Abstract
A chest radiograph is the most common and the initial radiological investigation for evaluating a child presenting with respiratory complaints. However, performing and interpreting chest radiography optimally requires training and skill. With the relatively easy availability of computed tomography (CT) scanning and more recently multidetector computed tomography (MDCT), these investigations are often performed. Although these can be the cross-sectional imaging modalities of choice in certain situations where detailed and exact anatomical and etiological information is required, both these investigations are associated with increased radiation exposure which has more detrimental effects on children, especially when repeated follow-up imaging is necessary to assess the disease status. Ultrasonography (USG) and magnetic resonance imaging (MRI) have evolved as radiation-free radiological investigations for evaluating the pediatric chest pathologies over the last few years. In the present review article, the utility and the current status, as well as the limitations of USG and MRI for evaluation of pediatric chest pathologies, are discussed. Radiology has grown beyond having just the diagnostic capabilities in managing children with chest disorders in the last two decades. Image-guided therapeutic procedures (percutaneous and endovascular) are routinely performed in children with pathologies in the mediastinum and lungs. The commonly performed image-guided pediatric chest interventions, including biopsies, fine needle aspiration, drainage procedures and therapeutic endovascular procedures, are also discussed in the current review.


Similar content being viewed by others
References
Jain R, Jana M, Gupta A, Naranje P. Ultrasonography in the evaluation of pediatric chest “masses”: When to consider? J Ultrasound Med. 2022;41:821–6.
Bhalla D, Naranje P, Jana M, Bhalla AS. Pediatric lung ultrasonography: Current perspectives. Pediatr Radiol. 2022;52:2038–50.
Hosokawa T, Honda M, Arakawa Y. Initial ultrasound evaluation of an anterior mediastinal mass ultimately diagnosed as T-cell acute lymphoblastic leukemia: A report of three cases in children. Radiol Case Rep. 2022;17:3639–45.
Bhalla D, Sinha P, Naranje P, et al. Transcutaneous mediastinal ultrasonography for lymphadenopathy in children: a pictorial essay of technique and imaging findings. J Ultrasound Med. 2022;41:773–83.
Jaworska J, Komorowska-Piotrowska A, Pomiećko A, et al. Consensus on the application of lung ultrasound in pneumonia and bronchiolitis in children. Diagnostics (Basel). 2020;10:935.
Yadav KK, Awasthi S, Parihar A. Lung ultrasound is comparable with chest roentgenogram for diagnosis of community-acquired pneumonia in hospitalised children. Indian J Pediatr. 2017;84:499–504.
Hajalioghli P, Nemati M, Dinparast Saleh L, Fouladi DF. Can chest computed tomography be replaced by lung ultrasonography with or without plain chest radiography in pediatric pneumonia? J Thorac Imaging. 2016;31:247–52.
Musolino AM, Tomà P, Supino MC, et al. Lung ultrasound features of children with complicated and noncomplicated community acquired pneumonia: A prospective study. Pediatr Pulmonol. 2019;54:1479–86.
Carrard J, Bacher S, Rochat-Guignard I, et al. Necrotizing pneumonia in children: Chest computed tomography vs. lung ultrasound. Front Pediatr. 2022;10:898402.
Rea G, Sperandeo M, Di Serafino M, Vallone G, Tomà P. Neonatal and pediatric thoracic ultrasonography. J Ultrasound. 2019;22:121–30.
Hiles M, Culpan AM, Watts C, Munyombwe T, Wolstenhulme S. Neonatal respiratory distress syndrome: Chest X-ray or lung ultrasound? A systematic review. Ultrasound. 2017;25:80–91.
Liu J, Cao H, Wang H, et al. The role of lung ultrasound in diagnosis of respiratory distress syndrome in newborn infants. Iran J Paediatr. 2014;24:147–54.
Raimondi F, Migliaro F, Sodano A, et al. Use of neonatal chest ultrasound to predict noninvasive ventilation failure. Pediatrics. 2014;134:e1089–94.
Lichtenstein D, Mauriat P. Lung ultrasound in the critically ill neonate. Curr Paediatr Rev. 2012;8:217–23.
Raimondi F, Migliaro F, Sodano A, et al. Can neonatal lung ultrasound monitor fluid clearance and predict the need of respiratory support? Crit Care. 2012;16:R220.
Irodi A, Leena RV, Prabhu SM, Gibikote S. Role of computed tomography in pediatric chest conditions. Indian J Pediatr. 2016;83:675–90.
Sodhi KS, Krishna S, Saxena AK, Sinha A, Khandelwal N, Lee EY. Clinical application of “Justification” and “Optimization” principle of ALARA in pediatric CT imaging: ‘How many children can be protected from unnecessary radiation?’ Eur J Radiol. 2015;84:1752–7.
Garg MK, Gupta P, Agarwal R, Sodhi KS, Khandelwal N. MRI: A new paradigm in imaging evaluation of allergic bronchopulmonary aspergillosis? Chest. 2015;147:e58–9.
Sodhi KS. Lung MRI in Children: The Road Less Travelled. Indian J Radiol Imaging. 2021;31:237–41.
Sodhi KS, Ciet P, Vasanawala S, Biederer J. Practical protocol for lung magnetic resonance imaging and common clinical indications. Pediatr Radiol. 2022;52:295–311.
Sodhi KS, Khandelwal N, Saxena AK, et al. Rapid lung MRI in children with pulmonary infections: Time to change our diagnostic algorithms. J Magn Reson Imaging. 2016;43:1196–206.
Sodhi KS, Khandelwal N, Saxena AK, et al. Rapid lung MRI - paradigm shift in evaluation of febrile neutropenia in children with leukemia: A pilot study. Leuk Lymphoma. 2016;57:70–5.
