head and neck cancers treated by chemoradiation. Head Neck 42(2):153–162. https://doi.org/10.1002/hed.25983
Hong A, Zhang X, Jones D et al (2016) Relationships between p53 mutation, HPV status and outcome in oropharyngeal squamous cell carcinoma. Radiother Oncol 118(2):342–349. https://doi.org/10.1016/j.radonc.2016.02.009
Feng Z, Zhang H, Levine AJ, Jin S (2005) The coordinate regulation of the p53 and mTOR pathways in cells. Proc Natl Acad Sci USA 102(23):8204. https://doi.org/10.1073/PNAS.0502857102
Mastronikolis NS, Tsiambas E, Papadas TA et al (2017) Deregulation of PTEN expression in laryngeal squamous cell carcinoma based on tissue microarray digital analysis. Anticancer Res 37(10):5521–5524. https://doi.org/10.21873/anticanres.11983
Rozengurt E, Soares HP, Sinnet-Smith J (2014) Suppression of feedback loops mediated by pi3k/mtor induces multiple overactivation of compensatory pathways: an unintended consequence leading to drug resistance. Mol Cancer Ther 13(11):2477–2488. https://doi.org/10.1158/1535-7163.MCT-14-0330
Guney K, Ozbilim G, Derin AT, Cetin S (2007) Expression of PTEN protein in patients with laryngeal squamous cell carcinoma. Auris Nasus Larynx 34(4):481–486. https://doi.org/10.1016/j.anl.2007.03.014
Wang H, Zhang Y, Yun H, Chen S, Chen Y, Liu Z (2017) ERK expression and its correlation with STAT1 in esophageal squamous cell carcinoma. Oncotarget 8(28):45249–45258. https://doi.org/10.18632/oncotarget.16902
Theocharis S, Kotta-Loizou I, Klijanienko J et al (2014) Extracellular signal-regulated kinase (ERK) expression and activation in mobile tongue squamous cell carcinoma: associations with clinicopathological parameters and patients survival. Tumor Biol 35(7):6455–6465. https://doi.org/10.1007/s13277-014-1853-9
Psyrri A, Lee JW, Pectasides E et al (2014) Prognostic biomarkers in phase II trial of cetuximab-containing induction and chemoradiation in resectable HNSCC: Eastern Cooperative Oncology Group E2303. Clin Cancer Res 20(11):3023–3032. https://doi.org/10.1158/1078-0432.CCR-14-0113
Schoeberl B, Eichler-Jonsson C, Gilles ED, Muüller G (2002) Computational modeling of the dynamics of the MAP kinase cascade activated by surface and internalized EGF receptors. Nat Biotechnol 20(4):370–375. https://doi.org/10.1038/nbt0402-370
Goethals L, Perneel C, Debucquoy A et al (2006) A new approach to the validation of tissue microarrays. J Pathol 208(5):607–614. https://doi.org/10.1002/path.1934
Funding
This study was supported by the Dutch Cancer Society (Project number: A6C 7072).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, design, material preparation and data collection. Analysis were performed by WWBdeK, EJdR, WEH and SMW. The first draft of the manuscript was written by WWBdeK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
For the first part of the study with staining’s on residual material informed consent is not required. For the organoids the Biobank Research Ethics Committee of the University Medical Center Utrecht (TCBio) approved the biobanking protocol: 12-093 HUB-Cancer according to the University Medical Center Utrecht (UMCU) Biobanking Regulation. All donors participating in this study signed informed-consent forms and can withdraw their consent at any time.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Kort, W.W.B., de Ruiter, E.J., Haakma, W.E. et al. p-mTOR, p-ERK and PTEN Expression in Tumor Biopsies and Organoids as Predictive Biomarkers for Patients with HPV Negative Head and Neck Cancer. Head and Neck Pathol 17, 697–707 (2023). https://doi.org/10.1007/s12105-023-01576-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-023-01576-4