Abstract
Objective
To investigate right and left cerebral tissue (ctSO2) and renal tissue oxygenations (rtSO2) in otherwise healthy children.
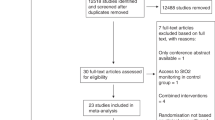
Methods
In this observational cross-sectional study, one hundred children seen as outpatients for well child care or common non-critical complaints, were included. Bilateral ctSO2 and rtSO2 were recorded simultaneously with INVOS™ 5100 device.
Results
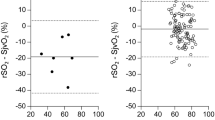
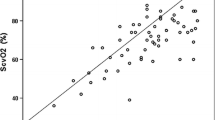
The median age was 6.7 y (IQR 3–10.4) and median weight was 21 kg (IQR 13–33). Right and left sided ctSO2 and rtSO2 values were 78.7% ± 6.0% and 79.1% ± 5.7%; 81.5% ± 9.4% and 81.4% ± 9.5% respectively. There were no differences in right and left cerebral and renal near infrared spectroscopy (NIRS) values, and no age centered lateralization effect. Renal measurements were higher than cerebral counterparts in 63% of the children. Interaction between age and regional oxygenation was significant. For both sides, renal oxygenation was higher than that of cerebrum in older children, whereas the opposite held true with younger age.
Conclusions
There are no right and left side differences in ctSO2 and rtSO2 values in otherwise healthy children. On the other hand, there seem to be differences between cerebral and renal regions with a significant age effect. Acknowledging its limitations, this study sheds light on laterality and cranial and renal NIRS measurements in otherwise healthy children, and may contribute to the interpretation of NIRS data in critically ill patients.


Similar content being viewed by others
References
Jöbsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198:1264–7.
Samraj RS, Nicolas L. Near infrared spectroscopy (NIRS) derived tissue oxygenation in critical illness. Clin Invest Med. 2015;38:E285–95.
Dix LML, van Bel F, Lemmers PMA. Monitoring cerebral oxygenation in neonates: an update. Font Pediatr. 2017;5:46.
Hirsch JC, Charpie JR, Ohye RG, Gurney JG. Near-infrared spectroscopy: what we know and what we need to know — a systematic review of the congenital heart disease literature. J Thorac Cardiovasc Surg. 2009;137:154–9, e1-12.
Kurth CD, Steven JL, Montenegro LM, et al. Cerebral oxygen saturation before congenital heart surgery. Ann Thorac Surg. 2001;72:187–92.
Thavasothy M, Broadhead M, Elwell C, Peters M, Smith M. A comparison of cerebral oxygenation as measured by the NIRO 300 and the INVOS 5100 near-infrared spectrophotometers. Anaesthesia. 2002;57:999–1006.
Bernal NP, Hoffman GM, Ghanayem NS, Arca MJ. Cerebral and somatic near-infrared spectroscopy in normal newborns. J Pediatr Surg. 2010;45:1306–10.
Dix LM, Van Bel F, Baerts W, Lemmers PM. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr Res. 2013;74:557–63.
Dullenkopf A, Frey B, Baenziger O, Gerber A, Weiss M. Measurement of cerebral oxygenation state in anaesthetized children using the INVOS 5100 cerebral oximeter. Pediatr Anesth. 2003;13:384–91.
Kussman BD, Laussen PC, Benni PB, McGowan FX Jr, McElhinney DB. Cerebral oxygen saturation in children with congenital heart disease and chronic hypoxemia. Anesth Analg. 2017;125:234–40.
Kussman BD, Wypij D, DiNardo JA, et al. An evaluation of bilateral monitoring of cerebral oxygen saturation during pediatric cardiac surgery. Anesth Analg. 2005;101:1294–300.
Lemmers PM, van Bel F. Left-to-right differences of regional cerebral oxygen saturation and oxygen extraction in preterm infants during the first days of life. Pediatr Res. 2009;65:226–30.
Abramo TJ, Zhou C, Estrada C, et al. Cerebral regional oxygen saturation monitoring in pediatric malfunctioning shunt patients. Am J Emerg Med. 2013;31:365–74.
Schneider BA, Avivi-Reich M, Mozuraitis M. A cautionary note on the use of the analysis of covariance (ANCOVA) in classification designs with and without within-subject factors. Front Psychol. 2015;6:474.
McNeill S, Gatenby J, McElroy S, Engelhardt B. Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J Perinatol. 2011;31:51–7.
