Abstract
Objective
To compare SNAPPE-II and STOPS admission severity scores in neonates admitted to neonatal intensive care unit (NICU) with a gestational age of ≥ 33 wk.
Methods
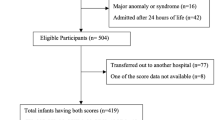
In this multicenter, prospective, observational study, the sickness scoring was done on all the neonates at 12 h after admission to the NICUs. The scoring systems were compared by the area under the curve (AUC) on the receiver operating characteristics (ROC) curve.
Results
A total of 669 neonates with gestational age ≥ 33 wk (mortality rate: 2.4%), who were admitted to five participating NICUs within 24 h of birth, were included. Both SNAPPE-II and STOPS had the good discriminatory and predictive ability for mortality with AUCs of 0.965 [95% confidence interval (CI): 0.94–0.98] and 0.92 (95% CI: 0.87–0.99), respectively. The STOPS scoring system with a cutoff score ≥ 4 on the ROC curve had 85% accuracy, whereas the SNAPPE-II cutoff score ≥ 33 on the ROC curve had 94% accuracy in predicting mortality.
Conclusion
In infants with the gestational age of ≥ 33 wk, SNAPPE-II and STOPS showed similar predictive ability, but the STOPS score, being a simpler clinical tool, might be more useful in resource-limited settings.


Similar content being viewed by others
References
Tarnow-Mordi W, Ogston S, Wilkinson AR, et al. Predicting death from initial disease severity in very low birthweight infants: a method for comparing the performance of neonatal units. BMJ. 1990;300:1611–4.
Parry G, Tucker J, Tarnow-Mordi W. UK Neonatal Staffing Study Collaborative Group. CRIB II: an update of the clinical risk index for babies score. Lancet. 2003;361:1789–91.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II:simplified newborn illness severity and mortality risk scores. J Pediatr. 2001;138:92–100.
Garg B, Sharma D, Farahbakhsh N. Assessment of sickness severity of illness in neonates: review of various neonatal illness scoring systems. J Matern Fetal Neonatal Med. 2018;31:1373–80.
Radfar M, Hashemieh M, Fallahi M, Masihi R. Utilization of SNAP II and SNAPPE II scores for predicting the mortality rate among a cohort of iranian newborns. Arch Iran Med. 2018;21:153–7.
A M, Etika R, Harianto A, Indarso F, Damanik S. The use of score for neonatal acute physiology perinatal extension II (SNAPPE II) in predicting neonatal outcome in neonatal intensive care unit. Paediatrica Indonesiana. 2016;45:241.
Harsha SS, Archana BR. SNAPPE-II (score for neonatal acute physiology with perinatal extension-II) in predicting mortality and morbidity in NICU. J Clin Diagn Res. 2015;9:SC10–2.
Rachuri S, Paul S, M. D. J. SNAPPE II score: predictor of mortality in NICU. Int J Contemp Pediatr. 2019;6:422–6.
Muktan D, Singh RR, Bhatta NK, Shah D. Neonatal mortality risk assessment using SNAPPE-II score in a neonatal intensive care unit. BMC Pediatr. 2019;19:279.
Asker HS, Satar M, Yıldızdaş HY, et al. Evaluation of score for neonatal acute physiology and perinatal extension II and clinical risk index for babies with additional parameters. Pediatr Int. 2016;58:984–7.
Gagliardi L, Cavazza A, Brunelli A, et al. Assessing mortality risk in very low birthweight infants: a comparison of CRIB, CRIB-II, and SNAPPE-II. Arch Dis Child Fetal Neonatal Ed. 2004;89:F419–22.
Sotodate G, Oyama K, Matsumoto A, Konishi Y, Toya Y, Takashimizu N. Predictive ability of neonatal illness severity scores for early death in extremely premature infants. J Matern Fetal Neonatal Med. 2022;35:846–51.
Reid S, Bajuk B, Lui K, Sullivan EA. NSW and ACT neonatal intensive care units audit group, PSN. Comparing CRIB- II and SNAPPE- II as mortality predictors for very preterm infants. J Paediatr Child Health. 2015;51:524–8.
Karaarslan U, Bağ Ö, Özer EA, Helvaci M. Comparison of CRIB II and SNAP-PE-II scoring systems in predicting the mortality and morbidity of Very Low Birth Weight infants. Turk J Pediatr Dis. 2017. https://doi.org/10.12956/tjpd.2017.270.
Özcan B, Kavurt AS, Aydemir Ö, Gençtürk Z, Baş AY, Demirel N. SNAPPE-II and risk of neonatal morbidities in very low birth weight preterm infants. Turk J Pediatr. 2017;59:105–12.
McLeod JS, Menon A, Matusko N, et al. Comparing mortality risk models in VLBW and preterm infants:systematic review and meta-analysis. J Perinatol. 2020;40:695–703.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–43.
Mathur NB, Arora D. Role of TOPS (a simplified assessment of neonatal acute physiology) in predicting mortality in transported neonates. Acta Paediatr. 2007;96:172–5.
Asari US, Shah PA, Jagiwala GP, Patel RM, Kolcha BA, Patel PB. A study of correlation of TOPS Score with outcome of referred neonates. Natl J Commun Med. 2020. https://doi.org/10.5455/njcm.20191219085358.
James J, Kailas L, Nair PMC. Shaji M. Optimizing use of empirical antibiotics in late preterm neonates at risk of early-onset sepsis. Indian J Child Health. 2019;6:189–92.
Rathod D, Adhisivam B, Bhat BV. Sick neonate score-a simple clinical score for predicting mortality of sick neonates in resource restricted settings. Indian J Pediatr. 2016;83:103–6.
Ray S, Mondal R, Chatterjee K, Samanta M, Hazra A, Sabui TK. Extended sick neonate score (ESNS) for clinical assessment and mortality prediction in sick newborns referred to tertiary care. Indian Pediatr. 2019;56:130–3.
Mansoor KP, Ravikiran SR, Kulkarni V, et al. Modified sick neonatal score (MSNS): a novel neonatal disease severity scoring system for resource-limited settings. Crit Care Res Pract. 2019;2019:9059073.
Funding
None.
Author information
Authors and Affiliations
Contributions
VV, SM, VRK: Concept of the study; VV, SM, TPO, BS, BT: Design of study; VV, BT, BS, YAM, S Seth, S Siramshetty, VRK: Data acquisition; VV, SM, SD: Analysis; VV, SM, SD, TPO: Drafting of the work and revising the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work. SM will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethical Approval
IRB approval was obtained for the study and written informed consent was taken from all parents.
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vardhelli, V., Seth, S., Mohammed, Y.A. et al. Comparison of STOPS and SNAPPE-II in Predicting Neonatal Survival at Hospital Discharge: A Prospective, Multicentric, Observational Study. Indian J Pediatr 90, 781–786 (2023). https://doi.org/10.1007/s12098-022-04330-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04330-w