Abstract
Objective
To study the etiological spectrum of acute liver failure in infants and young children and to identify clinical and biochemical markers for metabolic liver disease (MLD).
Methods
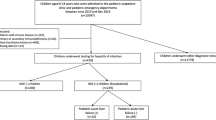
This study was conducted at Department of Pediatric Hepatology, in a tertiary care specialized centre for liver diseases. All children less than 3 y of age, with liver dysfunction and INR ≥2 were included in the study. They were managed as per the departmental protocol. Included children were divided based on the etiology into 2 groups: MLD and non MLD group. Comparison analysis (MLD vs. non MLD) of the clinical and biochemical parameters was done.
Results
There were 30 children under 3 y of age with acute liver failure (ALF) with median age of 12.5 mo. Fifteen children were less than 12 mo. MLD (33 %) and hemophagocytic lymphohistiocytosis (HLH) (17 %) together accounted for half of the cases of ALF in children below 3 y of age. The other common etiologies were drug induced liver injury and acute viral hepatitis A. Etiology remained indeterminate in 3 cases (10 %). Comparative analysis of the clinical and biochemical parameters between MLD and non MLD group showed significant difference between the two groups in the median values of age (p = 0.014), bilirubin (p = 0.017), jaundice to encephalopathy (JE) interval (p = 0.039) and blood sugar (p = 0.001). Suggestive family history (OR 3.73, 95 %CI 1.67–8.30), developmental delay (OR 4.4 95 %CI 2.03–9.51), presence of diarrhea/vomiting (OR 3.28, 95 %CI 1.32–8.13) in the history and presence of urinary non glucose reducing substance (NGRS) (OR 15.5, 95 %CI 2.26–106.87) were also significantly associated with MLD group. Only 40 % children survived with native liver.
Conclusions
MLD and HLH account for majority of ALF in infants. About 10 % of cases remain indeterminate. Viral hepatitis is more common in young children. Apart from clinical indicators, young age, high bilirubin, synthetic dysfunction, low sugar and NGRS in urine indicate MLD as a cause. Survival with native liver is low.


Similar content being viewed by others
References
Squires Jr RH, Shneider BL, Bucuvalas J, Alonso E, Sokol RJ, Narkewicz MR, et al; PALF Study Group. Acute liver failure in children: the first 348 patients in pediatric acute liver failure study group. J Pediatr. 2006;148:652–8.
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31.
Dhawan A. Etiology and prognosis of acute liver failure in children. Liver Transplant. 2008;14:S80–4.
Durand P, Debray D, Mandel R, Baujard C, Branchereau S, Gauthier F, et al. Acute liver failure in infancy: a 14-year experience of a pediatric liver transplantation center. J Pediatr. 2001;139:871–6.
Brett A, Pinto C, Carvalho L, Garcia P, Diogo L, Gonçalves I. Acute liver failure in under two year-olds–are there markers of metabolic disease on admission? Ann Hepatol. 2013;12:791–6.
Kallas M, Cheeseman P, Bhaduri B, Heaton N, Rela M, Mieli-Vergani G. Acute liver failure in infancy. J Pediatr Gastroenterol Nutr. 1997;24:482.
Kaur S, Kumar P, Kumar V, Sarin SK, Kumar A. Etiology and prognostic factors of acute liver failure in children. Indian Pediatr. 2013;50:677–9.
Sundaram SS, Alonso EM, Narkewicz MR, Zhang S, Squires RH; PALF Study Group. Characterization and outcomes of young infants with acute liver failure. J Pediatr. 2011;159:813–8.
Verma A, Dhawan A, Zuckerman M, Hadzic N, Baker AJ, Mieli-Vergani G. Neonatal herpes simplex virus infection presenting as acute liver failure: prevalent role of herpes simplex virus type I. J Pediatr Gastroenterol Nutr. 2006;42:282–6.
Acknowledgments
The authors appreciate the help of the staff of department of Pediatric Hepatology in management of the cases.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alam, S., Lal, B.B., Khanna, R. et al. Acute Liver Failure in Infants and Young Children in a Specialized Pediatric Liver Centre in India. Indian J Pediatr 82, 879–883 (2015). https://doi.org/10.1007/s12098-014-1638-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1638-6