Abstract
Objectives
To evaluate the clinical, hormonal and genetic characteristics of 46XY disorders of sexual development (DSD) patients from South India.
Methods
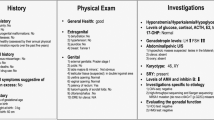
46XY DSD patients with a provisional diagnosis of 17β-hydroxysteroid dehydrogenase 3 (17BHSD3) deficiency, 5 alpha-reductase type 2 deficiency (5ARD2) or partial androgen insensitivity syndrome (PAIS) based on clinical and hormonal analysis were included in this study. All the patients underwent detailed clinical and hormonal evaluations. Targeted next-generation sequencing for all three genes (AR, HSD17B3, and SRD5A2) in parallel was carried out for all the included patients and their parents.
Results
Based upon the clinical and hormonal analysis, among the 37 children with 46XY DSD in the present study, 21 children were diagnosed with 5ARD2, 10 with PAIS, and six with 17BHSD3 deficiency. However, genetic analysis revealed pathogenic mutations in nine patients – six in the AR gene, two in the SRD5A2 gene, and one in the HSD17B3 gene. The concordance rate between provisional hormonal and genetic diagnosis was only 22.2%. Two out of six subjects with AR gene variants were positive for somatic mosaicism.
Conclusions
In the present study, a positive genetic diagnosis was detected in nine patients (24%), including five novel variants. In this study, mutations in the AR gene was the most reported. The authors did not find the testosterone: dihydrotestosterone (T: DHT) ratio to be an accurate hormonal diagnostic tool.



Similar content being viewed by others
References
Hughes IA, Houk C, Ahmed SF, Lee PA; Lawson Wilkins Pediatric Endocrine Society/European Society for Paediatric Endocrinology Consensus Group. Consensus statement on management of intersex disorders. J Pediatr Urol. 2006;2:148–62.
Délot EC, Vilain E. Towards improved genetic diagnosis of human differences of sex development. Nat Rev Genet. 2021;22:588–602.
Akcay T, Fernandez-Cancio M, Turan S, Güran T, Audi L, Bereket A. AR and SRD5A2 gene mutations in a series of 51 Turkish 46, XY DSD children with a clinical diagnosis of androgen insensitivity. Andrology. 2014;2:572–8.
Lee YS, Kirk JMW, Stanhope RG, et al. Phenotypic variability in 17β-hydroxysteroid dehydrogenase-3 deficiency and diagnostic pitfalls. Clin Endocrinol. 2007;67:20–8.
Hughes LA, McKay-Bounford K, Webb EA, et al. Next generation sequencing (NGS) to improve the diagnosis and management of patients with disorders of sex development (DSD). Endocr Connect. 2019;8:100–10.
Fan Y, Zhang X, Wang L, et al. Diagnostic application of targeted next-generation sequencing of 80 genes associated with disorders of sexual development. Sci Rep. 2017;7:44536.
Ahmed SF, Achermann JC, Arlt W, et al. UK guidance on the initial evaluation of an infant or an adolescent with a suspected disorder of sex development. Clin Endocrinol. 2011;75:12–26.
Ahmed SF, Khwaja O, Hughes IA. The role of a clinical score in the assessment of ambiguous genitalia. BJU Int. 2000;85:120–4.
Dixon J, Wallace AM, O’Toole S, Ahmed SF. Prolonged human chorionic gonadotrophin stimulation as a tool for investigating and managing undescended testes. Clin Endocrinol. 2007;67:816–21.
Ahmed SF, Achermann JC, Arlt W, et al. Society for Endocrinology UK guidance on the initial evaluation of an infant or an adolescent with a suspected disorder of sex development (revised 2015). Clin Endocrinol. 2016;84:771–88.
Hughes IA. Consequences of the Chicago DSD consensus: a personal perspective. Horm Metab Res. 2015;47:394–400.
Chapla A, Mruthyunjaya MD, Asha HS, et al. Maturity onset diabetes of the young in India - a distinctive mutation pattern identified through targeted next-generation sequencing. Clin Endocrinol. 2015;82:533–42.
Baidya A, Basu AK, Bhattacharjee R, et al. Diagnostic approach in 46, XY DSD: an Endocrine Society of Bengal (ESB) consensus statement. J Pediatr Endocrinol Metab. 2022;36:4–18.