Hyttel-Sorensen S, Pellicer A, Alderliesten T, et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase II randomised clinical trial. BMJ. 2015;350:g7635.
Lemmers PM, Toet M, van Schelven LJ, van Bel F. Cerebral oxygenation and cerebral oxygen extraction in the preterm infant: the impact of respiratory distress syndrome. Exp Brain Res. 2006;173:458–67.
Moran M, Miletin J, Pichova K, Dempsey EM. Cerebral tissue oxygenation index and superior vena cava blood flow in the very low birth weight infant. Acta Paediatr. 2009;98:43–6.
Alderliesten T, Dix L, Baerts W, Caicedo A, van Huffel S. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr Res. 2015;79:55–64.
Pichler G, Binder C, Avian A, Beckenbach E, Schmölzer GM, Urlesberger B. Reference ranges for regional cerebral tissue oxygen saturation and fractional oxygen extraction in neonates during immediate transition after birth. J Pediatr. 2013;163:1558–63.
Almaazmi M, Schmid MB, Havers S, et al. Cerebral near-infrared spectroscopy during transition of healthy term newborns. Neonatology. 2013;103:246–51.
Baik N, Urlesberger B, Schwaberger B, et al. Reference ranges for cerebral tissue oxygen saturation index in term neonates during immediate neonatal transition after birth. Neonatology. 2015;108:283–6.
Bailey SM, Hendricks-Munoz KD, Mally P. Cerebral, renal, and splanchnic tissue oxygen saturation values in healthy term newborns. Am J Perinatol. 2014;31:339–44.
Urlesberger B, Kratky E, Rehak T, et al. Regional oxygen saturation of the brain during birth transition of term infants: comparison between elective cesarean and vaginal deliveries. J Pediatr. 2011;159:404–8.
Schneider A, Minnich B, Hofstätter E, Weisser C, Hattinger-Jürgenssen E, Wald M. Comparison of four near-infrared spectroscopy devices shows that they are only suitable for monitoring cerebral oxygenation trends in preterm infants. Acta Paediatr. 2014;103:934–8.
Cho H, Nemoto EM, Sanders M, Fernandez K, Yonas H. Comparison of two commercially available near-infrared spectroscopy instruments for cerebral oximetry. J Neurosurg. 2000;93:351–4.
Yoshitani K, Kawaguchi M, Tatsumi K, Kitaguchi K, Furuya H. A comparison of the INVOS 4100 and the NIRO 300 near-infrared spectrophotometers. Anesth Analg. 2002;94:586–90.
Tweddell JS, Ghanayem NS, Hoffman GM. Pro: NIRS is ‘standard of care’ for postoperative management. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2010;13:44–50.
Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103:i3–13.
Moerman A, Meert F, De Hert S. Cerebral near-infrared spectroscopy in the care of patients during cardiological procedures: a summary of the clinical evidence. J Clin Monit Comput. 2016;30:901–9.
Zacharias DG, Lilly K, Shaw CL, et al. Survey of the clinical assessment and utility of near-infrared cerebral oximetry in cardiac surgery. J Cardiothorac Vasc Anesth. 2014;28:308–16.
Hoskote AU, Tume LN, Trieschmann U, et al. A cross-sectional survey of near-infrared spectroscopy use in pediatric cardiac ICUs in the United Kingdom, Ireland, Italy, and Germany. Pediatr Crit Care Med. 2016;17:36–44.
Ghanayem NS, Hoffman GM. Near infrared spectroscopy as a hemodynamic monitor in critical illness. Pediatr Crit Care Med. 2016;17:S201–6.
Acknowledgements
The authors thank Dr. Esra Akdeniz for detailed statistical analysis of this study and Alp T Ozturk for careful review of the manuscript.
Author information
Authors and Affiliations
Contributions
NYO designed the experiment; BA performed the experiments; NYO, FIG, EU and BA analyzed the data; FIG, EU, BA and NYO did literature search and wrote the paper. Dr. Makbule Nilufer Ozturk, Department of Pediatrics, Division of Pediatric Critical Care, Marmara University Pendik Training and Research Hospital will act as guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
The study is supported via an intramural grant (Marmara University Scientific Project Support BAPKO #SAG-CTUP-100616-0255).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Öztürk, N.Y., Aygün, B., Uyar, E. et al. Comparison of Bilateral Cerebro-Renal Tissue Oxygenations in Healthy Children. Indian J Pediatr 87, 99–104 (2020). https://doi.org/10.1007/s12098-019-03093-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-019-03093-1