Abstract
Objective
Comparison of mortality and major morbidities between very preterm (< 32 wk gestational age) small-for-gestational-age (SGA) and appropriate-for-gestational-age (AGA) neonates.
Methods
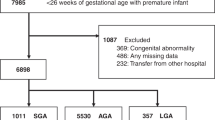
A retrospective observational study of neonates born between 26–31 wk gestational age from January 2015 to December 2019 was done in level-3 neonatal intensive care unit of a high-risk perinatal center in South India.
Results
Of the 1,178 very preterm neonates born in the study period, 909 were eligible for inclusion. After propensity score matching for gestational age, gender, and antenatal steroid use, 592 (444 AGA and 148 SGA) were included in the final analysis. SGA neonates had increased odds of necrotizing enterocolitis (NEC) ≥ stage 2A [adjusted odds ratio (aOR): 2.2; 95% CI: 1.15–4.21], abnormal composite outcome, i.e., any one of the mortality or major morbidities (aOR: 2.99; 95% CI: 1.96–4.57), hypoglycemia requiring intravenous fluids (aOR: 2.11; 95% CI: 1.05–4.23), and anemia requiring blood transfusions (aOR: 3.13; 95% CI: 1.98–4.93); and a trend towards increased odds of bronchopulmonary dysplasia (aOR: 1.9, 95% CI: 0.92–3.91). Mortality, intraventricular hemorrhage ≥ grade 2, periventricular leukomalacia ≥ grade 2, and retinopathy of prematurity requiring treatment were not different.
Conclusions
SGA neonates have higher odds of having NEC ≥ stage 2A, abnormal composite outcome, hypoglycemia, and anemia compared to appropriately grown neonates.

Similar content being viewed by others
Data Availability
On reasonable request.
References
Lee ACC, Katz J, Blencowe H, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1:e26-36.
Malhotra A, Allison BJ, Castillo-Melendez M, Jenkin G, Polglase GR, Miller SL. Neonatal morbidities of fetal growth restriction: pathophysiology and impact. Front Endocrinol. 2019;10:55.
Sacchi C, Marino C, Nosarti C, Vieno A, Visentin S, Simonelli A. Association of intrauterine growth restriction and small for gestational age status with childhood cognitive outcomes: a systematic review and meta–analysis. JAMA Pediatr. 2020;174:772–81.
Priante E, Verlato G, Giordano G, et al. Intrauterine growth restriction: new insight from the metabolomic approach. Metabolites. 2019;9:267.
Mendez-Figueroa H, Truong VTT, Pedroza C, Chauhan SP. Morbidity and mortality in small-for-gestational-age infants: a secondary analysis of nine MFMU network studies. Am J Perinatol. 2017;34:323–32.
Boghossian NS, Geraci M, Edwards EM, Horbar JD. Morbidity and mortality in small for gestational age infants at 22 to 29 weeks’ gestation. Pediatrics. 2018;141:e20172533.
Zeitlin J, El Ayoubi M, Jarreau PH, et al. Impact of fetal growth restriction on mortality and morbidity in a very preterm birth cohort. J Pediatr. 2010;157:733–9.
Grisaru-Granovsky S, Reichman B, Lerner-GevaL,et al. Mortality and morbidity in preterm small-for-gestational-age infants: a population–based study. Am J Obstet Gynecol. 2012;206:150.
Yamakawa T, Itabashi K, Kusuda S. Mortality and morbidity risks vary with birth weight standard deviation score in growth restricted extremely preterm infants. Early Hum Dev. 2016;92:7–11.
Qiu X, Lodha A, Shah PS, et al. Neonatal outcomes of small for gestational age preterm infants in canada. Am J Perinatol. 2012;29:87–94.
Tsai LY, Chen YL, Tsou KI, Mu SC. The Impact of small-for-gestational-age on neonatal outcome among very-low-birth-weight Infants. Pediatr Neonatol. 2015;56:101–7.
Jensen EA, Foglia EE, Dysart KC, et al. Adverse effects of small for gestational age differ by gestational week among very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2019;104:F192–8.
de Costa IT, Leone CR. Intrauterine growth restriction influence on the nutritional evolution and growth of preterm newborns from birth until discharge. Rev Paul Pediatr. 2009;27:15–20.
Giapros V, Drougia A, Krallis N, Theocharis P, Andronikou S. Morbidity and mortality patterns in small-for-gestational age infants born preterm. J Matern Fetal Neonatal Med. 2012;25:153–7.
Marchant T, Willey B, Katz J, et al. Neonatal mortality risk associated with preterm birth in East Africa, adjusted by weight for gestational age: individual participant level meta-analysis. Bhutta ZA, editor. PLoS Med. 2012;9:e1001292.
Ortigosa Rocha C, Bittar RE, Zugaib M. Neonatal outcomes of late-preterm birth associated or not with intrauterine growth restriction. Obstet Gynecol Int. 2010;2010:231842.
Tannirwar S, Kadam S, Pandit A, Vaidya U, Parikh T, Ankit S. Comparisons of mortality and pre-discharge respiratory morbidities in small for gestational age and appropriate-for gestational age premature infants - an Indian Experience. Iran J Neonatol IJN. 2016;7:1–6.
Hasthi UR, Ashwani N, Kumar CS, Chejeti SR. Morbidity and mortality patterns in small for gestational age versus appropriate for gestational age preterm neonates admitted in level II neonatal intensive care unit: A Observational Study. Int J Sci Study. 2017;4:133–6.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Tita ATN, Andrews WW. Diagnosis and management of clinical chorioamnionitis. Clin Perinatol. 2010;37:339–54.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Sehgal A, McNamara PJ. Does echocardiography facilitate determination of hemodynamic significance attributable to the ductus arteriosus? Eur J Pediatr. 2009;168:907–14.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33:179–201.
de Vries LS, Eken P, Dubowitz LM. The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res. 1992;49:1–6.
Inder TE, Perlman JM, Volpe JJ. Intraventricularhemorrhage and post hemorrhagic hydrocephalus. In: Joseph J Volpe, Editor. Volpe Neurology of Newborn. Philadelphia, PA: Elsevier; 2018. pp. 425–57
Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol Chic Ill. 1960;2003:1684–94.
Committee on Fetus and Newborn, Adamkin DH. Postnatal glucose homeostasis in late–preterm and term infants. Pediatrics. 2011;127:575–9.
New HV, Berryman J, Bolton-Maggs PH, et al. Guidelines on transfusion for fetuses, neonates and older children. Br J Haematol. 2016;175:784–828.
RStudio Team. RStudio: Integrated Development for R. In:RStudio PBC Boston MA. 2020. Available at: http://www.rstudio.com/. Accessed on 25 June 2020.
Author information
Authors and Affiliations
Contributions
RPA conceptualized the study, supervised data collection, and prepared manuscript. VV, VRK, and PRV collected the data, helped in manuscript preparation, and reviewed the final manuscript. TPO, SM, and SD supervised the data collection, analysis, and gave important inputs to the final manuscript. GMMR checked authenticity of data, did propensity score match, and reviewed the final manuscript. RPA will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethics Approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethics Committee of Fernandez hospitals approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anne, R.P., Vardhelli, V., Oleti, T.P. et al. Propensity-Matched Comparison of Very Preterm Small- and Appropriate-for-Gestational-Age Neonates. Indian J Pediatr 89, 59–66 (2022). https://doi.org/10.1007/s12098-021-03878-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-021-03878-3