Arya S, Barnabas R, Lila AR, et al. Clinical, hormonal, genetic, and molecular characteristics in androgen insensitivity syndrome in an Asian Indian cohort from a single centre in western India. Sex Dev. 2021;15:253–61.
Nagaraja MR, Rastogi A, Raman R, Gupta DK, Singh SK. Molecular diagnosis of 46, XY DSD and identification of a novel 8 nucleotide deletion in exon 1 of the SRD5A2 gene. J Pediatr Endocrinol Metab. 2010;23:379–85.
Tang Y, Chen Y, Wang J, et al. Clinical characteristics and genetic expansion of 46, XY disorders of sex development children in a Chinese prospective study. Endocr Connect. 2023;12:e230029.
Xie Q-G, Luo P, Xia K, et al. 46, XY disorders of sex development: the use of NGS for prevalent variants. Hum Genet. 2022;141:1863–73.
Kouri C, Sommer G, Flück CE. Oligogenic causes of human differences of sex development: facing the challenge of genetic complexity. Horm Res Paediatr. 2023;96:169–79.
Ittiwut C, Pratuangdejkul J, Supornsilchai V, et al. Novel mutations of the SRD5A2 and AR genes in Thai patients with 46, XY disorders of sex development. J Pediatr Endocrinol Metab. 2017;30:19–26.
Hornig NC, Holterhus P-M. Molecular basis of androgen insensitivity syndromes. Mol Cell Endocrinol. 2021;523:111146.
Köhler B, Lumbroso S, Leger J, et al. Androgen insensitivity syndrome: somatic mosaicism of the androgen receptor in seven families and consequences for sex assignment and genetic counseling. J Clin Endocrinol Metab. 2005;90:106–11.
Batista RL, Rodrigues ADS, Machado AZ, et al. Partial androgen insensitivity syndrome due to somatic mosaicism of the androgen receptor. J Pediatr Endocrinol Metab. 2018;31:223–8.
Maimoun L, Philibert P, Cammas B, et al. Phenotypical, biological, and molecular heterogeneity of 5α-reductase deficiency: an extensive international experience of 55 patients. J Clin Endocrinol Metab. 2011;96:296–307.
Shabir I, Khurana ML, Marumudi E, et al. Homozygous p.R246Q mutation and impaired spermatogenesis: long term follow-up of 4 children from one family with 5 alpha reductase 2 deficiency. Indian J Pediatr. 2016;83:481–2.
Kumar A, Sharma R, Faruq M, et al. Spectrum of pathogenic variants in SRD5A2 in Indian children with 46, XY disorders of sex development and clinically suspected steroid 5α-reductase 2 deficiency. Sex Dev. 2019;13:228–39.
Katz MD, Cai LQ, Zhu YS, et al. The biochemical and phenotypic characterization of females homozygous for 5 alpha-reductase-2 deficiency. J Clin Endocrinol Metab. 1995;80:3160–7.
Kumar A, Sharma R, Faruq M, et al. Clinical, biochemical, and molecular characterization of Indian children with clinically suspected androgen insensitivity syndrome. Sex Dev. 2022;16:34–45.
Imperato-McGinley J, Peterson RE, Gautier T, et al. Hormonal evaluation of a large kindred with complete androgen insensitivity: evidence for secondary 5 alpha-reductase deficiency. J Clin Endocrinol Metab. 1982;54:931–41.
Costa EMF, Domenice S, Sircili MH, Inacio M, Mendonca BB. DSD due to 5α-reductase 2 deficiency - from diagnosis to long term outcome. Semin Reprod Med. 2012;30:427–31.
Yu B, Liu Z, Mao J, et al. Novel mutations of HSD17B3 in three Chinese patients with 46, XY disorders of sex development. Steroids. 2017;126:1–6.
Author information
Authors and Affiliations
Contributions
RP, NN: Collection of clinical data, patient management and writing the manuscript; SK, JS, DN: Patient management, correction and review of the manuscript; LR: Genetic analysis and manuscript preparation; AC, NT: Genetic analysis, review and correction of the manuscript. SK will act as guarantor for this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Palui, R., Ravichandran, L., Kamalanathan, S. et al. Clinical, Hormonal, and Genetic Spectrum of 46 XY Disorders of Sexual Development (DSD) Patients. Indian J Pediatr (2024). https://doi.org/10.1007/s12098-024-05144-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12098-024-05144-8