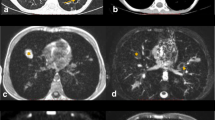
Sodhi KS, Gupta P, Shrivastav A, et al. Evaluation of 3 T lung magnetic resonance imaging in children with allergic bronchopulmonary aspergillosis: Pilot study. Eur J Radiol. 2019;111:88–92.
Sodhi KS, Sharma M, Lee EY, et al. Diagnostic utility of 3T Lung MRI in children with interstitial lung disease: A prospective pilot study. Acad Radiol. 2018;25:380–6.
Rana P, Sodhi KS, Bhatia A, Saxena AK, Suri D, Singh S. Diagnostic accuracy of 3-T lung magnetic resonance imaging in human immunodeficiency virus-positive children. Pediatr Radiol. 2020;50:38–45.
Sodhi KS, Sharma M, Saxena AK, Mathew JL, Singh M, Khandelwal N. MRI in thoracic tuberculosis of children. Indian J Pediatr. 2017;84:670–6.
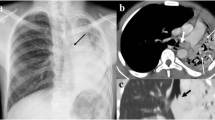
Sodhi KS, Bhatia A, Samujh R, Mathew JL, Lee EY. Prospective comparison of MRI and contrast-enhanced MDCT for evaluation of pediatric pulmonary hydatid disease: added diagnostic value of MRI. AJR Am J Roentgenol. 2019;212:982–7.
Sodhi KS, Bhatia A, Lee EY. Prospective Evaluation of Free-Breathing Fast T2-Weighted MultiVane XD Sequence at 3-T MRI for Large Airway Assessment in Pediatric Patients. AJR Am J Roentgenol. 2021;216:1074–80.
Sodhi KS, Bhatia A, Nichat V, et al. Chest MRI as an emerging modality in the evaluation of empyema in children with specific indications: Pilot study. Pediatr Pulmonol. 2021;56:2668–75.
Dournes G, Walkup LL, Benlala I, et al. The clinical use of lung mri in cystic fibrosis: What, now, how? Chest. 2021;159:2205–17.
Hayes-Jordan A, Connolly B, Temple M, et al. Image-guided percutaneous approach is superior to the thoracoscopic approach in the diagnosis of pulmonary nodules in children. J Pediatr Surg. 2003;38:745–8.
Cahill AM, Baskin KM, Kaye RD, Fitz CR, Towbin RB. CT-guided percutaneous lung biopsy in children. J Vasc Interv Radiol. 2004;15:955–60.
Fontalvo LF, Amaral JG, Temple M, et al. Percutaneous US-guided biopsies of peripheral pulmonary lesions in children. Pediatr Radiol. 2006;36:491–7.
Shah JH, Whitmore MJ. Interventional radiology's role in the treatment of pediatric thoracic disease. Semin Roentgenol. 2019;54:395–406.
Han Y, Kim HJ, Kong KA, et al. Diagnosis of small pulmonary lesions by transbronchial lung biopsy with radial endobronchial ultrasound and virtual bronchoscopic navigation versus CT-guided transthoracic needle biopsy: A systematic review and meta-analysis. PLoS ONE. 2018;13:e0191590.
Huo YR, Chan MV, Habib AR, Lui I, Ridley L. Post-biopsy manoeuvres to reduce pneumothorax incidence in CT-guided transthoracic lung biopsies: A systematic review and meta-analysis. Cardiovasc Intervent Radiol. 2019;42:1062–72.
Balfour-Lynn IM, Abrahamson E, Cohen G, et al; Paediatric Pleural Diseases Subcommittee of the BTS Standards of Care Committee. BTS guidelines for the management of pleural infection in children. Thorax. 2005;60:i1–21.
Bradley JS, Byington CL, Shah SS, et al; Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. The management of community-acquired pneumonia in infants and children older than 3 months of age: Clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:e25–76.
Islam S, Calkins CM, Goldin AB, et al; APSA Outcomes and Clinical Trials Committee, 2011–2012. The diagnosis and management of empyema in children: A comprehensive review from the APSA Outcomes and Clinical Trials Committee. J Pediatr Surg. 2012;47:2101–10.
Havelock T, Teoh R, Laws D, Gleeson F; BTS Pleural Disease Guideline Group. Pleural procedures and thoracic ultrasound: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65:ii61–76.
Shovlin CL, Condliffe R, Donaldson JW, Kiely DG, Wort SJ; British Thoracic Society. British Thoracic Society clinical statement on pulmonary arteriovenous malformations. Thorax. 2017;72:1154–63.
Lawler LP, Fishman EK. Arteriovenous malformations and systemic lung supply: Evaluation by multidetector CT and three-dimensional volume rendering. AJR Am J Roentgenol. 2002;178:493–5.
Gorsi U, Bansal A, Jugpal TS, Chaluvashetty SB, Sandhu MS. Endovascular management of massive hemoptysis secondary to systemic collaterals in previously treated pulmonary arteriovenous malformation. Vasc Endovascular Surg. 2019;53:674–8.
Panda A, Bhalla AS, Goyal A. Bronchial artery embolization in hemoptysis: A systematic review. Diagn Interv Radiol. 2017;23:307–17.
Roebuck DJ, Barnacle AM. Haemoptysis and bronchial artery embolization in children. Paediatr Respir Rev. 2008;9:95–104.
Author information
Authors and Affiliations
Contributions
AB, MJ, SBC, AKS, KSS made substantial contributions to the conception of the work, revised it critically for important intellectual content, and approved the version to be published. KSS will act as guarantor for this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhatia, A., Jana, M., Chaluvashetty, S.B. et al. Radiological Imaging in Chest Diseases: Moving Away from Conventional Modes. Indian J Pediatr 90, 798–805 (2023). https://doi.org/10.1007/s12098-023-04615-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-023-04615-8