Abstract
Objectives
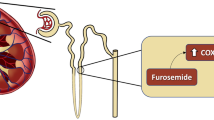
To evaluate the role of cardiopulmonary ultrasonography in the treatment of preterm infants with respiratory failure combined with patent ductus arteriosus (PDA).
Methods
A single-center, prospective, randomized, controlled trial of premature infants born in the authors’ hospital with a birth weight ≤ 1500 g and respiratory failure combined with PDA was conducted from January 2020 to December 2021. The included infants were randomly assigned to the cardiopulmonary ultrasound-guided therapy group or the traditional therapy group. The primary outcome of this study was data on respiratory support and PDA.
Results
A total of 76 premature infants were included in the study. There were 39 patients in the cardiopulmonary ultrasound-guided therapy group and 37 patients in the traditional therapy group. There was no difference in the baseline data, and the cardiopulmonary ultrasound-guided therapy group had a higher initial positive end-expiratory pressure [difference in median = −1.5 cm H2O, 95% confidence interval (CI): −2.0 to −1.0, p < 0.0001], earlier use of ibuprofen to close the PDA (difference in median = 2.5 d, 95% CI: 1.0–4.0, p = 0.004), fewer patients requiring invasive respiratory support [risk ratio (RR) = 0.63, 95% CI: 0.41–0.99, p = 0.04], and a lower incidence of moderate to severe bronchopulmonary dysplasia (RR = 0.44, 95% CI: 0.44–0.96, p = 0.04). There was no difference in the incidence of adverse events.
Conclusions
For premature infants with respiratory failure combined with PDA, cardiopulmonary ultrasonography can better guide respiratory support. The timely administration of drugs helps treat PDA, thereby decreasing the risk of intubation and BPD.
Trial Registration
https://www.trialos.com/index/, TRN: 20220420024607012, date of registration: 2022/03/28, retrospectively registered.


Similar content being viewed by others
References
Zhao M, Huang XM, Niu L, Ni WX, Zhang ZQ. Lung ultrasound score predicts the extravascular lung water content in low-birth-weight neonates with patent ductus arteriosus. Med Sci Monit. 2020;26:e921671.
Yu LF, Xu CK, Zhao M, Niu L, Huang XM, Zhang ZQ. Bedside cardiopulmonary ultrasonography evaluates lung water content in low-weight preterm neonates with patent ductus arteriosus. World J Clin Cases. 2021;9:1827–34.
Tang KQ, Yang SL, Zhang B, et al. Ultrasonic monitoring in the assessment of pulmonary recruitment and the best positive end-expiratory pressure. Med (Baltim). 2017;96:e8168.
Huang D, Ma H, Xiao Z, et al. Diagnostic value of cardiopulmonary ultrasound in elderly patients with acute respiratory distress syndrome. BMC Pulm Med. 2018;18:136.
Liu J, Guo G, Kurepa D, Society of Pediatrics, Asia-Pacific Health Association; the Division of Critical Ultrasound, Pediatric Society of Asia-Pacific Health Association; the Critical Ultrasound Group of Neonatal Specialty, et al. Committee, the Cross-Straits Medicine Exchange Association as well as the World Interactive Network focused on critical Ultrasound China Branch. Specification and Guideline for technical aspects and scanning parameter settings of neonatal lung ultrasound examination. J Matern Fetal Neonatal Med. 2022;35:1003–16.
Su BH, Lin HY, Huang FK, Tsai ML, Huang YT. Circulatory management focusing on preventing intraventricular hemorrhage and pulmonary hemorrhage in preterm infants. Pediatr Neonatol. 2016;57:453–62.
Sweet DG, Carnielli V, Greisen G, et al. European consensus guidelines on the management of respiratory distress syndrome – 2019 update. Neonatology. 2019;115:432–50.
Xiaomei Shao H, Ye. Xiaoshan Qiu. Practice of Neonatology, 5th Ed., Beijing, China: People’s Health Publishing House, 2019. p. 169.
Xiaomei Shao H, Ye. Xiaoshan Qiu. Practice of Neonatology, 5th Ed., Beijing, China: People’s Health Publishing House, 2019. p. 386.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Wang X, Liu D, He H, et al. Using critical care chest ultrasonic examination in emergency consultation: a pilot study. Ultrasound Med Biol. 2015;41:401–6.
Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ. Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med. 2011;183:341–7.
Robba C, Ball L, Battaglini D, et al. Effects of positive end-expiratory pressure on lung ultrasound patterns and their correlation with intracranial pressure in mechanically ventilated brain injured patients. Crit Care. 2022;26:31.
Vignon P, Repessé X, Vieillard-Baron A, Maury E. Critical care ultrasonography in acute respiratory failure. Crit Care. 2016;20:228.
Jain A, Shah PS. Diagnosis, evaluation, and management of patent ductus arteriosus in preterm neonates. JAMA Pediatr. 2015;169:863–72.
Kluckow M, Jeffery M, Gill A, Evans N. A randomised placebo-controlled trial of early treatment of the patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed. 2014;99:F99–104.
Isayama T, Lee SK, Mori R, et al. Canadian neonatal network; neonatal Research Network of Japan. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics. 2012;130:e957–65.
Miyata M, Toyoshima K, Yoda H, et al. Extensive use of vasodilator agents and functional echocardiography to monitor extremely-low-birth-weight infants in Japan. J Neonatal Perinatal Med. 2016;9:261–9.
Isayama T. The clinical management and outcomes of extremely preterm infants in Japan: past, present, and future. Transl Pediatr. 2019;8:199–211.
Sharma A, Xin Y, Chen X, Sood BG. Early prediction of moderate to severe bronchopulmonary dysplasia in extremely premature infants. Pediatr Neonatol. 2020;61:290–9.
Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: a systematic review and meta-analysis. JAMA. 2016;316:611–24.
Wang Xiaoting L, Dawei Yu. Expert consensus on severe ultrasound in China. Chin J Intern Med. 2016;55:900–12.
Funding
This work was supported by the Natural Science Foundation of Zhejiang Province (grant number LY20H040008) and Zhejiang Provincial Medical and Health Technology Project (grant number 2023KY164). The funding source played no role in the study design, data collection, data analysis, data interpretation, writing of the report, or decision to submit the report for publication.
Author information
Authors and Affiliations
Contributions
ZZ and LH developed the study protocol, implemented the study and collected data; MZ helped in interpretation of outcome measurement; XJ and XL helped in protocol development, supervised implementation, and contributed to writing the manuscript; ZZ supervised implementation and critical review of the manuscript. All authors have reviewed the manuscript and approved the submitted version. ZZ will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethical Approval
This study was reviewed and approved by the ethics committee (Ethical lot number: IIT-20220418-0058).
Consent to Participate
Detailed information about the study was given and explained to the participants as well as to their parents who agreed to participate in the study, after which they signed an informed consent and assent form.
Conflict of Interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Lou, X., Hua, L. et al. Cardiopulmonary Ultrasound-Guided Treatment of Premature Infants with Respiratory Failure and Patent Ductus Arteriosus: A Randomized, Controlled Trial. Indian J Pediatr 90, 1103–1109 (2023). https://doi.org/10.1007/s12098-023-04489-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-023-04489-w